Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Case Report
Massive traumatic abdominal wall hernia in pediatric multitrauma in Australia: a case report -
Sarah Douglas-Seidl, MD
 , Camille Wu, MBBS
, Camille Wu, MBBS
-
Journal of Trauma and Injury 2023;36(4):447-450.
DOI: https://doi.org/10.20408/jti.2023.0023
Published online: November 7, 2023
- 453 Views
- 10 Download
Department of Pediatric Surgery, Sydney Children's Hospital, Randwick, NSW, Australia
- Correspondence to Sarah Douglas-Seidl, MD Department of Pediatric Surgery, Sydney Children's Hospital, High St, Randwick, NSW 2031, Australia Tel: +61-2-9382-1111 Email: dr.sarah.seidl@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Traumatic abdominal wall hernia is a rare presentation, most commonly reported in the context of motor vehicle accidents and associated with blunt abdominal injuries and handlebar injuries in the pediatric population. A 13-year-old boy presented with multiple traumatic injuries and hemodynamic instability after a high-speed motor vehicle accident. His injuries consisted of massive traumatic abdominal wall hernia (grade 4) with bowel injury and perforation, blunt aortic injury, a Chance fracture, hemopneumothorax, and a humeral shaft fracture. Initial surgical management included partial resection of the terminal ileum, sigmoid colon, and descending colon. Laparostomy was managed with negative pressure wound therapy. The patient underwent skin-only primary closure of the abdominal wall and required multiple returns to theatre for debridement, dressing changes, and repair of other injuries. Various surgical management options for abdominal wall closure were considered. In total, he underwent 36 procedures. The multiple injuries had competing management aims, which required close collaboration between specialist clinicians to form an individualized management plan. The severity and complexity of this injury was of a scale not previously experienced by many clinicians and benefited from intrahospital and interhospital specialist collaboration. The ideal aim of primary surgical repair was not possible in this case of a giant abdominal wall defect.
- A traumatic abdominal wall hernia (TAWH) is a rare presentation [1]. Disruption of the abdominal wall muscles and fascia causes a TAWH, which most commonly occurs as a result of a motor vehicle accident (MVA) [1,2]. Blunt abdominal injuries are associated with 0.9% of TAWHs [3]. In most cases, TAWHs are accompanied by ecchymoses [1]. Associations have been made between diagnostic findings and grading (grades I–IV) [1]. TAWHs can be classified according to their cause [4]. Multiple factors, including the timing of the diagnosis, size of the abdominal wall defect and the presence of intra- or extra-abdominal injuries, determine the surgical management of TAWHs [4]. Most TAWH patients require surgical management [1]. Delays in diagnosis have been found in 20% of TAWH cases, with reported delays of between 2 days and 9 years [1].
INTRODUCTION
- A 13-year-old boy was transferred to the emergency department of Sydney Children’s Hospital (Randwick, Australia) with traumatic injuries sustained as a car passenger in a high-speed MVA. He had initially been managed in a regional emergency department. On scene, the patient had a Glasgow Coma Scale score that fluctuated between 12 and 14, and he was hemodynamically unstable, requiring transfusions. Emergency management at the scene included intercostal catheter (left side) and endotracheal tube insertion, as well as ongoing blood transfusions for hemodynamic instability. On arrival to our facility, the patient had received 4 units of blood.
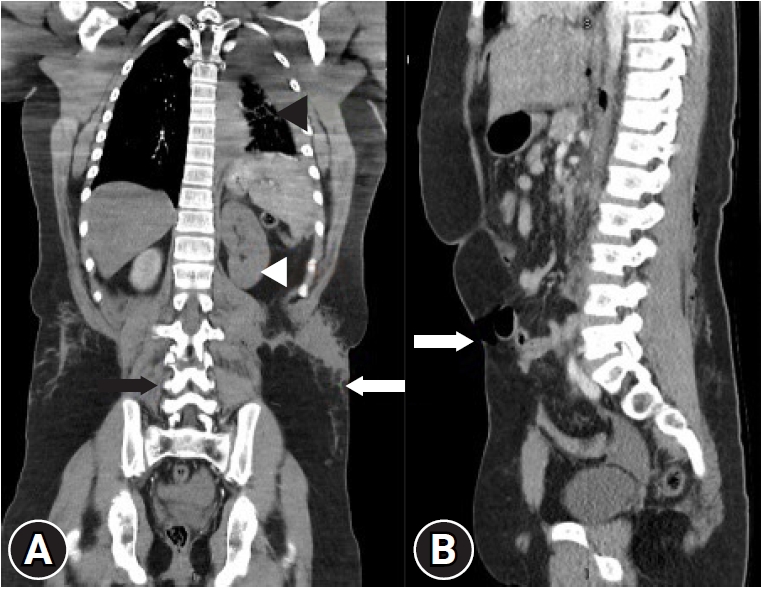
- The physical examination revealed seatbelt bruising with abrasions and ecchymosis to the lower abdomen and pelvis. Focused assessment with sonography for trauma showed fluid in the right upper quadrant. A computed tomography (CT) scan revealed herniation of abdominal contents through a ruptured transverse abdominal rectus muscle, with sigmoid colonic rupture, left kidney injury, and a left side hemopneumothorax with associated lung contusion requiring intercostal catheter insertion. Computed tomography angiography (CTA) was suggestive of blunt aortic injury at the level of the visceral aorta with aortic hematoma, occlusion of the left renal artery with total devascularization of the left kidney, and intraluminal thrombus between the right renal artery and superior mesenteric artery with partial devascularization of the right kidney (Fig. 1). The CT scan also showed a vertebral flexion and distraction fracture at L4 involving the middle and posterior columns, an L3 transversus process fracture, and a markedly displaced right humeral shaft fracture.
- Surgery involved resection of devitalized terminal ileum, distal descending and sigmoid colon, and hemostatic packing. Negative pressure wound therapy dressing was applied. The patient was admitted to the pediatric intensive care unit for hemodynamic instability, ongoing bleeding, and ventilation requirement. Continued blood loss from the abdominal drains (above 1l) required relook laparotomy on postoperative day (POD) 1 with renewal of hemostatic packing. The patient was coagulopathic, and he had blood loss and was hemodynamically unstable, which required increased inotropic support postoperatively. Due to instability and concerns about sepsis from extensive necrotic abdominal wall tissue, he required a second relook the same day with radical debridement, which resulted in the loss of most of the anterior abdominal wall. Due to extensive debridement requirements, a third relook and debridement were performed on POD 2 with plastic, colorectal, and vascular surgery teams in attendance for inspection and planning ongoing management. The lack of abdominal wall precluded stoma formation, and two primary anastomoses were performed (ileocolic and descending colon-sigmoid) on POD 4 during a planned relook, along with debridement of the abdominal wound and vacuum-assisted closure dressing change (Fig. 2). Surgical tracheostomy was performed on day 10 of admission. The unstable Chance fracture required ongoing spinal precautions. Laminectomy was delayed by more than 1 month, as the patient was unable to be placed prone due to the lack of an abdominal wall. The patient required approximately 20 further procedures for regular dressing changes and debridement.
- After 3 and a half months, the abdominal wound was fully granulated. The plastic surgery team performed skin-only closure of the abdominal wall, with grafting of a 10×5-cm defect in the right inguinal area. The patient was discharged 5 months after initial presentation. An extensive multidisciplinary team, including nurses, physiotherapists, anesthesiologists for acute and chronic complex pain management, mental health professionals, and social work practitioners, was involved in the management of this patient.
- Ethics statement
- Informed consent for publication of the research details and clinical images was obtained from the patient.
CASE REPORT
- MVAs are the commonest cause of TAWHs in adults [1]. In contrast, TAWHs in children are most commonly associated with handlebar injuries, with relatively few reported pediatric cases due to MVAs [1]. Most reported TAWHs are grade V [1]. In 60% of adult patients with TAWH and intra-abdominal injuries, these were most commonly bowel injuries (44%), followed by solid organ injuries (35%) [1]. In 40% of children with TAWH intra-abdominal injuries, bowel injuries comprised 70% [5]. Despite the lower number of intra-abdominal injuries in children the percentage of bowel injuries is higher than in the adult patient group (28% in children and 26.4% in adults).
- As yet, there is no common consensus on diagnosis and management. Diagnostic imaging is correlated with intraoperative findings [1]. In most cases, TAWHs are located in the right lower quadrant of the abdomen (33%), followed by the left lower quadrant (27%) [1]. AWHs cannot be distinguished from preexisting abdominal hernias on CT. The hernia mostly contains the small bowel (69%) [1]. Most children with TAWHs (85%) require surgical management, and 80% undergo laparotomy [5].
- Traumatic abdominal aortic injury (TAAI) is rare and generally associated with polytrauma [6]. TAAI occurs in <1% of blunt abdominal traumas. Most TAAI cases have been reported in the context of MVAs and diagnosed by CT or CTA, or during exploration. The clinical findings of TAAI are limited to severe cases [6]. Most blunt abdominal aortic injuries have been reported at the level of the inferior mesenteric artery (33%), followed by the renal arteries (24%) [6,7]. Vertebral fractures have been reported in 27% of adults with TAWHs [2]. Traumatic lumbar spine fractures are generally associated with transverse process fractures [8]. Flexion and distraction spinal fractures usually involve T11 to L2 and result from head-on-car collisions [9].
- In summary, we describe a complex pediatric case of TAWH complicated by abdominal aortic injury and vertebral fracture. Our total of 36 procedures for TAWHs in children and the complexity of surgical involvement constitute a rare scenario.
DISCUSSION
-
Author contributions
Conceptualization: all authors; Writing–original draft: SDS; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION
- 1. Suhardja TS, Atalla MA, Rozen WM. Complete abdominal wall disruption with herniation following blunt injury: case report and review of the literature. Int Surg 2015;100:531–9. ArticlePubMedPMCPDF
- 2. Chow KL, Omi EC, Santaniello J, et al. Traumatic abdominal wall hernias: a single-center case series of surgical management. Trauma Surg Acute Care Open 2020;5:e000495. ArticlePubMedPMC
- 3. Netto FA, Hamilton P, Rizoli SB, et al. Traumatic abdominal wall hernia: epidemiology and clinical implications. J Trauma 2006;61:1058–61. ArticlePubMed
- 4. Akbaba S, Gundogdu RH, Temel H, Oduncu M. Traumatic abdominal wall hernia: early or delayed repair. Indian J Surg 2015;77(Suppl 3):963–6. ArticlePubMedPMCPDF
- 5. Theodorou CM, Stokes SC, Beres AL. Traumatic abdominal wall hernia in children: a systematic review. J Surg Res 2021;262:181–9. ArticlePubMedPMC
- 6. Ballard DH, Kaskas NM, Hamidian Jahromi A, Skweres J, Youssef AM. Abdominal wall hernia and aortic injury secondary to blunt trauma: case report and review of the literature. Int J Surg Case Rep 2014;5:1238–41. ArticlePubMedPMC
- 7. Nucifora G, Hysko F, Vasciaveo A. Blunt traumatic abdominal aortic rupture: CT imaging. Emerg Radiol 2008;15:211–3. ArticlePubMedPDF
- 8. Park DK. Fractures of the thoracic and lumbar spine [Internet]. OrthoInfo, American Academy of Orthopaedic Surgeons; 2020 [cited 2022 May 27]. Available from: https://orthoinfo.aaos.org/en/diseases--conditions/fractures-of-the-thoracic-and-lumbar-spine/.
- 9. Shahriari M, Sadaghiani MS, Spina M, Yousem DM, Franck B. Traumatic lumbar spine fractures: transverse process fractures dominate. Clin Imaging 2021;71:44–8. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- A method of bedside urethrography before catheterization in pelvic trauma in Korea: a case report
- Blunt abdominal trauma resulting in pancreatic injury in a pediatric patient in Australia: a case report
- Penetrating gallbladder injury in a pediatric patient: a case report
- Traumatic tension enterothorax in New Zealand: a case report
- Management of a traumatic avulsion fracture of the occipital condyle in polytrauma patient in Korea: a case report
 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite



