Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Original Article
Traumatic degloving injuries: a prospective study to assess injury patterns, management, and outcomes at a single center in northern India -
Divij Jayant, MS1
 , Atul Parashar, MS2
, Atul Parashar, MS2 , Ramesh Sharma, MS2
, Ramesh Sharma, MS2
-
Journal of Trauma and Injury 2023;36(4):385-392.
DOI: https://doi.org/10.20408/jti.2023.0032
Published online: November 17, 2023
- 836 Views
- 38 Download
1Department of General Surgery, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
2Department of Plastic Surgery, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
- Correspondence to Atul Parashar, MS Department of Plastic Surgery, Postgraduate Institute of Medical Education and Research (PGIMER), Madhya Marg, Sector 12, Chandigarh 160012, India Tel: +91-987-620-1422 Email: atulparashar@hotmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- This study investigated the epidemiology, management, outcomes, and postoperative disabilities of degloving soft tissue injuries (DSTIs) treated at a tertiary care center in northern India.
-
Methods
- A prospective study of patients with DSTIs was conducted over 15 months. The type of degloving injury, the mechanism of injury, and any associated injuries were analyzed using the World Health Organization Disability Assessment Schedule (WHODAS) 2.0 along with the management, outcomes, and disabilities at a 3-month follow-up.
-
Results
- Among 75 patients with DSTIs, the average age was 27.5 years, 80.0% were male, and 76.0% had been injured in traffic accidents. The majority (93.3%) were open degloving injuries. Lower limbs were affected most often (62.7%), followed by upper limbs (32.0%). Fractures were the most commonly associated injuries (72.0%). Most patients required more than two procedures, including secondary debridement (41.3%), split skin grafting (80.0%), flap coverage (12.0%), or vacuum-assisted closure (24.0%), while five patients underwent conservative management for closed degloving injuries. Postoperative complications included surgical site infections (14.7%) and skin necrosis (10.7%). Two patients died due to septic shock and multiple organ dysfunction syndrome. The mean length of hospital stay was 11.5±8.1 days, with injuries affecting the lower limbs and perineum requiring longer hospital stays. The mean WHODAS 2.0 disability score at 3 months was 19. Most patients had mild disabilities. Time away from work depended largely upon the site and severity of the injury. Approximately 75% of patients resumed their previous job or study, 14% changed their job, and 8% stopped working completely due to residual disability.
-
Conclusions
- DSTIs are common injuries in trauma and management is challenging. Although open DSTI are clinically evident at secondary survey, closed degloving injuries may be missed in the primary survey, necessitating a high index of suspicion, thorough clinical examination, and protocol-based management. Primary preventive strategies (e.g., road safety protocols, preplacement training, and proper protective equipment in industries) are also needed to reduce the incidence of these injuries.
- Background
- Degloving soft tissue injuries (DSTIs) are characterized by the detachment or avulsion of skin and subcutaneous tissue from the underlying fascia and muscles. These injuries can involve any part of the body, but the lower limbs and trunk are more commonly affected, with a variable amount of injury to soft tissues [1–3]. Degloving injuries can be open or closed and complete or partial. Open partial degloving injuries have a detached skin flap that still covers the underlying structure while, in complete degloving, the underlying structures are exposed. Closed degloving injuries are characterized by detachment of subcutaneous tissue from underlying fascia resulting in a hematoma with an overlying intact skin [1–3]. Degloving injuries are common in northern India. Various cultural and aesthetic factors can contribute to an increased incidence of these injuries such as the religious practices of the Sikh population who wear the pagri (turban), which increases the risk of head injuries and avulsion injuries to the head and face, and the kada (wrist bracelet), which predisposes to degloving injuries involving the hands and wrists. In addition, the practice of wearing multiple rings on one’s fingers predisposes to finger avulsion injuries. DSTIs in industrial workplaces are primarily caused by conveyor belts and occasionally by roller machines. Recognizing such injuries is essential since delayed diagnosis of closed degloving can lead to subsequent secondary infection [4]. DSTIs are associated with high-velocity injuries and have a high risk of contamination that can develop into a secondary infection or even necrotizing soft tissue infection if not managed promptly [5]. Clinical diagnostic indicators and well-established guidelines for the management of DSTIs are lacking; thus, prompt recognition is the first crucial step for a favorable outcome. Treatment can vary from conservative management to multidisciplinary surgical intervention, which may include excision of devitalized tissue followed by primary skin closure, skin graft, flap cover, and/or skeletal fixation to restore meaningful function [1]. Differentiating viable tissue from nonviable tissue can be difficult during the initial presentation since tissues with threatened blood supply become ischemic, and necrosis develops over time [5]. Outcomes vary based on the mechanism of injury, impact type, affected site, type of degloving (open or closed, complete or partial), associated injuries, and in certain polytrauma patients, the necessary prioritization of life and limb. Most available literature focuses on the treatment of DSTIs and does not look into injury patterns, outcomes and disabilities after the management of such injuries, and preventive strategies, if any.
- Objectives
- In this study, we prospectively studied DSTIs with respect to mechanism, clinical presentation, management, complications, and outcomes based on disability assessments at 3-month follow-ups.
INTRODUCTION
- Ethics statement
- The study protocol was reviewed and approved by the Institutional Review Board of Postgraduate Institute of Medical Education and Research (PGIMER) (No. INT/IEC/2022/000145). Written informed consent was obtained from all patients. The study was conducted in compliance with the principles of the Declaration of Helsinki
- Study design
- This prospective observational study was conducted at the academic, tertiary care center of PGIMER (Chandigarh, India) over a period of 15 months. DSTIs were defined as the avulsion of soft tissue (skin and subcutaneous tissue) from the underlying fascia and muscles. In open degloving injuries, torn skin might still be attached as a flap, while closed degloving injuries had detachment of subcutaneous tissue from the underlying fascia with intact overlying skin creating a cavity filled with hematoma (Morel-Lavallée lesion). In this study, closed degloving injuries were diagnosed by clinical assessment with or without the use of ultrasonography (USG), computed tomography (CT), or magnetic resonance imaging (MRI). The 75 patients with DSTIs, whose ages ranged from 5 to 60 years, were studied prospectively. Patients who presented to the hospital ≥72 hours after injury or who received primary treatment elsewhere were excluded. On presentation, all patients underwent thorough assessment and resuscitation according to Advanced Trauma Life Support guidelines. We recorded demographic data; circumstances of the injury including date, time, and mode of injury (traffic accident, industrial accident, domestic accident, fall from height, sports injury); site of the injury; and associated injuries. Baseline evaluation of the patient included a medical history documenting any comorbidities, a complete physical examination of the part affected, relevant laboratory tests (blood sugar level, coagulation profile, renal function test, hemogram [hemoglobin, platelets, and total leucocyte count]), and relevant imaging studies (x-ray of the affected part and MRI or CT angiography) if clinically indicated. Most open DSTIs were debrided within 24 hours, followed by reassessment after 48 to 72 hours. The type and number of surgical procedures required were recorded. Postoperative complications and the total length of hospital stay were recorded. Patients were followed up after discharge at 2 weekly intervals for the first month, thereafter at monthly intervals until 3 months. The final outcome and disability were assessed at the 3-month follow-up according to the World Health Organization Disability Assessment Schedule (WHODAS) 2.0 [6].
- Statistical analysis
- Data analysis was done using IBM SPSS ver. 22.0 (IBM Corp) and Microsoft Excel 2010 (Microsoft Corp). Quantitative variables, including blood sugar levels, hemograms, coagulation profiles, renal function tests, and liver function tests were represented as mean±standard deviation or median (interquartile range), as applicable. The normality of continuous data was checked by applying the Kolmogorov-Smirnov test. Qualitative variables such as occupation, sex, mode of injury, and site of injury were represented using the chi-square test. The follow-up of patients, including the baseline status at discharge, and the first, second, and third-month check-up was evaluated using a repeated measures analysis of variance test. For any skewed data, the nonparametric Mann-Whitney test was applied.
METHODS
- Preoperative assessment
- Of the 75 patients, 60 (80.0%) were male and 15 (20.0%) were female, with ages ranging from 5 to 60 years and an average age of 27.5 years. Twenty-nine (38.7%) were students and 23 (30.7%) were manual workers, while the rest were farmers, drivers, painters, electricians, or plumbers. Traffic accidents were responsible for 57 injuries (76.0%), followed by 10 industrial accidents (13.3%), five domestic accidents (6.7%), two falls from a height (2.7%), and one impact from a falling heavy object (1.3%). Seventy patients (93.3%) had open degloving injuries while five (6.7%) had closed degloving injuries. Lower limbs were most commonly affected (n=47, 62%), followed by upper limbs (n=24, 32.0%), head and neck (n=12, 16.0%), perineum (n=11, 14.7%), and torso (n=4, 5.3%), while the rest (n=3, 4.0%) involved the back. Fractures were most commonly associated with the DSTI injury (n=54, 72.0%), followed by amputation of fingers or limbs and cut tendons (n=12, 16.0%), traumatic brain injuries (n=7, 9.3%), and solid or hollow viscus injuries (n=6, 8.0%). All patients with closed degloving injuries had associated closed fractures; three (4.0%) had trochanteric fractures and two (2.7%) had pelvic fractures. Low-impact injuries (causing soft tissue lacerations) were seen in three cases (4.0%), medium-impact injuries (causing avulsion or fracture along with laceration) were seen in 35 (46.7%), and high-impact injuries (severe crush or amputation) were seen in 37 (49.3%). Characteristics of the patients are shown in Table 1.
- Postoperative assessment and follow-up
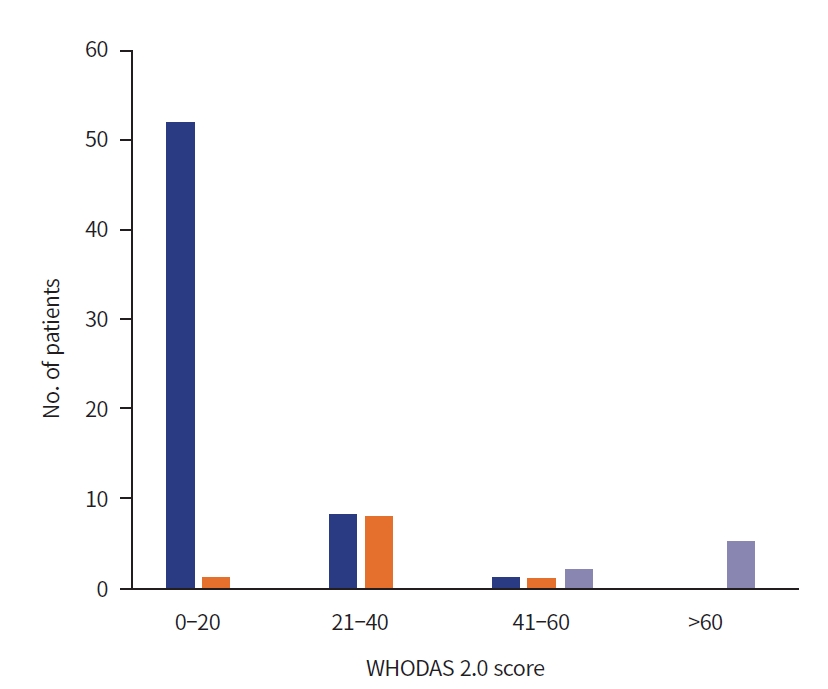
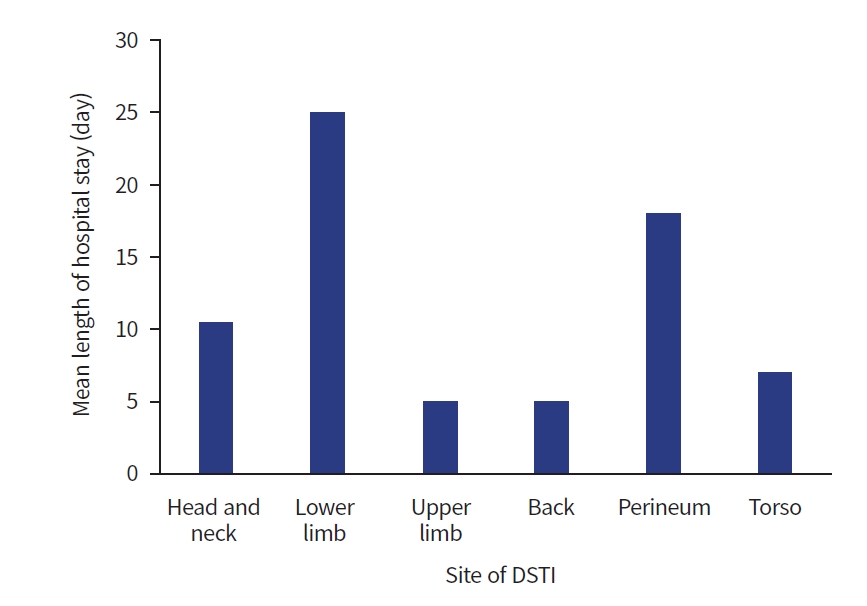
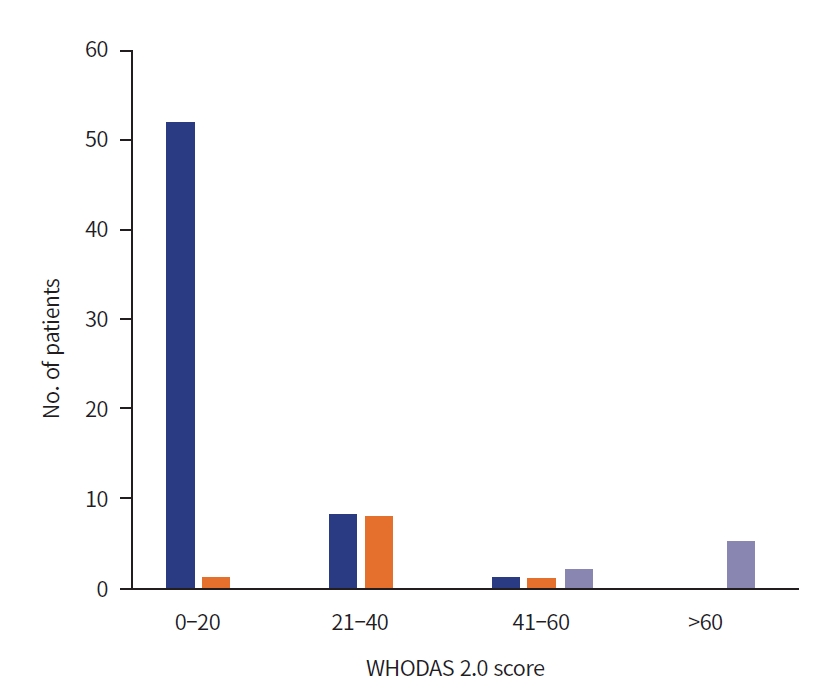
- The treatment received varied according to the type and extent of the degloving and associated injuries (Table 2). All patients were initially resuscitated and subsequently underwent primary debridement. The majority of patients required multiple surgical procedures: secondary debridement in 31 patients (41.3%), split skin grafting (SSG) in 60 patients (80.0%), flap coverage (local or regional) in nine patients (12.0%), revision of amputation in 12 patients (16.0%), tendon repair in four patients (5.3%), and vacuum-assisted closure (VAC) in 18 patients (24.0%); whereas conservative management with repeated hematoma aspirations and compression dressings were performed in five closed degloving injuries (6.7%). Postoperative complications included surgical site infections in 11 patients (14.7%), followed by skin necrosis (n=8, 10.7%), septic shock (n=6, 8.0%), and a combination of skin and flap necrosis (n=5, 6.7%), and two deaths (2.7%) due to septic shock and multiple organ dysfunction syndrome (MODS). Twenty-four patients (32.0%) had no postoperative complications. The mean length of hospital stay was 11.5±8.1 days, which varied according to the site and extent of the DSTI injury and associated injuries. DSTIs affecting the head and neck had an average stay of 10.5 days; lower limbs, 25 days; upper limbs, 5 days; back, 5 days; perineum, 18 days; and injuries affecting the torso, 7 days (Fig. 1). The number of weeks off from work also varied according to the site and severity of the injuries, as well as postoperative complications. Two patients (2.7%) were unable to work for 2 weeks, 15 patients (20.0%) for 2 to 4 weeks, 30 patients (40.0%) for 4 to 8 weeks, 16 patients (21.3%) for 8 to 12 weeks, and five patients (6.7%) for 12 to 24 weeks. After their injury, 56 patients (74.7%) resumed their previous job or study, 11 (14.7%) changed their job, and the remaining six patients (8.0%) stopped working completely due to the severity of their injuries. Residual disability at the 3-month follow-up was calculated using the WHODAS 2.0 (0, no disability; 100, highest disability). With a mean score of 19.7 (range, 3.5–68.5), the majority of patients had mild disability. By correlating the WHODAS 2.0 scores and the number of weeks off from work (Fig. 2), we found that, among 53 patients with mild disability (score, 0–20), 52 (98.1%) resumed their previous job or study, while only one (1.9%) changed their job. Among 16 patients with moderate disability (score, 21–40), eight (50.0%) resumed their previous job or study, while the other eight (50.0%) changed their jobs. Among four patients with severe disability (scores 41–60), only one (25.0%) were able to resume their previous work, while one (25.0%) changed their job, and the other two (50.0%) stopped working completely. All two patients with major disability (score, >60) stopped working completely due to severity of their injuries.
RESULTS
- This single-institution study enrolled 75 patients with DSTIs and studied their demographic details, injury patterns, management, outcomes, and disabilities at a 3-month follow-up. The available literature is largely descriptive with only a few studies reporting on injury patterns and management. No other study has focused on the postoperative disabilities and outcomes in such injuries [7–9]. Furthermore, previous studies have reported on specific anatomical sites and were retrospective. Most were derived from case series [7,9], except one retrospective analysis of 178 DSTI patients in Qatar [8], which studied the patterns and management of degloving injuries. Our center is a major referral center for northern India; thus, the demographic profile of this study was representative of DSTIs in developing countries like India.
- In our study, the mean age of the affected patients was 27.5 years and 80% were male. This corresponds to other studies that also found young men to be commonly affected [7–13]. The higher prevalence of men affected is due to a disproportionately higher proportion of men as drivers, industrial workers, and farmers. Traffic accidents were responsible for 75% of the total injuries with lower limbs mostly affected. These findings are consistent with other studies that showed a higher association between traffic accidents and DSTIs of the lower limbs [8–11]. Patients with DSTIs affecting the head and neck due to traffic accidents did not have a safety helmet at the time of injury. Preplacement training and the use of protective gear in industries play an important role in the prevention of workplace related injuries [12]. Only three patients (20%) with DSTIs due to industrial accidents had preplacement training. Thus, primary preventive strategies such as preplacement training, road safety protocols, and use of protective gear can theoretically eliminate or decrease the incidence of DSTIs.
- DSTIs are serious injuries and often result from high-velocity trauma. The majority of patients in our study had open-type degloving and multiple associated injuries: fractures (72.0%), amputation of fingers or limbs and cut tendon injuries (16.0%), traumatic brain injuries (9.3%), and solid or hollow viscus injuries (8.0%). The presence of fractures, limb amputation, and traumatic brain or abdominal injuries was a surrogate marker for the severity of injury. Although Injury Severity Scores were not calculated in our study, the morbidity and mortality increased with an increase in such associated injuries. Previous studies did not mention associated injuries or the type of DSTI (with one exception [8]), which have a significant impact on treatment planning, outcome, and postoperative disability. Although the number of patients in our study with closed degloving injuries was limited, they were associated with trochanteric and pelvic fractures.
- The incidence of DSTIs is unknown due to a lack of clinical diagnostic criteria, variable severity, and the need to prioritize treatments for a polytrauma patient where saving life and limb takes priority. Closed degloving injuries, however severe they may be, can be missed or dealt with after stabilization of the patient. Defining the severity of injury prior to treatment is important since the viability of an avulsed flap is critical. Viability assessment by clinical inspection and intravenous (IV) fluorescein have been described; however, the efficacy of IV fluorescein in DSTIs is unknown [13–15]. Thus, clinical examination is the most feasible method, however subjective it may be. Skin and soft tissues with bleeding edges and good capillary refill will most likely survive, while discolored tissue with fixed staining that is nonblanchable on digital pressure, and tissues with thrombosed subcutaneous veins require excision [13–15]. Moreover, the diagnosis of closed DSTIs is difficult since the early subtle changes of bruising or hematoma with an intact overlying skin can mask an underlying fluid collection, which if not recognized and managed promptly can lead to life-threatening necrotizing infections [16]. DSTIs can be diagnosed by clinical examination and/or imaging of the affected part if required [16]. Anechoic and hypoechoic lesions on ultrasound, with or without echogenic foci or even fluid, can indicate closed degloving injuries. However, MRI is the modality of choice for diagnosing closed degloving injuries [16,17].
- The management approach for DSTIs following resuscitation and severity assessment can include the preservation of degloved but viable tissue with primary closure, a skin graft with or without VAC, or a flap cover and/or secondary debridement if required [10]. In our center, the majority of open DSTIs are debrided within the first 24 hours, followed by reassessment after 48 to 72 hours. Most can be managed with SSG except for major pelvic and thigh degloving injuries, which require staged tissue reconstruction procedures. In our study, the majority of patients required multiple surgical procedures, including secondary debridement (41.3%), SSG (80.0%), a local or regional flap (12.0%), or VAC (24.0%), whereas 6.7% received conservative management. In a study by Hakim et al. [8], 62.9% of patients were managed with primary debridement, and 19.1% received serial debridement with or without VAC application. Milcheski et al. [9] reported the use of tissue banking for hemodynamically unstable patients, followed by grafting after stabilization. Arnez et al. [10] reported excision of nonviable tissue and flap coverage in two-thirds of patients and skin grafts in 44% of patients. Yan et al. [11] reported incision of the degloved skin with defatting, multiple stab incisions, and securing skin to the recipient bed with sutures. Sakai et al. [18] reported using degloved skin as a full-thickness graft with the use of VAC to secure it. There is reported use of a bilayer dermal regeneration template in DSTIs as well. However, due to the paucity of research, case reports, and analysis of the cost of its use, randomized controlled trials are required to validate its use in the trauma setting [19]. VAC was used in approximately 25% of our patients and showed excellent results as it promotes accelerated granulation tissue and can also be applied over skin grafts [20–22]. In our study, five patients with closed degloving injuries were managed with percutaneous aspiration and compression dressings, which required multiple treatments. A lack of treatment guidelines for closed degloving injuries also makes treatment more challenging. Reported treatment options include observation, compression dressings, percutaneous aspiration, incision and drainage, and debridement [23]. A high incidence of hematoma reaccumulation has been reported after aspiration, and healing by secondary intention is sometimes required [17]. In addition, a higher incidence of concomitant pelvic fractures and traumatic brain injuries increases morbidity and mortality in closed degloving injuries. In our study, the most common postoperative complication was surgical site infection (14.7%), followed by skin necrosis (10.7%). Eight patients presented with septic shock, two of whom died due to refractory septic shock and MODS. One-third of patients in our study had no postoperative complications. A single previous study [8] described a wound infection rate of 3.9% and a skin necrosis rate of 1.1% in patients with DSTI. A higher incidence in our study might be due to differences in the severity and extent of the degloving injuries in the study population.
- In this study, outcomes were evaluated by length of hospital stay and degree of disability. The mean length of hospital stay was 11.5±8.1 days with a maximum of 30 days. Extensive DSTIs with associated injuries that required multidisciplinary and staged management required longer admission. The majority of patients who were managed with SSGs were discharged and managed at primary health centers with regular follow-up in our outpatient clinic. This was done to accommodate new patients, since we receive a large influx of trauma patients as a tertiary care center with limited bed availability. Only two published studies have reported a median length of hospital stay as 10 days [8] and 32.5 days [9]. Reasons for this vast discrepancy might include the characteristics of the study population, a study focused on specific anatomic areas or on extensive degloving injuries, and a retrospective study design.
- This is the only study to assess postmanagement disability in terms of time off from work and WHODAS 2.0 scores. Overall, 40.0% of patients required 4 to 8 weeks off from work, 20.0% were off for 2 to 4 weeks, and 21.3% were off work for 8 to 12 weeks. A single study [11] mentioned time to ambulation, with >75% of patients without long bone fractures ambulating 4 to 6 weeks postoperatively, while injuries associated with fractures took much longer. Disability assessment has not been addressed in previous studies, which might be due to their retrospective nature. The WHODAS 2.0 is used to standardize disability levels and covers six domains of functioning: cognition, mobility, self-care, getting along (interacting with others), daily life activities, and participation in community activities. In our study, disability was calculated at 3 months after the injury, where 0 being no disability and 100 being full disability. The disability scores ranged from a minimum of 3.5 to a maximum of 68.5. The mean score was 19.6 and at 3 months most patients had mild disability. The WHODAS 2.0 scores were correlated with the number of weeks off from work to assess the feasibility and practical application of scoring. Overall, 98.1% of patients with mild disabilities resumed their previous job, while only one changed his job. Half of the patients with moderate disabilities changed their job, while the other half resumed their previous jobs. Half of the patients with severe disabilities stopped working completely, 25.0% changed their jobs, and 25.0% were able to resume their previous work. All patients (100%) with major disabilities stopped working completely.
- Limitations
- There were certain limitations in this study. The study population was limited to a single tertiary care center to which only the most complicated cases requiring multidisciplinary care were referred, and approximately 50 cases of DSTI that had received primary treatment elsewhere were excluded from our study. The Injury Severity Score was not recorded in our study. The time from admission to operative intervention was also not recorded, since polytrauma patients that require a multidisciplinary approach and multiple surgical specialty evaluations may have an increased time to treatment and therefore may have worse outcomes. The viability of the degloved tissue was not recorded in our study and was left to the discretion of the operating surgeon for planning. There was a limited number of patients with closed degloving injuries. There were wide variations in the mechanism of injury, associated injuries, clinical presentation, and treatment options. Therefore, further studies with larger cohorts are required to study closed degloving injuries, since there is a considerable difference between open and closed DSTIs.
- Conclusions
- Degloving injuries are common in a trauma setting and their management is challenging. Some of these injuries may be missed during the primary survey as the ongoing resuscitation of a trauma patient revolves around the most urgent life and limb-threatening injuries. Although CT or MRI can detect degloving injuries, these diagnostic modalities are used for other associated injuries rather than degloving in particular. Thus, DSTIs can be missed with imaging as well. These injuries are often associated with high-velocity trauma and have a high risk of contamination, which contributes to an increased risk of secondary infection and necrotizing soft tissue infection if not diagnosed promptly. Furthermore, differentiating viable from nonviable tissues in partial degloving injuries can be difficult during the initial presentation, as the discoloration and necrosis of detached skin take time to evolve. In our study, most patients were male, and the majority of injuries were due to high-velocity trauma in traffic accidents. Open degloving injuries mostly affected lower limbs and were commonly associated with fractures. Closed degloving injuries were diagnosed clinically and radiologically with MRI, followed by percutaneous aspiration and compression dressings. Injuries affecting lower limbs and the perineum had a longer mean length of hospital stay. Disability at 3 months, as calculated by the WHODAS 2.0, found that a majority had mild disability. Nearly 75% of patients resumed their previous job or study, 14% changed their job, and 8% stopped working completely due to the severity of their injuries. Timely surgical intervention can help reduce postoperative complications and promote early rehabilitation, thereby reducing residual disability. Thus, a high index of suspicion with a multidisciplinary approach, a thorough clinical examination, and timely assessment of the affected part are required for treatment. However, because of the gaps in site-specific and severity-specific treatment guidelines that take into account the variability in degloving injuries, evidence-based guidelines and treatment approaches are needed to improve outcomes. Primary prevention strategies such as proper protective equipment, road safety protocols, and preplacement industrial training can help prevent or decrease the burden of such injuries.
DISCUSSION
-
Author contributions
Conceptualization: DJ, AP; Methodology: AP; Supervision: AP, RS; Validation: AP, RS; Visualization: RS; Writing–original draft: DJ. Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION
| Variable | Value |
|---|---|
| No. of surgical procedures | 2.5±1.0 |
| Treatment received | |
| Primary debridement | 71 (94.7) |
| Secondary or revision debridement | 31 (41.3) |
| Split skin graft | 60 (80.0) |
| Flap cover (local or regional) | 9 (12.0) |
| Revision of amputation | 12 (16.0) |
| Tendon repair | 4 (5.3) |
| Vacuum-assisted closure | 18 (24.0) |
| Conservative management | 5 (6.7) |
| Primary suturing | 1 (1.3) |
| Length of hospital stay (day) | 11.5±8.1 |
| Mean length of hospital stay according to anatomical site of the DSTI (day) | |
| Head and neck | 10.5 |
| Lower limb | 25.0 |
| Upper limb | 5.0 |
| Back | 5.0 |
| Perineum | 18.0 |
| Torso | 7.0 |
| Postoperative complication | |
| Surgical site infection | 11 (14.7) |
| Skin necrosis | 8 (10.7) |
| Skin and flap necrosis | 5 (6.7) |
| Septic shock | 6 (8.0) |
| Death | 2 (2.7) |
| None | 24 (32.0) |
| No. of weeks off work | |
| 2 | 2 (2.7) |
| >2–4 | 15 (20.0) |
| >4–8 | 30 (40.0) |
| >8–12 | 16 (21.3) |
| >12–24 | 5 (6.7) |
| >24 | 7 (9.3) |
| Postinjury work status | |
| Resumed previous job | 56 (74.7) |
| Changed job | 11 (14.7) |
| Stopped working | 6 (8.0) |
| Disabilitya) at 3-mo follow-up | 19.6±15.7 |
| Mild | 53 (70.7) |
| Moderate | 16 (21.3) |
| Severe | 4 (5.3) |
| Major | 2 (2.7) |
Values are presented as mean±standard deviation or number (%)
DSTI, degloving soft tissue injury.
a) Measured using the World Health Organization Disability Assessment Schedule (WHODAS) 2.0 [6].
- 1. Krishnamoorthy R, Karthikeyan G. Degloving injuries of the hand. Indian J Plast Surg 2011;44:227–36.
- 2. Antoniou D, Kyriakidis A, Zaharopoulos A, Moskoklaidis S. Degloving injury: report of two cases and review of the literature. Eur J Trauma 2005;31:593–6. ArticlePubMedPMC
- 3. Wojcicki P, Wojtkiewicz W, Drozdowski P. Severe lower extremities degloving injuries: medical problems and treatment results. Pol Przegl Chir 2011;83:276–82. ArticlePDF
- 4. Yan H, Gao W, Li Z, et al. The management of degloving injury of lower extremities: technical refinement and classification. J Trauma Acute Care Surg 2013;74:604–10. PubMed
- 5. Latifi R, El-Hennawy H, El-Menyar A, et al. The therapeutic challenges of degloving soft-tissue injuries. J Emerg Trauma Shock 2014;7:228–32. PubMed
- 6. Ustun TB, Kostanjsek N, Chatterji S, Rehm J, editors. Measuring health and disability: manual for WHO Disability Assessment Schedule (WHODAS 2.0). World Health Organization; 2010. ArticlePubMedPMC
- 7. Khan M, Aziz A, Naz S, et al. Plastic surgical trauma: a single-centre experience. Indian J Plast Surg 2012;45:538–45. ArticlePubMedPMC
- 8. Hakim S, Ahmed K, El-Menyar A, et al. Patterns and management of degloving injuries: a single national level 1 trauma center experience. World J Emerg Surg 2016;11:35. ArticlePubMedPMC
- 9. Milcheski DA, Ferreira MC, Nakamoto HA, Tuma P, Gemperli R. Degloving injuries of lower extremity: proposal of a treatment protocol. Rev Col Bras Cir 2010;37:199–203. ArticlePubMed
- 10. Arnez ZM, Khan U, Tyler MP. Classification of soft-tissue degloving in limb trauma. J Plast Reconstr Aesthet Surg 2010;63:1865–9. ArticlePubMed
- 11. Yan H, Gao W, Li Z, et al. The management of degloving injury of lower extremities: technical refinement and classification. J Trauma Acute Care Surg 2013;74:604–10. PubMed
- 12. Tarun G, Ramu M. Prevention of industrial accidents: measures and challenges. Int J Pure Appl Math 2018;120:491–8.
- 13. Mandel MA. The management of lower extremity degloving injuries. Ann Plast Surg 1981;6:1–5. ArticlePubMed
- 14. Bloomenstein RB. Viability prediction in pedicle flaps by infrared thermometry. Plast Reconstr Surg 1968;42:252–61. ArticlePubMed
- 15. In: Eccles S, Handley B, Khan U, McFadyen I, Nanchahal J, Nayagam S, editors. Standards for the management of open fractures. Oxford University Press; 2020.
- 16. Latifi R. The diagnostic and therapeutic challenges of degloving soft-tissue injuries. SOJ Surg 2013;1:01. Article
- 17. Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallée lesion. J Trauma 1997;42:1046–51. PubMed
- 18. Sakai G, Suzuki T, Hishikawa T, Shirai Y, Kurozumi T, Shindo M. Primary reattachment of avulsed skin flaps with negative pressure wound therapy in degloving injuries of the lower extremity. Injury 2017;48:137–41. ArticlePubMed
- 19. Alet JM, Weigert R, Castede JC, Casoli V. Management of traumatic soft tissue defects with dermal regeneration template: a prospective study. Injury 2014;45:1042–8. ArticlePubMed
- 20. Meara JG, Guo L, Smith JD, Pribaz JJ, Breuing KH, Orgill DP. Vacuum-assisted closure in the treatment of degloving injuries. Ann Plast Surg 1999;42:589–94. ArticlePubMed
- 21. Wong LK, Nesbit RD, Turner LA, Sargent LA. Management of a circumferential lower extremity degloving injury with the use of vacuum-assisted closure. South Med J 2006;99:628–30. ArticlePubMed
- 22. Dini M, Quercioli F, Mori A, Romano GF, Lee AQ, Agostini T. Vacuum-assisted closure, dermal regeneration template and degloved cryopreserved skin as useful tools in subtotal degloving of the lower limb. Injury 2012;43:957–9. ArticlePubMed
- 23. Nickerson TP, Zielinski MD, Jenkins DH, Schiller HJ. The Mayo Clinic experience with Morel-Lavallée lesions: establishment of a practice management guideline. J Trauma Acute Care Surg 2014;76:493–7. PubMed
- 24. In: Ustun TB, Kostanjsek N, Chatterji S, Rehm J, editors. Measuring health and disability: manual for WHO Disability Assessment Schedule (WHODAS 2.0). World Health Organization 2010;
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite