Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(1); 2022 > Article
-
Case Report
Chronic epidural hematoma evacuated through surgical treatment: a case report -
Eui Gyu Sin, MD

-
Journal of Trauma and Injury 2022;35(1):43-45.
DOI: https://doi.org/10.20408/jti.2021.0036
Published online: February 22, 2022
- 3,024 Views
- 175 Download
- 1 Crossref
Department of Neurosurgery, Konyang University Hospital, Daejeon, Korea
- Correspondence to Eui Gyu Sin, MD Department of Neurosurgery, Konyang University Hospital, 158 Gwanjeodong-ro, Seo-gu, Daejeon 35365, Korea Tel: +82-42-612-2161 E-mail: worser1982@naver.com
• Received: May 3, 2021 • Accepted: June 2, 2021
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Epidural hematoma (EDH) can sometimes be life-threatening, although small-volume EDHs can resolve spontaneously like other intracranial hematomas. However, in rare cases, EDH can transform into a chronic form instead of disappearing. In contrast to subdural hematoma, there is no agreed-upon definition or treatment of chronic EDH. A 41-year-old male patient with acute EDH in the bilateral paravertical area due to partial rupture of the sagittal sinus was operated first, and then remnant contralateral hematoma was treated conservatively. One month after surgery, he showed hemiparesis, and brain imaging revealed chronic EDH at the location of the remnant acute hematoma. We performed surgery again to treat chronic EDH through a large craniotomy. Although many cases of EDH are self-limited, clinicians must keep in mind that some cases of EDH, especially those of venous origin and arising in young people, can become chronic and require surgical treatment.
- Epidural hematoma (EDH) in its acute form was first described by Jacobson in 1886 [1]. EDH can be a life-threatening condition; therefore, treatment has focused on its acute form. However, many cases of EDH improve spontaneously, and surgical treatment is only required for a relatively small proportion of acute cases.
- Unlike subdural hematoma (SDH), there is no agreed-upon definition of chronic EDH or an established interval between the trauma and the diagnosis. This may result from the rarity of the condition, which is why most clinicians underestimate the clinical importance of chronic EDH. Herein, we introduce our experience with a successful operation for chronic EDH.
INTRODUCTION
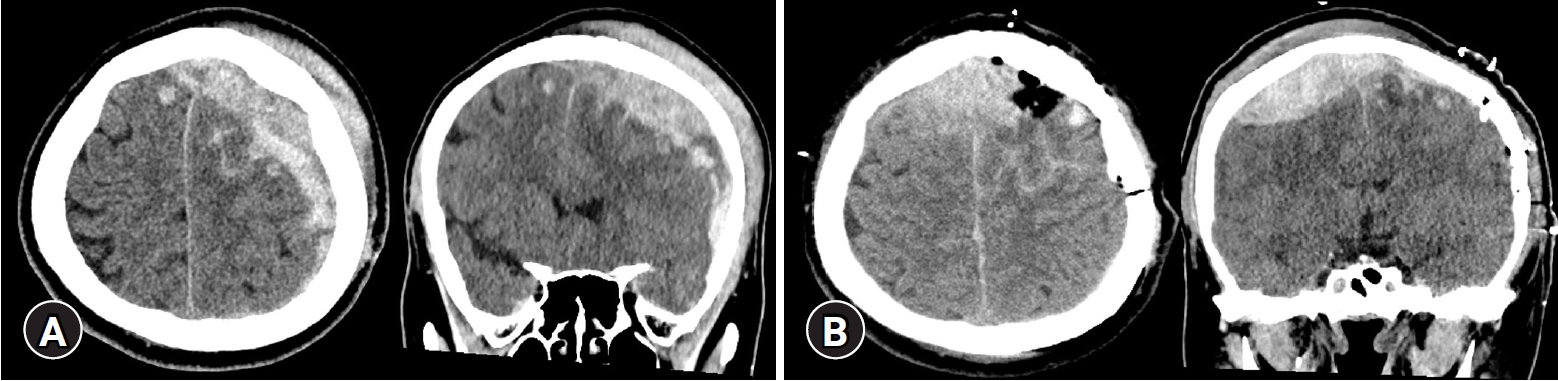
- A 41-year-old male patient presented to Konyang University Hospital due to a fall from height. His consciousness was slightly drowsy and right-side motor power was reduced to grade Ⅲ. The initial brain computed tomography (CT) scan showed left paravertical EDH associated with a linear skull fracture along the sagittal suture line (Fig. 1A). Therefore, we planned an emergent operation. Although a very small portion of the hematoma extended to the right paravertex, we only evacuated the left-side hematoma because his left-side motor function was intact. The bleeding focus was a partial rupture of the superior sagittal sinus due to a skull fracture.
- After surgery, brain CT showed evacuation of the EDH at the left paravertex, but an increased amount of EDH on the contralateral side (Fig. 1B). The patient’s Glasgow Coma Scale improved to 14 from 10, and right hemiparesis also improved. Therefore, we planned conservative treatment for the remnant EDH in the right paravertical area. We expected spontaneous resorption of the hematoma, as commonly occurs with nonsurgical intracranial hematoma.
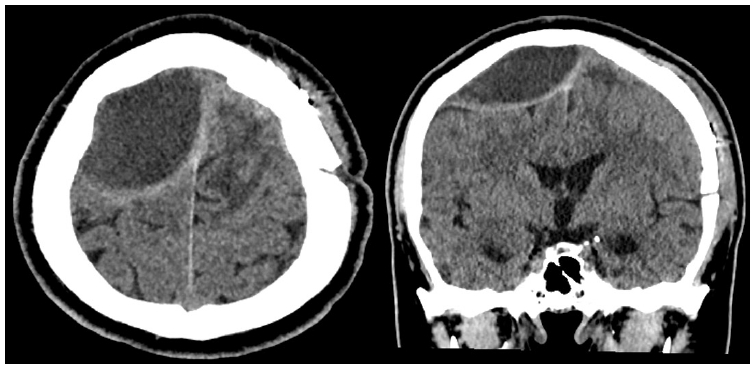
- One month after the operation, the patient’s right hemiparesis had improved fully, but he reported left-side discomfort and paresthesia. We performed another brain CT scan, which showed a hypodense lesion on the right paravertical convexity with expansion of its volume in comparison to the previous CT scan (Fig. 2).
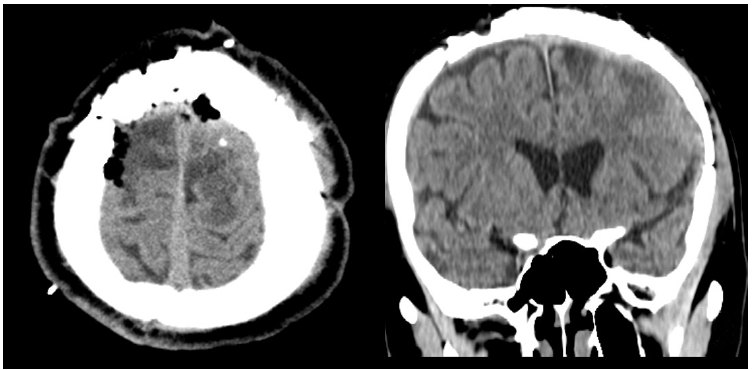
- In light of the amount of time that had passed, we considered that this chronic EDH would not subside spontaneously, so we planned a second operation. The EDH, which consisted of a large amount of organized, solid clots and a small fluid component, was surgically evacuated via a large contralateral craniotomy (Fig. 3). The source of the hemorrhage was not identified during surgery. The patient was discharged 2 weeks after the second operation. No complications and neurological deficits were identified at 6 months after surgery.
CASE REPORT
- EDH occurs as a complication in approximately 1.5% of treated head injuries, and chronic EDH accounts for less than 4% of these cases [2]. Chronic EDH is an unusual and distinctive entity that is not well established, unlike SDH. Some authors refer to chronic EDH as a hematoma observed from 48 hours to 13 days after the incident of trauma or surgery [2,3].
- The pathophysiology of chronic EDH has not been well researched in comparison to chronic SDH. According to Punt [4] in 1978, the process of chronic EDH is similar to that of chronic SDH initiated by stripping of the dura due to trauma or surgery, leading to a small collection at the site that subsequently enlarges due to repeated hemorrhage. A dense fibrous capsule enclosing the hematoma is known to be common [5,6], but did not occur in our case.
- As observed in our case, during its transformation to the chronic form, the hematoma expands. Similar to chronic SDH, processes such as development of a membrane and liquefaction of the solid clot are also seen in chronic EDH [2,7]. The existence of a membrane is important. Neovascular proliferation in the membrane with increased permeability, as well as the hyperfibrinolytic activity of the hematoma, are considered important factors for hematoma development [8]. A dense fibrous capsule forms in response to the products of erythrocyte breakdown, but typical membrane formation as seen in chronic SDH is rare [4–6]. Some authors described this membrane on CT scans as a bright enhanced rim enveloping the hematoma [9]. Our case also showed an enhanced rim. Because the enhanced lesion may be confused with a brain abscess or tumor, it requires attention.
- Chronic EDH is known to be more likely to arise from venous EDH, as in our case, than from a usual arterial EDH [10]. The reason for this is not clear, but we think that a venous EDH may spread out more slowly than an arterial EDH, facilitating the development of a chronic hematoma. It is also more common in younger age groups, as the dura is comparatively less adherent to the inner table of the skull [6].
- Unlike chronic SDH, there is no established theory of the form of internal contents in chronic EDH. Some authors have found “liquefaction” in the cavity, needing only burr hole trephination [9,11]; others have found that the clots were almost always solid even after 1 month [12]. This issue has important implications for surgical treatment. Based on our case, we think that wide craniotomy is preferable to burr hole drainage considering this issue.
- As we all know, the vast majority of EDH cases are self-limited. Therefore, many clinicians have focused on its treatment in the acute phase (e.g., surgical evacuation). However, as our case shows, EDH can transform into a chronic form and provoke a delayed neurologic deficit. Clinicians must keep this point in mind.
DISCUSSION
-
Ethical statement
Informed consent was obtained from the patient.
-
Conflicts of interest
The author has no conflicts of interest to declare.
-
Funding
None.
ARTICLE INFORMATION
Fig. 1.(A) Preoperative brain computed tomography scan. A high-density lentiform shaped hematoma was present mainly on the left paravertical convexity, and a very small amount of hematoma was present on contralateral side. (B) Postoperative brain computed tomography scan. The left paravertical epidural hematoma was removed, but the volume of the right-side hematoma increased along the superior sagittal sinus. The patient provided written informed consent for the publication of the research details and clinical images.


Fig. 2.Brain computed tomography scan 1 month after the first surgery. The right paravertical epidural hematoma had transformed into a chronic epidural hematoma with its increased volume compressing the brain cortex. Capsular enhancement was seen through a non-enhancement computed tomography scan. The patient provided written informed consent for the publication of the research details and clinical images.
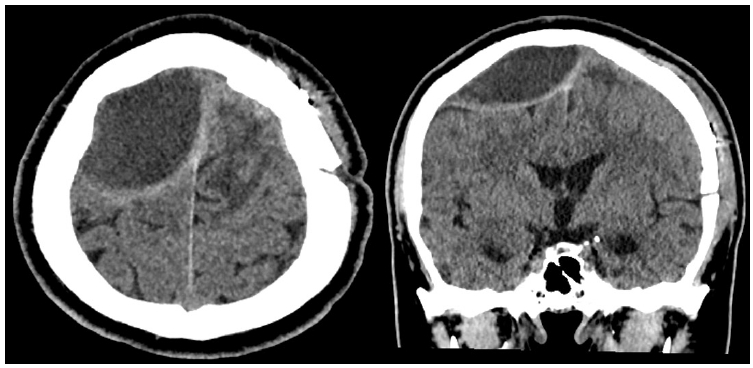
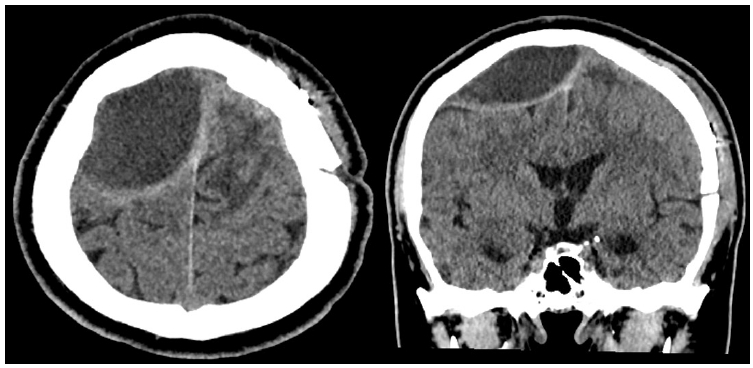
Fig. 3.Postoperative brain computed tomography scan. The right chronic epidural hematoma had been fully removed via craniotomy. The patient provided written informed consent for the publication of the research details and clinical images.


- 1. Jacobson WH. On middle meningeal haemorrhage. Guys Hosp Rep 1886;43:147–308.
- 2. Zuccarello M, Fiore DL, Pardatscher K, Trincia G, Andrioli GC. Chronic extradural haematomas. Acta Neurochir (Wien) 1983;67:57–66. ArticlePubMed
- 3. Iwakuma T, Brunngraber CV. Chronic extradural hematomas: a study of 21 cases. J Neurosurg 1973;38:488–93. ArticlePubMed
- 4. Punt J. Chronic extradural hematoma presenting 33 years after penetrating cranial trauma: case report. J Neurosurg 1978;49:103–6. ArticlePubMed
- 5. Jackson IJ, Speakman TJ. Chronic extradural hematoma. J Neurosurg 1950;7:444–7. ArticlePubMed
- 6. Sparacio RR, Khatib R, Chiu J, Cook AW. Chronic epidural hematoma. J Trauma 1972;12:435–9. ArticlePubMed
- 7. Masuzawa H, Sato J, Kamitani H, Miyake H, Ishiko T, Yoshimasu N. Membrane formation in epidural and subperiosteal hematomas: relationship with the neomembrane of chronic subdural hematomas. Neurol Med Chir (Tokyo) 1982;22:995–1001. ArticlePubMed
- 8. Ito H, Komai T, Yamamoto S. Fibrinolytic enzyme in the lining walls of chronic subdural hematoma. J Neurosurg 1978;48:197–200. ArticlePubMed
- 9. Watanabe T, Nakahara K, Miki Y, Shibui S, Takakura K, Nomura K. Chronic expanding epidural haematoma: case report. Acta Neurochir (Wien) 1995;132:150–3. ArticlePubMed
- 10. Mathuriya SN, Kak VK, Banerjee AK. Ossified epidural haematoma: report of two cases. Clin Neurol Neurosurg 1989;91:269–72. ArticlePubMed
- 11. Kaufman HH, Herschberger J, Kopitnik T, McAllister P, Hogg J, Conner T. Chronic extradural haematomas: indications for surgery. Br J Neurosurg 1992;6:359–64. ArticlePubMed
- 12. Pozzati E, Staffa G, Nuzzo G, Frank F. Late recurrence of bleeding in a chronic extradural hematoma. J Trauma 1987;27:579–80. ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Chronic epidural hematoma: a systematic review and meta-analysis
Nicaise Kpègnon Agada, Nourou Dine Adeniran Bankole, Mèhomè Wilfried Dossou, Omar Boladji Adébayo Badirou, Emeka Alfred Clement, Fresnel Lutèce Ontsi Obame, Laté Dzidoula Lawson, Romeo Bujiriri Murhega, Arsène Daniel Nyalundja, Nukunté David Lionel Togben
Egyptian Journal of Neurosurgery.2023;[Epub] CrossRef
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite