Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Original Article
Proximally based sural artery flap for the reconstruction of soft tissue defects around the knee and proximal third of the leg in India: a clinical study -
Lakshmi Palukuri, MCh1
 , Sreedharala Srinivas, MCh2
, Sreedharala Srinivas, MCh2 , Dharmapuri Madhulika, MS1
, Dharmapuri Madhulika, MS1 , Sanujit Pawde, MS1
, Sanujit Pawde, MS1 , Ajo Sebastian, MS1
, Ajo Sebastian, MS1 , Swathi Sankar, MS1
, Swathi Sankar, MS1 , Sandeep Reddy Chintha, DNB1
, Sandeep Reddy Chintha, DNB1
-
Journal of Trauma and Injury 2023;36(4):369-375.
DOI: https://doi.org/10.20408/jti.2023.0042
Published online: November 23, 2023
- 887 Views
- 30 Download
- 1 Crossref
1Department of Plastic Surgery, Osmania Medical College and Hospital, Hyderabad, India
2Department of Neurosurgery, Osmania Medical College and Hospital, Hyderabad, India
- Correspondence to Palukuri Lakshmi, MCh Department of Plastic Surgery, Osmania Medical College and Hospital, 5-96/3/A Rd no. 11, Bhavani Nagar, Dilsukh Nagar, Hyderabad 500060, India Tel: +91-40-2460-0146 Email: lakshmipaluku@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- The reconstruction of defects around the knee and the proximal third of the leg necessitates thin, pliable skin with a stable and sensate soft tissue cover. This study analyzed the use of a proximally based sural artery flap for the coverage of such defects.
-
Methods
- This prospective clinical interventional study involved 10 patients who had soft tissue defects over the knee and the proximal third of the leg. These patients underwent reconstruction with a proximally based sural artery flap. The study analyzed various factors including age, sex, etiology, location and presentation of the defect, defect dimensions, flap particulars, postoperative complications, and follow-up.
-
Results
- There were 10 cases, all of which involved men aged 20 to 65 years. The most common cause of injury was trauma resulting from road traffic accidents. The majority of defects were found in the proximal third of the leg, particularly on the anterolateral aspect. Defect dimensions varied from 6×3 to 15×13 cm2, and extensive defects as large as 16 cm × 14 cm could be covered using this flap. The size of the flaps ranged from 7×4 to 16×14 cm2, and the pedicle length was 10 to 15 cm. In all cases, donor site closure was achieved with split skin grafting. This flap consistently provided a thin, pliable, stable, and durable soft tissue cover over the defect with no functional deficit and minimal donor site morbidity. Complications, including distal flap necrosis and donor site graft loss, were observed in two cases.
-
Conclusions
- The proximally based sural fasciocutaneous flap serves as the primary method for reconstructing medium to large soft tissue defects around the knee and the proximal third of the leg. This technique offers thin, reliable, sensate, and stable soft tissue coverage, and can cover larger defects with minimal complications.
- Background
- Injuries that result in soft tissue skin defects around the knee are common, often caused by road traffic accidents. They can also occur secondary to burns, surgical infections, and post–tumor resection. The reconstruction of these defects is challenging due to the need for thin, pliable skin that can restore knee functions [1]. Defects in and around the knee present a significant challenge to reconstructive surgeons due to their location over a mobile joint. This often necessitates stable, pliable tissue with sensation. The skin in this area has less redundancy and a poor arterial supply below the proximal third of the lower leg. Additionally, superficial venous return in this region is frequently ineffective. As a result, soft tissue defects that occur in this region are difficult to cover. To meet these demands, a proximally based sural artery flap appears to be one of the best choices. It is a thin, sensate flap with a good aesthetic appearance and minimal donor site morbidity [2]. This makes it a favorable option compared to other alternatives. However, there are few published reports on this flap.
- Objectives
- The purpose of this study was to evaluate the outcomes of the proximally based sural artery flap when used in the reconstruction of defects around the knee and the proximal third of the leg.
INTRODUCTION
- Ethics statement
- This study was approved by the Institutional Review Board of Osmania General Hospital (No. 20613001002D). Written informed consents for publication of the research details and clinical images were obtained from the patients.
- Study design and patients
- This is a prospective clinical interventional study that was conducted in the Department of Plastic Surgery at Osmania General Hospital (Hyderabad, India), a tertiary care center. The study involved 10 patients who presented with soft tissue defects around the knee or the proximal third of the leg and underwent reconstruction with a proximally based sural artery flap. All the patients were referred from the orthopedic department after the initial stabilization of fractures and any other injuries. The demographic data collected from the patients included age, sex, the mode and etiology of the injury, medicolegal status, any associated fractures, presentation of the defect, addictions, associated comorbid conditions, and complications.
- All patients underwent a routine surgical profile, including a radiograph of the affected limb. This was done to rule out any associated fractures, and if any were found, appropriate management was undertaken. Additionally, a Doppler study of the affected lower limb was conducted to assess the vascular status of the limb.
- After obtaining informed consents about the prognosis of the condition and the planned procedure, patients were included in the study. These patients then underwent preoperative planning for the flap. This involves marking the dimensions of the defect and planning the flap in reverse using a lint cloth, marking pen, and measuring tape.
- Surgical technique
- The following surgical technique was employed [2,3]. Either a standard lateral or prone position was adopted after administering spinal or general anesthesia. Under tourniquet control, meticulous debridement of the recipient site was carried out, and the exact dimensions of the defect were measured. The axis of the flap was drawn along a line that extended from the midpoint of the popliteal fossa to a point midway between the lateral malleolus and the Achilles tendon. Reverse planning was conducted using a lint piece to verify the reach of the flap. The pivot point of the flap was positioned approximately 2 cm from the midpoint of the popliteal fossa along the previously described axis. Preoperative Doppler for assessing flow in the sural artery was not conducted in any of the cases included in this study. Along the distal margin of the flap, the skin and fascia were incised. The sural nerve, associated vascular plexus, and the short saphenous vein were identified and cleanly divided. Dissection was carried out from distal to proximal. The deep fascia was included in the flap at the distal, medial, and lateral sides and was secured with the skin to prevent shearing.
- In the proximal part of the flap, we made only a skin incision. The flap was designed to center the neurovascular bundle. In the upper section, we carefully dissected the sural nerve and the median superficial sural artery between the two heads of the gastrocnemius until we reached the predetermined pivot point (Fig. 1). We included approximately 3 cm of the surrounding soft tissue to safeguard the sural artery pedicle. We then constructed a suitable subcutaneous tunnel to allow the flap and pedicle to reach the recipient site. In some instances, we had to incise the tunnel due to potential pedicle compression. We deflated the tourniquet to verify the flap's viability. The flap was then inset at the recipient site, and a corrugated rubber drain was placed under the flap, which was removed between the 3rd and 5th day.
- The donor area was covered with split skin graft in all cases. A plaster of Paris slab was applied across the knee joint to immobilize it in all patients. Patients were positioned either prone or laterally, with the operated limb elevated.
METHODS
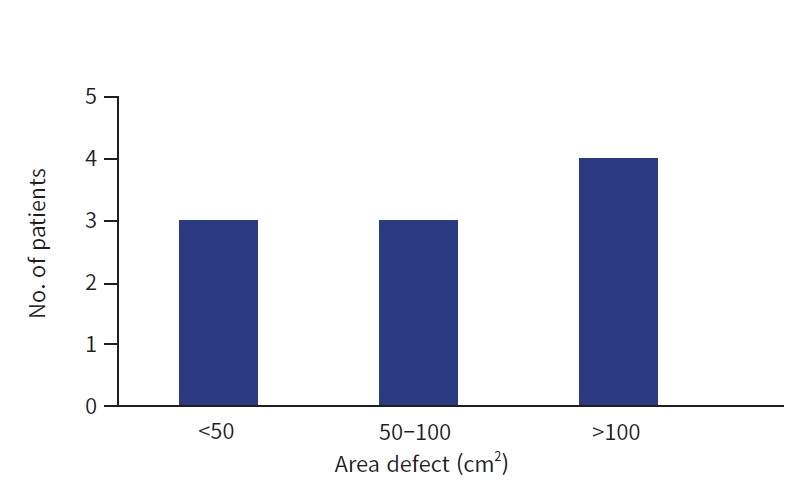
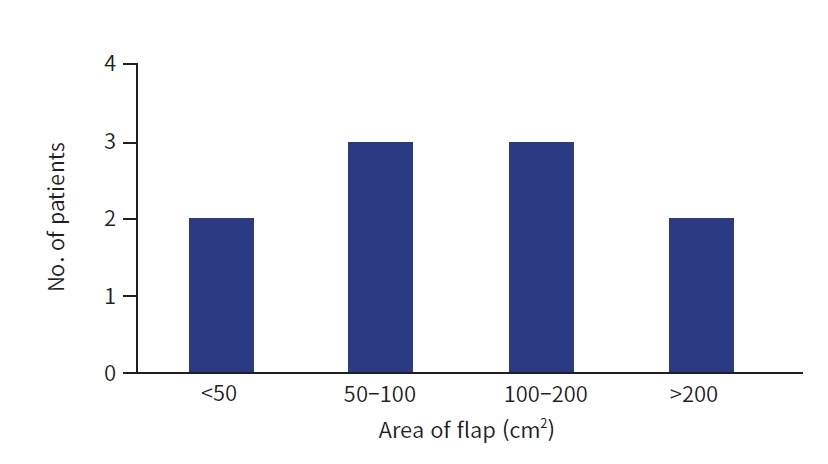
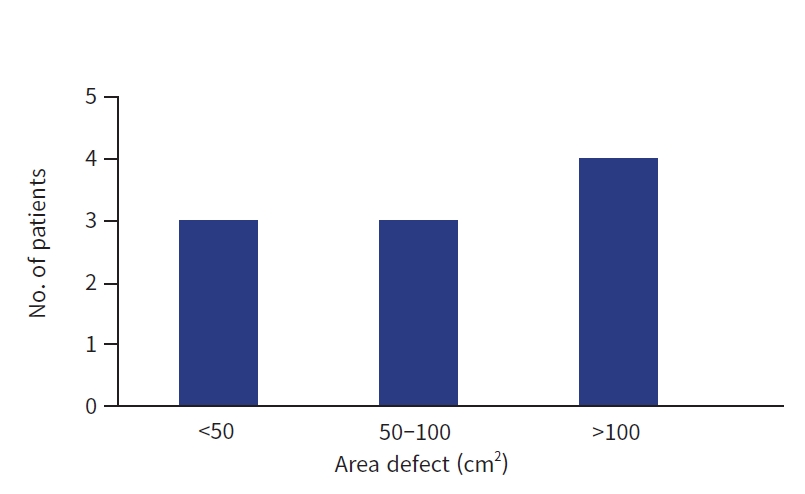
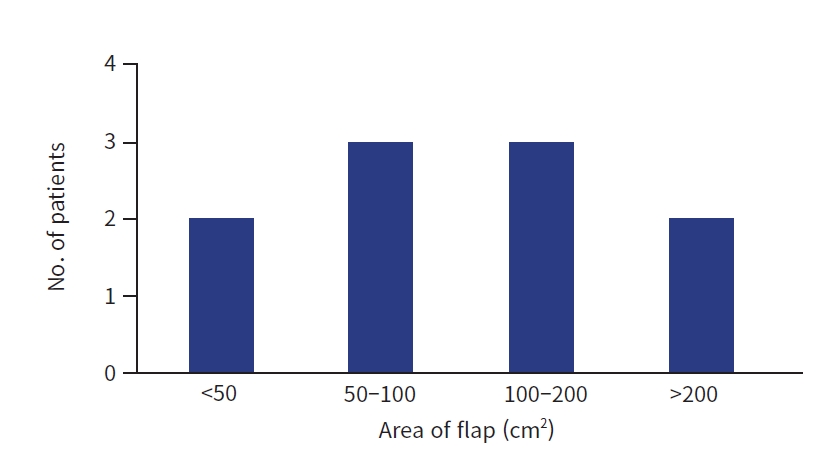
- The patients in this study ranged in age from 20 to 65 years, with an average age of 36.9 years. All 10 patients in our study group were male. The most common cause of the defect was trauma resulting from road traffic accidents, accounting for nine cases. One case was due to an injury from a fall from a height. The most frequently observed site of the defect was the proximal third of the leg, seen in seven cases, followed by defects around the knee in three cases. Regarding the location of the defect, soft tissue defects in our study were most commonly found on the anterolateral aspect of the proximal third of the leg, with five cases. The defects analyzed in the study had an average size of 98.3 cm2. The largest defect noted in the study measured 15×13 cm2 (Fig. 2). The area of the flap harvested in this study group ranged from 7×4 to 16×14 cm2 (Fig. 3). The pedicle length of the flap ranged from 10 to 15 cm, with an average of 11.7 cm. All patients underwent split skin grafting for closure of the donor site. Two patients experienced complications of distal necrosis, which was managed by flap debridement and reinsertion. These same two patients also experienced donor site graft loss, which was managed with supplementary grafting. Details of the cases are shown in Table 1.
- Representative cases
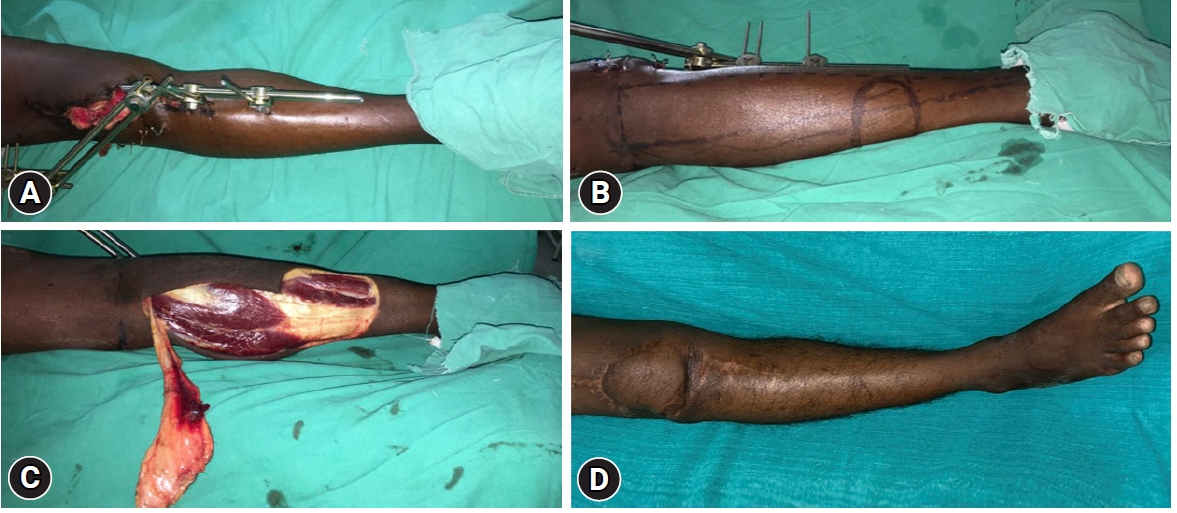
- A 32-year-old male patient experienced a road traffic accident (RTA)—specifically, a tractor tire ran over his leg while he was working in the field—and sustained an injury to his right leg (Fig. 4). He presented with a soft tissue defect on the anterolateral aspect of the proximal third of his leg, with an exposed implant. The dimensions of the defect were 15×10 cm2, and the flap size was 16×11 cm2, with a pedicle length of 11 cm. The postoperative period was uneventful, and the flap settled well.
- A 22-year-old male patient with a history of an RTA (a collision between a car and a bike) sustained an injury to his right leg (Fig. 5). He presented with a soft tissue defect on the anterolateral aspect of his knee, which exposed the distal femur. The dimensions of the defect were 12×6 cm2, and the flap size was 13×7 cm2, with a pedicle length of 15 cm. The postoperative period was uneventful, and the flap settled well.
- A 20-year-old male patient was in an RTA (a collision between a car and a truck) and sustained an injury to his left leg (Fig. 6). He presented with a soft tissue defect on the antero-lateral aspect of the proximal third of his leg, where an implant was exposed. The dimensions of the defect were 8×6 cm2. The flap size was 11×7 cm2, with a pedicle length of 11 cm. The postoperative period was uneventful, and the flap settled well.
RESULTS
Case 1
Case 2
Case 3
- Improving the optimal methods for recipient site reconstruction and minimizing donor site morbidity are ongoing areas of exploration in reconstructive surgery. Reconstructing soft tissue defects around the knee is often a challenge for plastic surgeons due to the specific requirements necessary for knee joint reconstruction. The chosen method for reconstruction should be straightforward, reproducible, and reliable, with minimal morbidity at the donor site. The donor tissue should possess thin, pliable, stretchable, and sensate skin. Additionally, the undersurface should be nonadhesive to ensure that the knee's flexion and extension functions are not compromised [1]. Various flaps have been proposed for covering these defects around the knee, including local flaps (muscle, fasciocutaneous, perforator), cross-leg flaps, or free flaps [3]. The gastrocnemius flap is the most commonly used muscle for covering defects in this area. This muscle flap is easy to execute and highly reliable. However, its lack of innervation and the potential for unsatisfactory cosmetic results (such as bulkiness and contour deformity) are notable drawbacks to the use of muscle flaps [4].
- The outcomes of local fasciocutaneous flaps are not consistently satisfactory. This is primarily because they are typically random pattern flaps with compromised vascularity at the tip. Consequently, distal necrosis often occurs at the site where these flaps are most needed. This subsequent healing process can compromise both the function and appearance of the knee joint [5].
- More recently, local perforator flaps have been increasingly utilized due to their notable advantages, including low donor morbidity and superior aesthetic outcomes. Perforator flaps, such as the medial sural artery perforator flap, anterior tibialis artery perforator flap, reversed anterolateral thigh perforator flap, and the pedicled vastus medialis perforator, are favored for reconstructing skin defects around the knee. These flaps provide thin, pliable skin that fulfils most of the reconstruction requirements in the knee area. The cosmetic results following the application of these flaps are excellent, and the morbidity at the donor site is also minimal. However, these flaps do have some drawbacks, including a lack of sensation, the need for a Doppler to locate a suitably sized perforator near the defect, and a long and somewhat tedious dissection process [6,7].
- The inferomedial thigh flap, which is based on perforators originating from the descending genicular artery, can provide flaps large enough to cover the entire knee. However, this procedure necessitates a preoperative evaluation of the perforator vessels, as this flap can occasionally experience venous congestion, sometimes requiring an additional venous microanastomosis with a local vein. Such vascular incidents are less common with the proximally based sural island flap. In our series, all 10 flaps survived completely, with no vascular incidents, demonstrating the reliability of its blood supply. All grafted donor sites healed satisfactorily.
- The proximally based sural island flap has proven capable of providing ample tissue for coverage. We have successfully raised flap dimensions as large as 16 cm ×14 cm2 to cover extensive defects. In the past, such large defects would have necessitated either a free flap or a cross-leg flap [1]. Microvascular reconstruction of defects in the knee joint area presents another viable option [8]. While this is a single-stage procedure, it does have its drawbacks. These include the need for specialized equipment, such as a microscope, and a surgeon with specific expertise. Additionally, identifying suitable recipient vessels at the site can also pose a challenge.
- The proximally based sural fasciocutaneous flap, utilized in our study, offers certain benefits. Its tissue is thin and pliable, and the flap's undersurface facilitates easy gliding of the knee joint. This flap is highly reliable and can be readily extended into the mid-third of the leg. It also has a long pedicle with a good arc of rotation, which allows for easy extension to the distal thigh [9].
- The flap offers several advantages, including its ease and speed of elevation, and the fact that it does not necessitate microsurgical skills or meticulous dissection of the pedicle. Furthermore, this flap is thin and sensate, contributing to an aesthetically pleasing appearance at the site. It promotes fracture healing in defects where the fracture site is exposed by providing a stable and durable soft tissue cover. In instances where an implant is exposed, it safeguards the implant from infection. The flap also provides a smooth gliding surface, facilitating free movement of the knee joint in cases of knee defects [2,3,9].
- Like any other flap, this one also has certain disadvantages, such as its appearance if a skin graft has been used at the donor site. This cosmetic disadvantage is not present if the donor site is primarily closed, specifically in cases where the flap width is less than 3 cm. However, in our study, the donor site was closed using split-thickness skin grafting in all cases. Since the donor site is located on the posterior calf region, which is typically concealed, most patients did not report this as a major complaint during the postoperative period, once the graft had completely settled. As the sural nerve is harvested along with the flap, there is a loss of sensation on the lateral side of the foot. This tends to diminish over time due to sensory overlap from surrounding regions, as observed in a well-established, distally based sural artery flap [2].
- Cheon et al. [2] also employed the same technique, using the flap for reconstruction around the knee joint in 10 cases, with a follow-up period of 1 to 2.5 years. The outcomes were similar to those in our study, as the flap was thin, sensate, and did not impede the function of the knee joint. In their study, the maximum flap size raised was only 6×10 cm2, whereas in our study, we were able to raise a flap with a maximum area of 15×13 cm2. Cheon et al. [2] identified the loss of sensation on the lateral side of the foot as a significant drawback, but in our study, patients did not cite this as a major issue during the postoperative period. Aside from the complications of marginal flap necrosis and donor site graft loss, which were observed in two cases, there were no other complaints from the patients, even after a long-term follow-up of over 1 year.
- Limitations
- The limitation of the study was its sample size. Although the sample size for this study was small, it still demonstrated the versatility and usefulness of this flap. Further research with larger cohorts is warranted to validate our findings and provide a more comprehensive assessment of its clinical applicability.
- Conclusions
- The proximally based sural fasciocutaneous flap is a workhorse flap used for the reconstruction of soft tissue defects around the knee and the proximal third of the leg. It has proven to be reliable, efficient, and more versatile than other reconstructive options such as local flaps (muscle, fasciocutaneous, perforator), cross-leg flaps, or free flaps. This flap is relatively easy to learn and harvest, making it an ideal alternative for covering soft tissue defects, as described in the study. It yields acceptable functional and aesthetic outcomes with minimal donor site morbidity. The flap offers the advantages of providing thin, reliable, sensate, and stable soft tissue coverage with a good gliding surface, and it can cover larger defects with minimal complications. With its ease of dissection, consistent vascular pedicle, antegrade blood supply, adequate venous drainage, and thin skin, it is superior to surrounding peer flaps and yields satisfactory outcomes.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no any financial support for this study.
-
Author contributions
Conceptualization: all authors; Data curation: PL, S Srinivas, DM, SP, S Sankar, SRC; Formal analysis: PL, S Srinivas, DM, SP; Methodology: PL, S Srinivas, DM, AS; Project administration: PL, S Srinivas, DM, SP, S Sankar, SCR; Visualization: PL, DM; Writing–original draft: all authors; Writing–review & editing: all authors; All authors read and approved the final manuscript.
-
Acknowledgments
The authors thank their family members and colleagues for their cooperation in completion of this study. The authors also thank the operating room, ward staff, and the clerical staff for their involvement and cooperation.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION


- 1. Deng C, Wei Z, Wang B, et al. The proximally based lateral superficial sural artery flap: a convenient and optimal technique for the reconstruction of soft-tissue defects around the knee. Int J Clin Exp Med 2016;9:15167–76.
- 2. Cheon SJ, Kim IB, Park WR, Kim HT. The proximally-based sural artery flap for coverage of soft tissue defects around the knee and on the proximal third and middle third of the lower leg: 10 patients followed for 1-2.5 years. Acta Orthop 2008;79:370–5. PubMed
- 3. Pan H, Zheng Q, Yang S. Utility of proximally based sural fasciocutaneous flap for knee and proximal lower leg defects. Wounds 2014;26:132–8. PubMed
- 4. Barfod B, Pers M. Gastrocnemius-plasty for primary closure of compound injuries of the knee. J Bone Joint Surg Br 1970;52:124–7. ArticlePubMedPDF
- 5. Satoh K, Fukuya F, Matsui A, Onizuka T. Lower leg reconstruction using a sural fasciocutaneous flap. Ann Plast Surg 1989;23:97–103. ArticlePubMed
- 6. Rad AN, Christy MR, Rodriguez ED, Brazio P, Rosson GD. The anterior tibialis artery perforator (ATAP) flap for traumatic knee and patella defects: clinical cases and anatomic study. Ann Plast Surg 2010;64:210–6. PubMed
- 7. Zheng HP, Lin J, Zhuang YH, Zhang FH. Convenient coverage of soft-tissue defects around the knee by the pedicled vastus medialis perforator flap. J Plast Reconstr Aesthet Surg 2012;65:1151–7. ArticlePubMed
- 8. Fisher J, Cooney WP 3rd. Designing the latissimus dorsi free flap for knee coverage. Ann Plast Surg 1983;11:554–62. ArticlePubMed
- 9. Suri MP, Friji MT, Ahmad QG, Yadav PS. Utility of proximally based sural artery flap for lower thigh and knee defects. Ann Plast Surg 2010;64:462–5. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Local or regional flaps in developing country: Experience from Eastern Bhutan
Kinzang Dorji
International Wound Journal.2024;[Epub] CrossRef
 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite