Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(Suppl 1); 2022 > Article
-
Case Report
Repair of traumatic flank hernia with mesh strip suture: a case report -
Shin Ae Lee, M.D.
 , Ye Rim Chang, M.D.
, Ye Rim Chang, M.D.
-
Journal of Trauma and Injury 2022;35(Suppl 1):S46-S52.
DOI: https://doi.org/10.20408/jti.2022.0026
Published online: August 16, 2022
- 2,691 Views
- 69 Download
Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- Correspondence to Ye Rim Chang, M.D. Department of Surgery, Seoul National University College of Medicine, 101 Daehak-ro, Jongno-gu, Seoul 03080, Korea Tel: +82-2-2072-0937 E-mail: yerimchang@gmail.com
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Traumatic flank hernia is a relatively rare hernia. We report a case of a male patient with severe multiple trauma, including abdominal injury, who presented with flank hernia 3 years postinjury. The hernia was successfully repaired using mesh strips suture, and at the 12-month follow-up, no complications or recurrence was found. Our findings indicate that when it is difficult to secure a sufficient operative field for mesh anchoring in a traumatic flank hernia, a technique of sutured repair with mesh strips may be considered as a treatment option as it requires less dissection. Compared to the conventional planar mesh repair, this technique decreases the risk of injuries and ischemic necrosis of the surrounding tissues.
- Flank hernias occurring after blunt abdominal trauma are rare. Approximately 500 cases have been reported in the literature [1–18]. In 2009, the European Hernia Society divided lateral hernia into four zones: L1 (subcostal), L2 (flank), L3 (iliac), and L4 (lumbar) [19]. When the hernia is located lateral to the rectal sheath in the area 3 cm above and below the umbilicus, it is defined as flank hernia [19], which is further divided into primary (spontaneous) and secondary (trauma or surgery), with an incidence of 55% for primary and 25% for secondary flank hernia [20].
- Traumatic flank hernia repair has been reported only in case series; thus, surgical techniques or long-term outcomes have not been established. Kearney et al. [6] reported that primary repair of traumatic flank hernia using mesh strips provides high tension directly to the hernia defect site and has a low recurrence rate due to force distribution at the suture site. In addition, compared to conventional hernia repair, the range of tissue dissection for repair using mesh strips is not wide, so the risk of damage to surrounding structures is low [6]. Moreover, mesh strip technique can be performed easily and quickly.
- In this article, we report a case of a male patient who presented with traumatic flank hernia 3 years postinjury, which was successfully repaired using mesh strips. This is the first reported case of traumatic flank hernia repair using the mesh strip technique in Asia.
- This study was approved by the Institutional Review Board of Seoul National University Hospital (No. 2201-130-1294). Written informed consent was obtained from the patient for publication of this case report and accompanying images.
INTRODUCTION
- A male patient with a history of intrahepatic duct stone surgery was transported to a regional trauma center after he collided with a 15-t truck while driving. His mental status was Glasgow Coma Scale 15, and he complained of severe abdominal pain. The patient was afebrile with a blood pressure of 70/40 mmHg, pulse rate of 68/min, and respiratory rate of 26/min at arrival. Focused assessment of sonography for trauma revealed a large amount of intraabdominal fluid. Shortly, the patient developed severe hypotension, which was unresponsive to resuscitation. Zone 1 resuscitative endovascular balloon occlusion of the aorta was performed, and emergency laparotomy was decided.
- A large amount of hematoma due to massive bleeding from the mesenteric avulsion site and transected vessels was observed after crash laparotomy. Bleeders were controlled, and infarcted small bowel (160 cm length) due to mesenteric avulsion (30 cm length, two sites) was resected. Perforated sigmoid colon was also transected. After 2 days, small bowel anastomosis, S-colon anastomosis, and transverse colostomy were performed during second-look laparotomy.
- Other accompanying injuries (left humerus fracture, multiple rib and sternum fractures, both feet fractures, and multiple transverse spine fractures) were also treated. Two months later, colostomy repair was performed, and the patient was discharged 4 months after trauma.
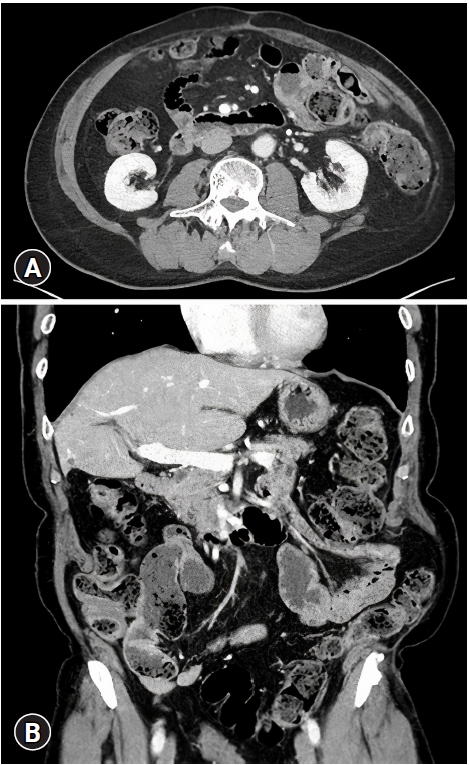
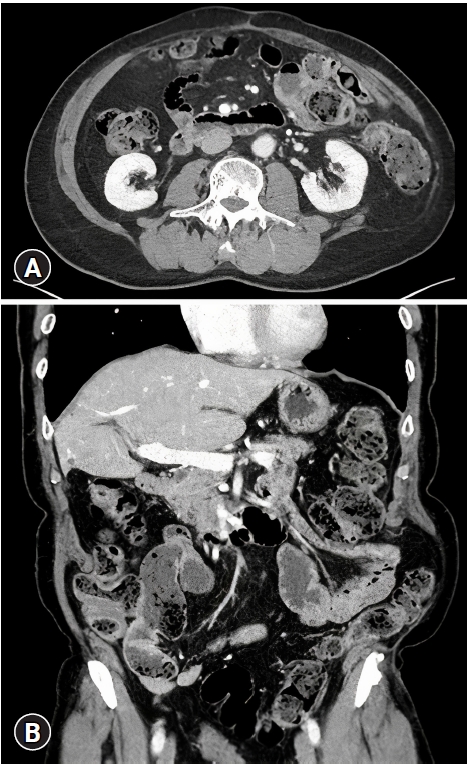
- Three years after injury, the patient newly developed left flank bulging and discomfort (Fig. 1). Computed tomography revealed abdominal wall defect and bowel herniation sized 5.6×11.6 cm above the iliac crest without signs of bowel incarceration (Fig. 2). Repair of traumatic flank hernia with mesh strip suture was planned.
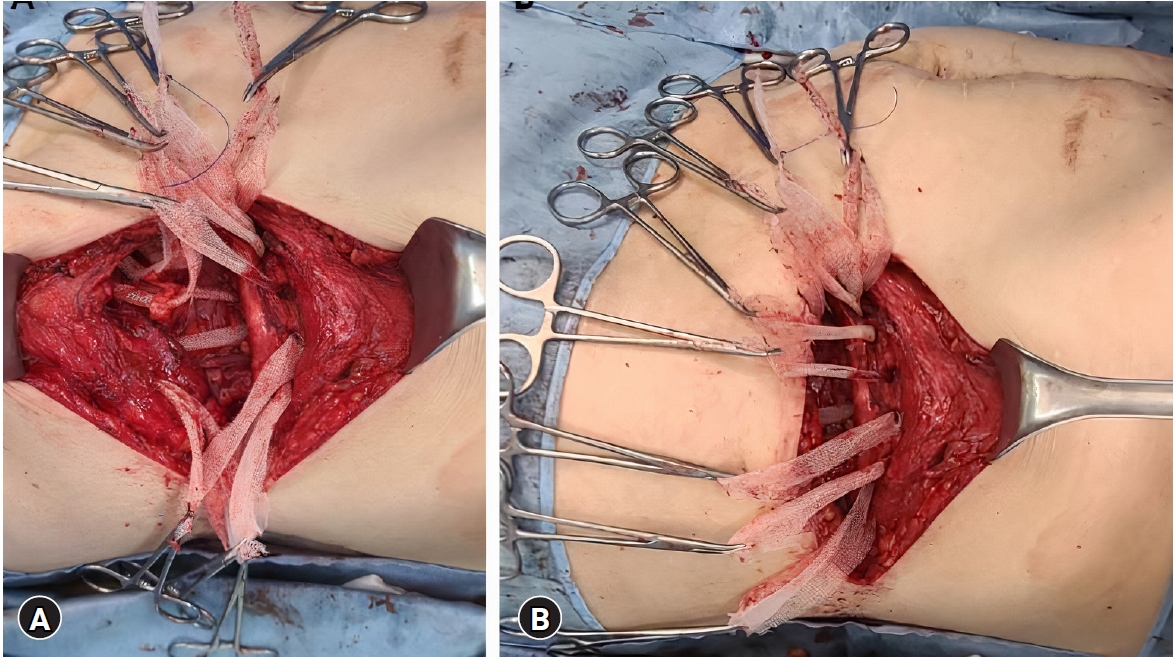
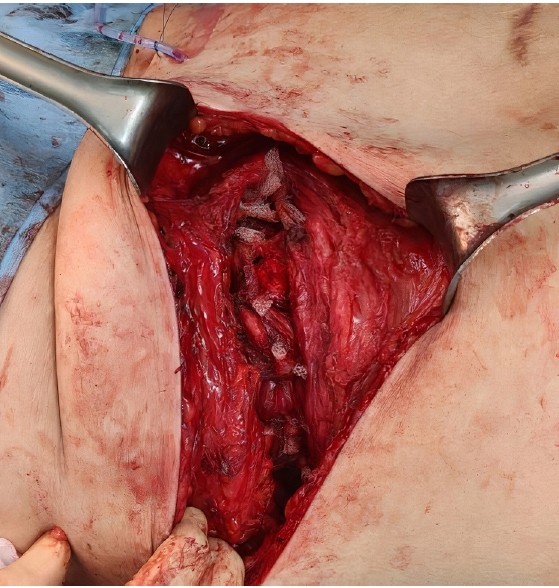
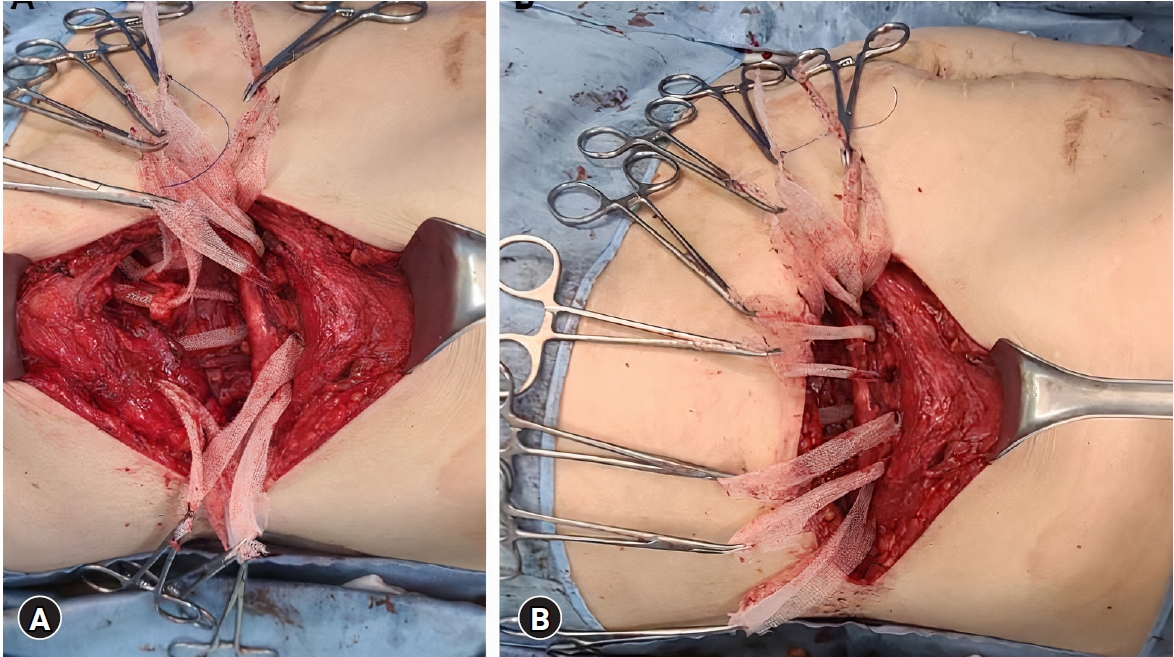
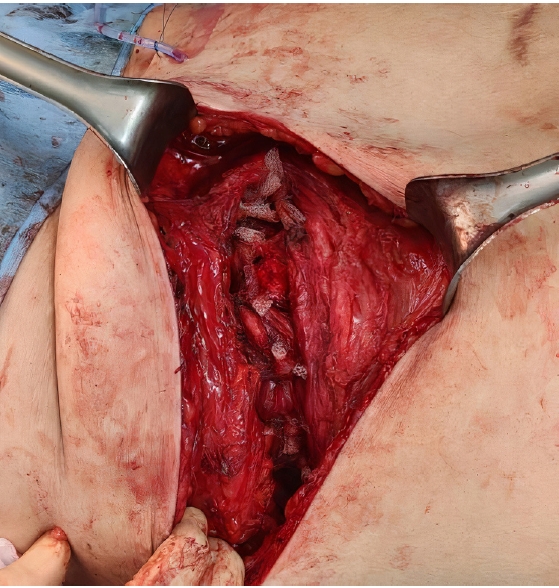
- The patient was placed in a right lateral decubitus position. A beanbag was placed under the patient, and negative pressure was applied to fix the posture (Fig. 3). The bed was bent to extend the space between the iliac crest and the costal margin. The incision was made in the midportion of the abdominal wall defect. The skin and subcutaneous tissue were dissected until the external oblique muscle was identified. The transversus abdominis muscle edge of the hernia defect was identified to complete the exposure of the defect. After confirming that the peritoneum was intact, monofilament polypropylene mesh (Bard Davol, Warwick, RI, USA) was cut into strips with a width of 2 cm. The end of each mesh was triangulated for easy pull-through. The transversus abdominis muscle was pierced with a sharp hemostat approximately 2 to 3 cm from the newly debrided edge of the transverse abdominis muscle. The mesh strip was then pulled through the muscle and tied like a suture after making the operating table flat. Eight mesh strips were applied with even distance (Figs. 4, 5). After placing the Jackson-Pratt drain over the repaired transversus abdominis muscle, the internal and external oblique muscles were repaired with 1-0 polydioxanone suture. Another Jackson-Pratt drain was placed over the external oblique muscle, and the subcutaneous tissue and skin were closed with 2-0 nylon.
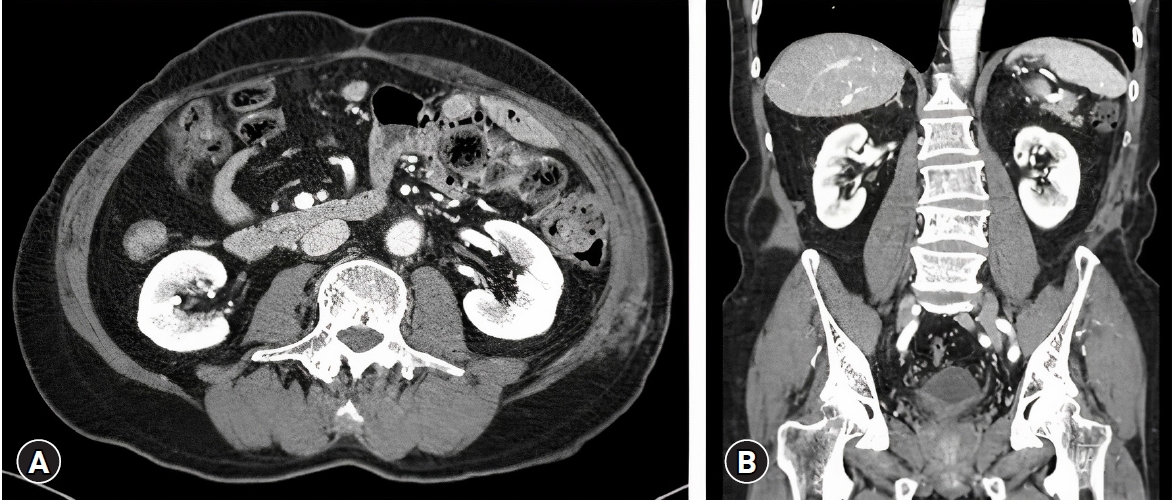
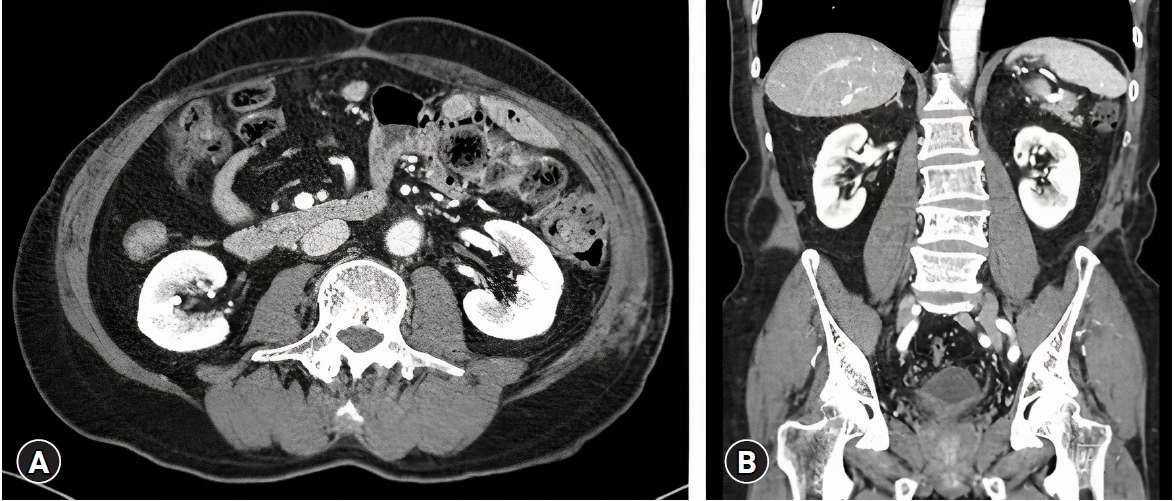
- No evidence of fever and surgical site infection was noted postoperatively. On the 8th postoperative day, the Jackson-Pratt drain was drained to less than 10 mL daily and removed, and the patient was discharged. Computed tomography taken 4 months postoperatively confirmed that the surgical site was intact without recurrence (Fig. 6). No recurrence was observed 12 months postoperatively (Fig. 7). The patient confirmed of having no surgical site discomfort, pain, or foreign body sensation while performing daily activities.
CASE REPORT
- Traumatic flank hernia is a rare hernia, and surgical approach is difficult due to the surrounding bony structures and major neurovascular structures. Conventional methods of flank hernia repair include open, laparoscopic, and robotic approaches or a combination of these approaches. Regarding the repair technique, primary repair or planar mesh reinforcement is usually performed.
- It is recommended that sufficient flap dissection be achieved as wide mesh overlap is imperative. The planar mesh should be covered 5 to 10 cm wider than the size of the hernia defect in both open and laparoscopic approach [4,10–13,15]. For mesh repair using the traditional open technique, the mesh should be anchored to the surrounding muscles or bony prominence, and there is a risk of bleeding or nerve injury [4,10–12,15].
- In the laparoscopic approach, the rate of surgical site infection or recurrence is lower than that in open repair [4]. However, as the laparoscopic approach requires mobilization of the bowel for mesh fixation, there might be a risk of organ injury [4]. Some studies have suggested that the laparoscopic approach to repair flank hernia should be limited to smaller defects [13–15], although data on the mean hernia defect size are limited.
- The most important outcome in hernia repair is the recurrence rate. Table 1 summarizes 18 case series regarding lumbar hernia (including flank hernia) repair targeting a total of 526 patients reported in the literature [1–18]. An open approach was performed in 13 studies, a laparoscopic approach in three studies, a combination of both approaches in one study, and a laparoscopic or robotic approach in one study. The overall recurrence rate of this cohort was 6.1% (0%–13.3%). The causes of lumbar (or flank) hernia recurrence included insufficient mesh overlap or fixation and mesh implantation failure due to infection [10,15,18]. Common complications that occur after hernia repair included seroma, hematoma, and infection [2,7,8,12,13,15,16,18]. Others included skin dehiscence, necrosis, chronic pain, and postoperative anemia due to underlying disease or bleeding during surgery [3–5,11,12,14]. Among them, chronic pain was reported in 0% to 42% of the cases [4,5,11,12,14]. The definition of chronic pain is not clear; therefore, it might have been difficult to differentiate between chronic and postoperative pain [4]. Some studies did not assess chronic pain, which might be a reason for the wide range of prevalence of chronic pain in the cases [2,6,7,10,13,15,18].
- Using the experimental pig model, a study introduced the mesh sutured repair in 2014 and compared it with standard primary suture [21]. That study demonstrated that mesh suture has higher resistance and tensile strength for pull-through than standard primary suture. According to another report on 107 mesh sutured repairs of abdominal wall defects published in 2016 [22], the recurrence rate (early mean follow-up time of 234 days) was <4%, and the incidence of surgical site occurrence (infection, seroma, hematoma, reoperation, delayed wound healing) was 17%. Another study published in 2020 reported that among four patients with traumatic flank hernia who underwent mesh strip repair [6], there were no complications such as surgical site infection, hematoma, or wound breakdown and no recurrence during the mean period of 24.3 months of follow-up. The authors suggested that targeted placement of the mesh at the repair site using strips of mesh distributes the forces of closure across a larger surface area, helping to reduce the likelihood of pull-through with improved outcomes [6]. In addition, mesh suture creates a magnified foreign body response because of its increased surface area [22]. Persistent foreign body response and associated scar formation would be important for the long-term strength of hernia defect closure [22].
- There were two reasons for selecting mesh strips sutured repair for the present case. First, due to the large size of the hernia defect, extensive tissue dissection would have been required for traditional mesh application, which might have increased the risk of postoperative complications. The hernia was located at the L2–L3 boundary according to classification, and it was difficult to secure a sufficient operative field on the inferior border for planar mesh repair. Second, the tension of the surrounding tissue was anticipated to be weak compared to other types of flank hernias. As the patient had very high energy in-car traffic accident, seatbelt might have damaged the fascia and muscles. The injured tissues may have been stretched due to long-standing exposure of intraabdominal pressure and may have progressed to an abdominal wall defect. Since the tension of surrounding tissue was anticipated to be weak, the magnified foreign body response, which is an advantage of the mesh strip suture, would be helpful. Therefore, sutured repair using mesh strips was selected so as to increase the tensile strength of the transversus abdominis muscle with less surrounding tissue dissection.
- In conclusion, when it is difficult to secure a sufficient operative field for mesh anchoring in a traumatic flank hernia, a technique of sutured repair with mesh strips may be considered as a treatment option, given that this technique requires less dissection, thereby reducing the risk of injuries and ischemic necrosis of the surrounding tissue, compared to the conventional planar mesh repair. However, this technique has a limitation that it cannot be applied when there is tissue loss or edges of the hernia cannot be approximated. Further studies are warranted to evaluate the safety and efficacy of the mesh strips suture in traumatic flank hernia repair.
DISCUSSION
-
Ethical statements
This study was approved by the Institutional Review Board of Seoul National University Hospital (No. 2201-130-1294). Written informed consent was obtained from the patient for publication of this case report and accompanying images.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: all authors; Data curation: all authors; Methodology: all authors; Project administration: all authors; Writing–original draft: all authors; Writing–review & editing: all authors.
All authors read and approved the final manuscript.
ARTICLE INFORMATION



| Study | Surgical technique | Repair technique | No. of patients | Mean defect size (cm2) | Mean FU (mo) | Recurrence (%) | Complication (%) |
|---|---|---|---|---|---|---|---|
| Bender et al. [2] | Open | Varied | 25 | NC | 5.7 | 12.0 | 28.0 |
| Edwards et al. [4] | Laparoscopy | Mesh | 27 | 188 | 3.6 | 0 | 0 |
| Fei et al. [5] | Open | Extended sublay, mesh | 18 | NC | 26.2 | 0 | 27.8 |
| Fei et al. [5] | Open | Routine sublay, mesh | 23 | NC | 24.5 | 13.0 | 13.0 |
| Luc et al. [7] | Open | Retromuscular, IPOM | 112 | NCa) | 35.0 | 9.8 | 24.1 |
| Patel et al. [10] | Open | Varied | 6b) | 78.6 | 15.4 | 11.5 | 49.2 |
| Petersen et al. [11] | Open | Sublay, mesh | 4 | NC | 33.0 | 0 | 0 |
| Pezeshk et al. [12] | Open | Varied | 29 | 94 | 21.2 | 3.4 | 31.0 |
| Phillips et al. [13] | Open | Retromuscular, mesh | 16 | 508 | 16.8 | 0 | 31.0 |
| Purnell et al. [14] | Open | Varied, mesh | 31 | NCc) | 27.7 | 9.7 | 6.5 |
| Veyrie et al. [15] | Open | Retromuscular, mesh | 61d) | 56 | 47.0 | 4.9 | 11.5 |
| Zieren et al. [18] | Open | Retromuscular, onlay, mesh | 15 | NCe) | 60.0 | 13.3 | 33.0 |
| Muhkerjee et al. [8] | Open | Mesh | 8 | 90 | 12.0 | 20.0 | 10.0 |
| Novitsky et al. [9] | Laparoscopy | Mesh | 14 | NCf) | 35.0 | 0 | 0 |
| Amaral et al. [1] | Combining laparoscopy and open | Laparoscopic IPOM and open onlay, mesh | 16 | NCg) | 37.0 | 12.5 | 6.3 |
| Cavalli et al. [3] | Open | Retromuscular, mesh | 22 | 232 | 44.8 | 4.5 | 9.1 |
| Zhao et al. [17] | Laparoscopy | TAPE, mesh | 19 | NCh) | 20.0 | 0 | 0 |
| Wijerathne et al. [16] | Laparoscopy, robot | Varied, mesh | 21 | 19.8 | 14.0 | 0 | 18.2 |
| Kearney et al. [6] | Open | Mesh strip | 4 | NC | 24.3 | 0 | 0 |
FU, follow-up; NC, not calculated; IPOM, intraperitoneal onlay mesh; TAPE, transabdominal partially extraperitoneal.
a) Mean width, 8.9±11.7 cm.
b) A total of 61 lumbar hernia patients (subcostal hernia, 14 patients; flank hernia, 33 patients; iliac hernia, 11 patients; lumbar hernia, 3 patients).
c) Mean width, 11.1 cm.
d) A total 61 lateral incisional hernia (subcostal hernia, 14 patients; flank hernia, 12 patients; iliac hernia, 35 patients).
e) Mean size, 15×11 cm.
f) Mean width, 6×9 cm.
g) Mean width, 6.4±2.8 cm.
h) Mean width, 5.8±2.1 cm.
- 1. Amaral PH, Tastaldi L, Barros PH, et al. Combined open and laparoscopic approach for repair of flank hernias: technique description and medium-term outcomes of a single surgeon. Hernia 2019;23:157–65. ArticlePubMedPDF
- 2. Bender JS, Dennis RW, Albrecht RM. Traumatic flank hernias: acute and chronic management. Am J Surg 2008;195:414–7. ArticlePubMed
- 3. Cavalli M, Aiolfi A, Morlacchi A, et al. An extraperitoneal approach for complex flank, iliac, and lumbar hernia. Hernia 2021;25:535–44. ArticlePubMedPDF
- 4. Edwards C, Geiger T, Bartow K, et al. Laparoscopic transperitoneal repair of flank hernias: a retrospective review of 27 patients. Surg Endosc 2009;23:2692–6. ArticlePubMedPDF
- 5. Fei Y, Li L. Comparison of two repairing procedures for abdominal wall reconstruction in patients with flank hernia. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2010;24:1506–9. PubMed
- 6. Kearney AM, Dumanian GA. Simplified repair of traumatic iliac crest flank hernias with mesh strips. Plast Reconstr Surg Glob Open 2020;8:e2970. ArticlePubMedPMC
- 7. Luc G, David A, Couzi L, Midy D, Collet D, Dubuisson V. Lateral incisional hernia after renal transplantation: a comparative study. World J Surg 2014;38:2791–6. ArticlePubMedPDF
- 8. Mukherjee K, Miller RS. Flank hernia repair with suture anchor mesh fixation to the iliac crest. Am Surg 2017;83:284–9. ArticlePubMedPDF
- 9. Novitsky YW. Laparoscopic repair of traumatic flank hernias. Hernia 2018;22:363–9. ArticlePubMedPDF
- 10. Patel PP, Warren JA, Mansour R, Cobb WS 4th, Carbonell AM. A large single-center experience of open lateral abdominal wall hernia repairs. Am Surg 2016;82:608–12. ArticlePubMedPDF
- 11. Petersen S, Schuster F, Steinbach F, Henke G, Hellmich G, Ludwig K. Sublay prosthetic repair for incisional hernia of the flank. J Urol 2002;168:2461–3. ArticlePubMed
- 12. Pezeshk RA, Pulikkottil BJ, Bailey SH, et al. An evidence-based model for the successful treatment of flank and lateral abdominal wall hernias. Plast Reconstr Surg 2015;136:377–85. ArticlePubMed
- 13. Phillips MS, Krpata DM, Blatnik JA, Rosen MJ. Retromuscular preperitoneal repair of flank hernias. J Gastrointest Surg 2012;16:1548–53. ArticlePubMedPDF
- 14. Purnell CA, Park E, Turin SY, Dumanian GA. Postoperative flank defects, hernias, and bulges: a reliable method for repair. Plast Reconstr Surg 2016;137:994–1001. PubMed
- 15. Veyrie N, Poghosyan T, Corigliano N, Canard G, Servajean S, Bouillot JL. Lateral incisional hernia repair by the retromuscular approach with polyester standard mesh: topographic considerations and long-term follow-up of 61 consecutive patients. World J Surg 2013;37:538–44. ArticlePubMedPDF
- 16. Wijerathne S, Malik S, Usmani F, Lomanto D. Minimally invasive repair for lateral ventral hernia: tailored approach from a hernia centre at a tertiary care institution. Hernia 2021;25:399–410. ArticlePubMedPDF
- 17. Zhao Y, Zhang W, Shao X, Cheng T, Li J, Wu L. Transabdominal partial extraperitoneal repair of lateral hernias of the abdomen and flank. J Laparoendosc Adv Surg Tech A 2022;32:653–8. ArticlePubMed
- 18. Zieren J, Menenakos C, Taymoorian K, Muller JM. Flank hernia and bulging after open nephrectomy: mesh repair by flank or median approach? Report of a novel technique. Int Urol Nephrol 2007;39:989–93. ArticlePubMedPDF
- 19. Muysoms FE, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia 2009;13:407–14. ArticlePubMedPMC
- 20. Beffa LR, Margiotta AL, Carbonell AM. Flank and lumbar hernia repair. Surg Clin North Am 2018;98:593–605. ArticlePubMed
- 21. Dumanian GA, Tulaimat A, Dumanian ZP. Experimental study of the characteristics of a novel mesh suture. Br J Surg 2015;102:1285–92. ArticlePubMedPMCPDF
- 22. Lanier ST, Dumanian GA, Jordan SW, Miller KR, Ali NA, Stock SR. Mesh Sutured repairs of abdominal wall defects. Plast Reconstr Surg Glob Open 2016;4:e1060. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Massive traumatic abdominal wall hernia in pediatric multitrauma in Australia: a case report
- Removal of broken syndesmotic screw with minimal bone defects in Korea: a case report
- Endovascular treatment of traumatic iliac venous injury combined with phlegmasia cerulea dolens in Korea: a case report
- Dual repair of traumatic flank hernia using laparoscopic and open approaches: a case report
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite