Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Original Article
Determining the appropriate resting energy expenditure requirement for severe trauma patients using indirect calorimetry in Korea: a retrospective observational study -
Hak-Jae Lee, MD
 , Sung-Bak Ahn, MD
, Sung-Bak Ahn, MD , Jung Hyun Lee, MD
, Jung Hyun Lee, MD , Ji-Yeon Kim, MD
, Ji-Yeon Kim, MD , Sungyeon Yoo, MD
, Sungyeon Yoo, MD , Suk-Kyung Hong, MD
, Suk-Kyung Hong, MD
-
Journal of Trauma and Injury 2023;36(4):337-342.
DOI: https://doi.org/10.20408/jti.2023.0051
Published online: November 3, 2023
- 632 Views
- 32 Download
Division of Acute Care Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- Correspondence to Hak-Jae Lee, MD Division of Acute Care Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Korea Tel: +82-2-3010-1568 Email: lhj206@hanmail.net
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- This study aimed to compare the resting energy expenditure (REE) measured using indirect calorimetry with that estimated using predictive equations in severe trauma patients to determine the appropriate caloric requirements.
-
Methods
- Patients admitted to the surgical intensive care unit between January 2020 and March 2023 were included in this study. Indirect calorimetry was used to measure the patients’ REE values. These values were subsequently compared with those estimated using predictive equations: the weight-based equation (rule of thumb, 25 kcal/kg/day), Harris-Benedict, Ireton-Jones, and the Penn State 2003 equations.
-
Results
- A total of 27 severe trauma patients were included in this study, and 47 indirect calorimetric measurements were conducted. The weight-based equation (mean difference [MD], –28.96±303.58 kcal) and the Penn State 2003 equation (MD, –3.56±270.39 kcal) showed the closest results to REE measured by indirect calorimetry. However, the REE values estimated using the Harris-Benedict equation (MD, 156.64±276.54 kcal) and Ireton-Jones equation (MD, 250.87±332.54 kcal) displayed significant differences from those measured using indirect calorimetry. The concordance rate, which the predictive REE differs from the measured REE value within 10%, was up to 36.2%.
-
Conclusions
- The REE values estimated using predictive equations exhibited substantial differences from those measured via indirect calorimetry. Therefore, it is necessary to measure the REE value through indirect calorimetry in severe trauma patients.
- Background
- Proper nutritional support plays a crucial role in the recovery of critically ill patients. Overfeeding and underfeeding are potentially associated with mortality [1,2]. Overfeeding can lead to complications such as infection, hyperglycemia, and ventilation weaning failure. Underfeeding can have some complications such as infection, skeletal muscle loss, impaired immune function, and delayed wound healing. Several studies have reported the importance of determining and supplying the appropriate amount of calories [2–6]. The American Society for Parenteral and Enteral Nutrition (ASPEN) and European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines recommend indirect calorimetry use to measure patients’ appropriate caloric intakes [7,8]. However, using indirect calorimetry in the clinical setting is challenging due to the associated costs and required resources. Therefore, the ASPEN guidelines recommend that a published predictive equation or simplistic weight-based equation (25 to 30 kcal/kg/day) be used to determine energy requirements [7].
- Notwithstanding, several studies have reported that these predictive equations are not sufficiently accurate [2,4,9,10]. Since calculations involving predictive equations are based on parameters such as patient height, weight, sex, and age, they do not accurately reflect a patient’s actual condition. In particular, severe trauma potentially leads to a cascade of metabolic responses. In addition to primary traumatic injury, various metabolic responses occur due to secondary injury, such as massive transfusion, resuscitation, generalized inflammation, and infection [11,12]. Although most trauma patients have normal nutritional statuses before hospital admission, these metabolic responses increase the risk of malnutrition. Therefore, determining the appropriate caloric requirements for trauma patients is imperative.
- Objectives
- This study aims to compare the resting energy expenditure (REE) measured by indirect calorimetry in severe trauma patients with the value obtained through the predictive equations.
INTRODUCTION
- Ethics statement
- This study was approved by the Institutional Review Board of Asan Medical Center (No. 2023-0355). The requirement for informed consent was waived due to the retrospective nature of the study.
- Study setting and patients
- This study retrospectively investigated trauma patients admitted to the surgical intensive care unit (ICU) between January 2020 and March 2023. Severe trauma patients with an Injury Severity Score (ISS) ≥15 who had undergone mechanical ventilation for more than 3 days were included in this study. Patients aged <18 years who were unable to undergo indirect calorimetric measurement (fraction of inspired oxygen >0.6, bronchopleural fistula, and/or persistent air leakage) were excluded. Patient-related data were retrospectively collected from electrical medical records and analyzed. Nutritional status at the ICU admission was classified according to the ASPEN malnutrition criteria [13].
- Indirect calorimetric measurement
- Indirect calorimetry was performed using a CARESCAPE Monitor B650 (GE Healthcare). REE was measured by three well-experienced critical care nurses. Measurements were conducted under the following strict conditions to obtain accurate results: (1) prohibition of interventions, such as positioning, suctioning, or hemodialysis that may stimulate the patients; (2) indirect calorimetric calibration for ≥10 minutes before each measurement; and (3) rest for ≥30 minutes before each measurement. Oxygen consumption and CO2 production were measured, and the respiratory quotient and REE were calculated using the Weir equation.
- Predictive equations
- REE was estimated using four predictive methods: the weight-based equation (rule of thumb, 25 kcal/kg/day) [14], Harris-Benedict equation [15], Ireton-Jones equation (for ventilated patients) [16], and the Penn State 2003 equation [17] (Table 1).
- Outcomes
- The primary outcome was the comparison between indirect calorimetry–measured and predictive equation–derived REE values. The secondary outcome was the concordance rate between the measured and predicted REE values. The concordance rate was defined as the value of the predictive equation–estimated REE that was within the 90% to 110% range of the indirect calorimetry–measured REE value.
- Statistical analysis
- Continuous, normally distributed variables are presented as mean±standard deviation. Measurements were compared using the paired t-test. Bland-Altman method was used to calculate the mean difference (MD) between predicted and measured REE values. Statistical significance was set at P<0.05. Statistical analyses were conducted using R ver. 4.2.3 (R Foundation for Statistical Computing).
METHODS
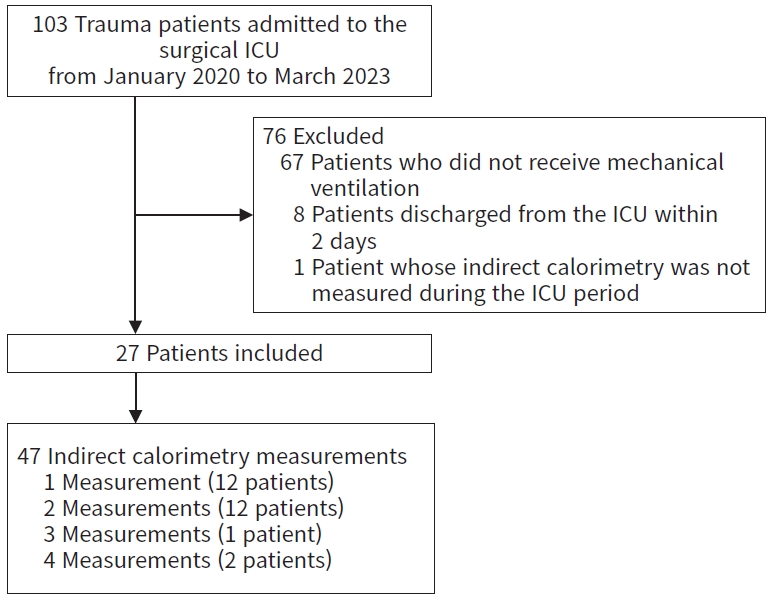
- A total of 47 indirect calorimetric measurements were performed on 27 trauma patients whose mean age was 55.6±18.3 years (Fig. 1). Traffic accidents, the most common cause, accounted for 15 patients (55.6%). The average ISS was 28.6±11.1, and 25 patients (92.6%) had normal nutritional statuses before ICU admission. The average length of stay in the ICU was 30.4±15.7 days, and the average length of hospital stay was 53.4±27.9 days (Table 2).
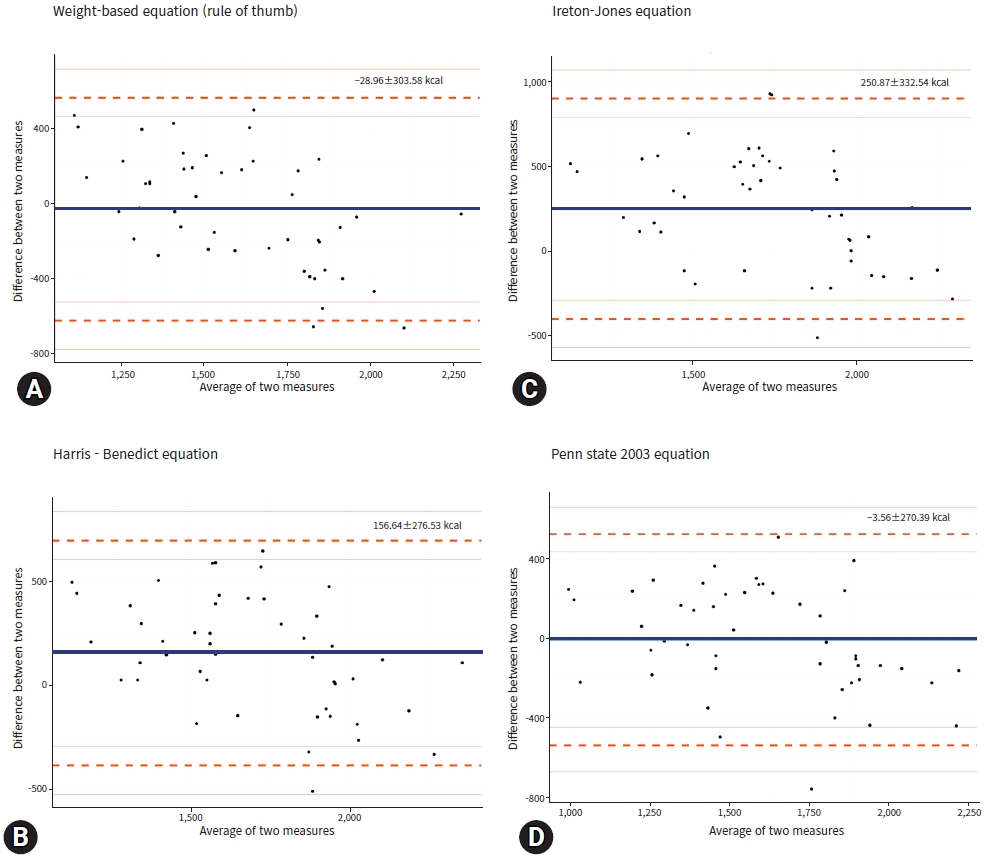
- The mean indirect calorimetry–measured REE value was 1,613.0±382.2 kcal, and the respiratory quotient was 0.73±0.06. Among the four predictive equations, the weight-based equation (MD, –28.96±303.58 kcal) and the Penn State 2003 equation (MD, –3.56±270.39 kcal) yielded the closest results, while Harris-Benedict and Ireton-Jones equations exhibited differences of 156.64±276.53 kcal (P=0.024) and 250.87±332.54 kcal (P=0.001), respectively. However, the concordance rate deviated from 27.6% to 36.2% (Table 3). Bland-Altman analysis revealed that each predictive equation–derived REE value differed significantly from the indirect calorimetry–measured REE value (Fig. 2).
RESULTS
- When treating severe trauma patients, proper nutritional therapy is important for their recovery. It is important to supply appropriate caloric requirements according to the patient’s recovery progress. Nevertheless, determining these values in actual clinical settings proves challenging. Therefore, although several guidelines recommend indirect calorimetry use for critically ill patients, using this technique is difficult due to various limitations. In particular, few hospitals use indirect calorimetry in Korea due to challenges such as insurance fees.
- Therefore, this study analyzed the concordance of predictive equations in comparison to that of indirect calorimetry. Four predictive equations typically used for critically ill and trauma patients were compared with the measured REE of indirect calorimetry. Among the four predictive equations, the simple weight-based equation and the Penn State 2003 equation yielded results that were most consistent with the indirect calorimetry–measured REE value. Several studies have reported that the Penn State 2003 equation showed the best results among several predictive equations. In a study by Kwon et al. [18], the Penn State equation produced the highest r-value (0.742; 95% confidence interval, 0.636 to 0.821) and least MD (54.8 kcal; range: –595.9 to 705.5). A study by Lee et al. [19], which targeted liver transplant patients, also found the Penn State equation showed the closest result to the measure REE. Kamel et al. [20] and Zusman et al. [21] reported that the Harris-Benedict equation yielded the closest REE value to that measured using indirect calorimetry; nevertheless, our study revealed a vast difference between the Harris-Benedict equation–derived REE value and that measured via indirect calorimetry. In contrast, our study found the REE value estimated using the weight-based equation to be most consistent with that measured using indirect calorimetry.
- However, when the concordance rate was analyzed to ascertain whether the error between the measured and predictive equation–derived REE values was within 10%, considerable disparities were obtained. Several studies have reported differences between predictive equation–derived and indirect calorimetry–measured REE values [4,20,21]. In a study by Zusman et al. [21], which retrospectively analyzed a large cohort of 1,440 critically ill patients, the concordance rate was analyzed based on an error of 15%. Moreover, the Harris-Benedict equation generated the best result, with a concordance rate of 15%, and other predictive equations yielded low concordance rates. In a study by Kamel et al. [20] on critically ill surgical patients, including trauma patients, the Harris-Benedict equation exhibited the highest concordance rate (65.2%). However, most of the other predictive equations yielded low concordance rates of 40% to 50%. In our study, which exclusively included severe trauma patients, all four predictive equations produced concordance rates within the 27.6% to 36.2% range, and they were lower than those in other studies. This means that it is more difficult to evaluate the appropriate caloric requirement through a predictive equation in severe trauma patients. Bland-Altman analysis revealed that each predictive equation’s REE value drastically deviated from the mean indirect calorimetry–measured REE value. Therefore, it is necessary to evaluate an appropriate caloric requirement through IC for severe trauma patients with complicated metabolic responses.
- Limitations
- This study has several limitations. First, the number of samples was small. The number of enrolled patients was small because it was limited to patients with severe trauma. Second, since the time points at which indirect calorimetric measurements were performed varied, the effect of measurement time points could not be compensated for. Finally, this was a single-center retrospective study; thus, selection bias might have arisen. A prospective large cohort study is required in the future.
- Conclusions
- The simplistic weight-based equation and the Penn State 2003 equation showed the similar results to the REE values measured through indirect calorimetry. However, this study’s findings suggest that the predictive equation–estimated energy expenditure of critically ill trauma patients deviates significantly from that measured using indirect calorimetry. Therefore, indirect calorimetry should be used to measure the REE values of severe trauma patients.
DISCUSSION
-
Author contributions
Conceptualization: HJL, SKH; Data curation: HJL, SBA, JHL, JYK, SY; Formal analysis: SBA, JYK, SWY; Visualization: HJL; Methodology: HJL, JHL, SKH; Writing–original draft: HJL; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Author contributions
Conceptualization: HJL, SKH; Data curation: HJL, SBA, JHL, JYK, SY; Formal analysis: SBA, JYK, SWY; Visualization: HJL; Methodology: HJL, JHL, SKH; Writing–original draft: HJL; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION

| Name | Equation |
|---|---|
| Weight-based equation [14] | REE=25×W |
| Harris-Benedict equation [15] | Male: REE=1.3 (stress factor)×(66.47+13.75×W+5×H–6.755×A) |
| Female: REE=1.3 (stress factor)×(665.1+9.563×W+1.85×H–4.676×A) | |
| Ireton-Jones equation [16] (for ventilated patients) | Male: REE=2028–11(A)+5(W)+239(T)+804(B) |
| Female: REE=1,784–11(A)+5(W)+239(T)+804(B) | |
| Penn State 2003 equation [17] | REE=0.85×HBE+175×Tmax+33×VE–6433 |
- 1. Hiesmayr M. Nutrition risk assessment in the ICU. Curr Opin Clin Nutr Metab Care 2012;15:174–80. ArticlePubMed
- 2. Zusman O, Theilla M, Cohen J, Kagan I, Bendavid I, Singer P. Resting energy expenditure, calorie and protein consumption in critically ill patients: a retrospective cohort study. Crit Care 2016;20:367. ArticlePubMedPMCPDF
- 3. Klein CJ, Stanek GS, Wiles CE 3rd. Overfeeding macronutrients to critically ill adults: metabolic complications. J Am Diet Assoc 1998;98:795–806. PubMed
- 4. Tatucu-Babet OA, Ridley EJ, Tierney AC. Prevalence of underprescription or overprescription of energy needs in critically ill mechanically ventilated adults as determined by indirect calorimetry: a systematic literature review. JPEN J Parenter Enteral Nutr 2016;40:212–25. PubMed
- 5. Villet S, Chiolero RL, Bollmann MD, et al. Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 2005;24:502–9. ArticlePubMed
- 6. Moonen HP, Beckers KJ, van Zanten AR. Energy expenditure and indirect calorimetry in critical illness and convalescence: current evidence and practical considerations. J Intensive Care 2021;9:8. ArticlePubMedPMCPDF
- 7. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40:159–211. PubMed
- 8. Singer P, Blaser AR, Berger MM, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr 2019;38:48–79. ArticlePubMed
- 9. Vasileiou G, Qian S, Iyengar R, et al. Use of predictive equations for energy prescription results in inaccurate estimation in trauma patients. Nutr Clin Pract 2020;35:927–32. ArticlePubMedPDF
- 10. Ma DS, Lee GJ. Comparison of resting energy expenditure using indirect calorimetry and predictive equations in trauma patients: a pilot study. J Trauma Inj 2021;34:13–20. ArticlePDF
- 11. Rogobete AF, Grintescu IM, Bratu T, et al. Assessment of metabolic and nutritional imbalance in mechanically ventilated multiple trauma patients: from molecular to clinical outcomes. Diagnostics (Basel) 2019;9:171. ArticlePubMedPMC
- 12. Byerly SE, Yeh DD. The role of indirect calorimetry in care of the surgical patient. Curr Surg Rep 2022;10:186–91. ArticlePubMedPMCPDF
- 13. White JV, Guenter P, Jensen G, et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet 2012;112:730–8. ArticlePubMed
- 14. Singer P, Berger MM, Van den Berghe G, et al. ESPEN guidelines on parenteral nutrition: intensive care. Clin Nutr 2009;28:387–400. ArticlePubMed
- 15. Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci U S A 1918;4:370–3. ArticlePubMedPMC
- 16. Ireton-Jones CS, Turner WW Jr, Liepa GU, Baxter CR. Equations for the estimation of energy expenditures in patients with burns with special reference to ventilatory status. J Burn Care Rehabil 1992;13:330–3. ArticlePubMed
- 17. Frankenfield D, Smith JS, Cooney RN. Validation of 2 approaches to predicting resting metabolic rate in critically ill patients. JPEN J Parenter Enteral Nutr 2004;28:259–64. ArticlePubMed
- 18. Kwon J, Lee JH, Kim M, Choi D. Nutritional assessment formulae for nutritional requirement determination in severe trauma. Asia Pac J Clin Nutr 2022;31:611–8. PubMed
- 19. Lee SJ, Lee HJ, Jung YJ, Han M, Lee SG, Hong SK. Comparison of measured energy expenditure using indirect calorimetry vs predictive equations for liver transplant recipients. JPEN J Parenter Enteral Nutr 2021;45:761–7. ArticlePubMedPDF
- 20. Kamel AY, Robayo L, Liang D, et al. Estimated vs measured energy expenditure in ventilated surgical-trauma critically ill patients. JPEN J Parenter Enteral Nutr 2022;46:1431–40. ArticlePubMedPDF
- 21. Zusman O, Kagan I, Bendavid I, Theilla M, Cohen J, Singer P. Predictive equations versus measured energy expenditure by indirect calorimetry: a retrospective validation. Clin Nutr 2019;38:1206–10. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite