Distally based lateral supramalleolar flap for reconstructing distal foot defects in India: a prospective cohort study
Article information
Abstract
Purpose
Defects involving the ankle and foot are often the result of road traffic accidents. Many such defects are composite and require a flap for coverage, which is a significant challenge for reconstructive surgeons. Various locoregional options, such as reverse sural artery, reverse peroneal artery, peroneus brevis muscle, perforator-based, and fasciocutaneous flaps, have been used, but each flap type has limitations. In this study, we used the distally based lateral supramalleolar flap to reconstruct distal dorsal defects of the foot. The aim of this study was to analyze the efficacy of the flap in reconstructing distal dorsal defects of the foot. The specific objectives were to study the adequacy, reach, and utility of the lateral supramalleolar flap for distal defects of the dorsum of the foot; to observe various complications encountered with the flap; and to study the functional outcomes of reconstruction.
Methods
The distal dorsal foot defects of 10 patients were reconstructed with distal lateral supramalleolar flaps over a period of 6 months at a tertiary care center, and the results were analyzed.
Results
We were able to effectively cover distal foot defects in all 10 cases. Flap congestion was observed in two cases, and minor graft loss was seen in two cases.
Conclusions
The distally based lateral supramalleolar flap is a good pedicled locoregional flap for the coverage of distal dorsal foot and ankle defects of moderate size, with relatively few complications and little morbidity. It can be used as a lifeboat or even substitute for a free flap.
INTRODUCTION
Background
Defects involving the ankle and foot, seen commonly in clinical settings, are often the result of road traffic accidents (RTAs). These are mostly composite defects that may involve tendons, bones, joints, and neurovascular structures. These composite defects are quite challenging and often require the combined intervention of orthopedic and plastic surgeons. A typical defect involving multiple components of the foot usually requires staged reconstruction: skeletal stabilization first, followed by a stable cover with thin, pliable soft tissue and, if required, repair and reconstruction of the bone after the flap cover has settled. For optimum recovery and salvage of foot defects, early intervention is key in the form of debridement and a plan for definitive reconstruction. The assessment of distal vascularity is another major step in deciding our treatment modality. Various options are available for the coverage of foot defects, such as grafts, local flaps, pedicled flaps, perforator-based flaps, and free flaps. Using a skin graft to cover mobile sites is not ideal because more damage may occur and function may be impaired. Therefore, the use of fasciocutaneous flaps for covering these defects encourages vascularity at the site, provides a stable cover to the exposed vital structures, and offers a good gliding surface for tendons. Locoregional flap options available for foot defects are the reverse sural artery (RSA) flap, reverse peroneal artery (RPA) flap, peroneus brevis muscle flap, perforator-based fasciocutaneous flaps, and lateral supramalleolar flap. Each flap has its own merits and demerits. In this study, we investigated the specific advantages of the distally based lateral supramalleolar flap over other pedicled options. A classical lateral supramalleolar flap can be used for reconstruction of defects in the distal third of the leg, the ankle, and the proximal foot, whereas a distally based lateral supramalleolar flap can cover moderately sized distal defects of the dorsum of the foot.
Objectives
The purpose of our study was to test the efficiency of the distally based lateral supramalleolar flap for reconstruction of defects of the distal dorsal foot and ankle. The specific objectives of our study were to study the adequacy, reach, and usefulness of a lateral supramalleolar flap for distal defects of the dorsum of the foot; to observe various complications encountered with the flap; and to study the functional outcomes of reconstruction.
METHODS
Ethics statement
We conducted this study in compliance with the principles of the Declaration of Helsinki. The study’s protocol was reviewed and approved by the Institutional Review Board of Osmania Medical College (No. ECR/300/Inst/AP/2013/RR-20). Written informed consent was obtained from the patients.
Study design
This prospecitve cohort study followed patients with distal defects of the dorsum of the foot for 6 months, after direct admission to a tertiary care center in Telangana or referral from an orthopedics department. Participants’ defects were reconstructed using a lateral supramalleolar flap. Patients with an injury to the intended flap area (lateral perimalleolar area), the anterior tibial artery, or in areas of communication between the anterior tibial and anterior lateral malleolar arteries were excluded from the study.
After an initial workup and hemodynamic stabilization, patients were taken for skeletal stabilization by orthopedic surgeons. Debridement of the wound and defect analysis were performed, and the defect was reconstructed with a distal lateral supramalleolar flap. The postoperative position was maintained with splint support or external fixation. The flap was clinically monitored postoperatively, and complications were analyzed.
Demographic parameters were recorded, including age, sex, etiology, time of presentation, defect site, defect size, defect extent, dimensions of the flap, the distance of the anterior perforating branch of peroneal artery from the tip of the lateral malleolus, distal communication with the anterior tibial artery, and postoperative complications.
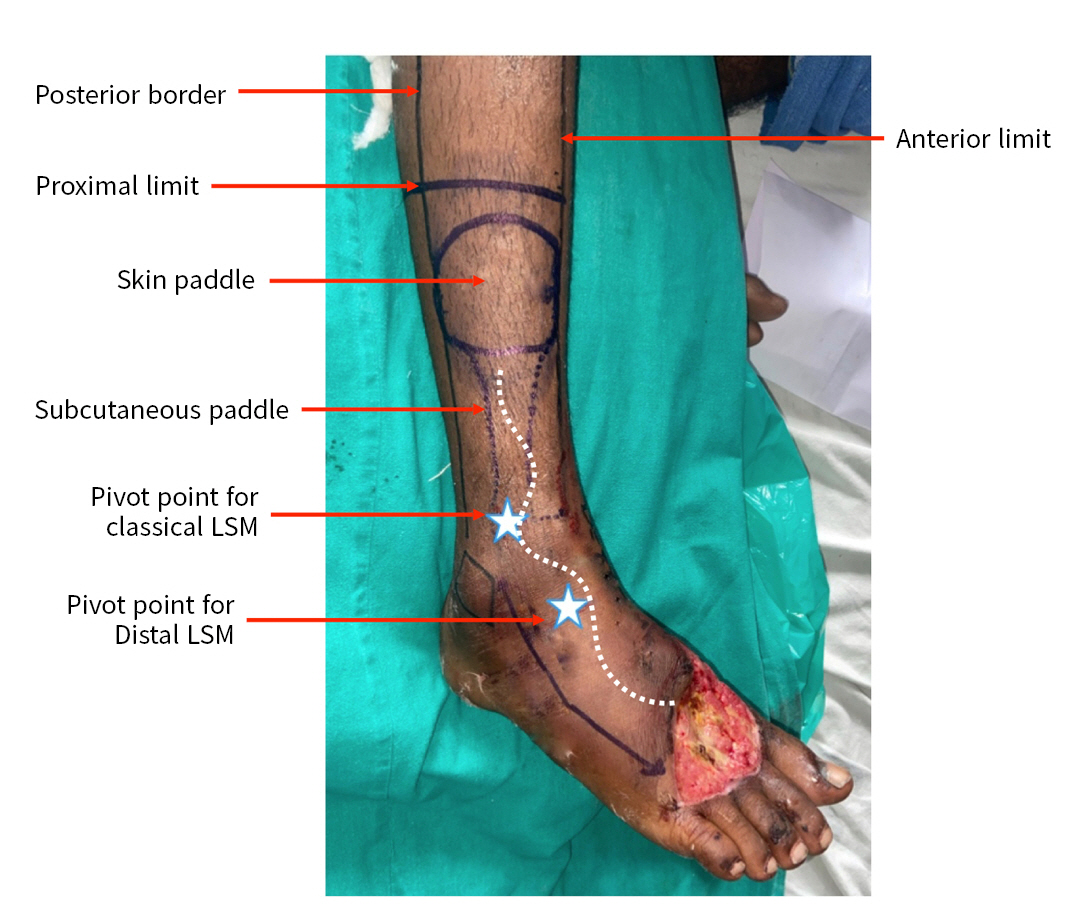
Lateral supramalleolar flap design and planning
The anterolateral lower half of the leg is supplied by the superficial cutaneous branch of the anterior perforating branch of the peroneal artery (Figs. 1, 2). The proximally based lateral supramalleolar flap is based on the anterior perforating branch of the peroneal artery, with a pivot point 5-cm superomedial to the tip of the lateral malleolus in the tibia-fibular groove. In contrast, the distally based lateral supramalleolar flap is based on the distal communications of the peroneal artery with the anterior tibial artery, that is, the sinus tarsus branch and anterior lateral malleolar artery; blood flow comes from the anterior tibial artery by extending its reach to the most distal parts of the dorsal foot (Fig. 1). The upper border of the flap is the midpoint of the leg in a lateral neutral line, the anterior border is the shin or tibia, and the posterior border is the posterior side of the fibula. The perforating branch of the peroneal artery 5-cm supramedial and the distal communication with the anterior tibial artery were marked with a handheld Doppler ultrasound device. The defect was measured and transposed on the leg’s anterolateral surface in the lower half with a pivot point at the communicating vessels, and planning was done in reverse. The superficial peroneal nerve was included with the flap in order to increase the blood supply around the nerve (Fig. 3).
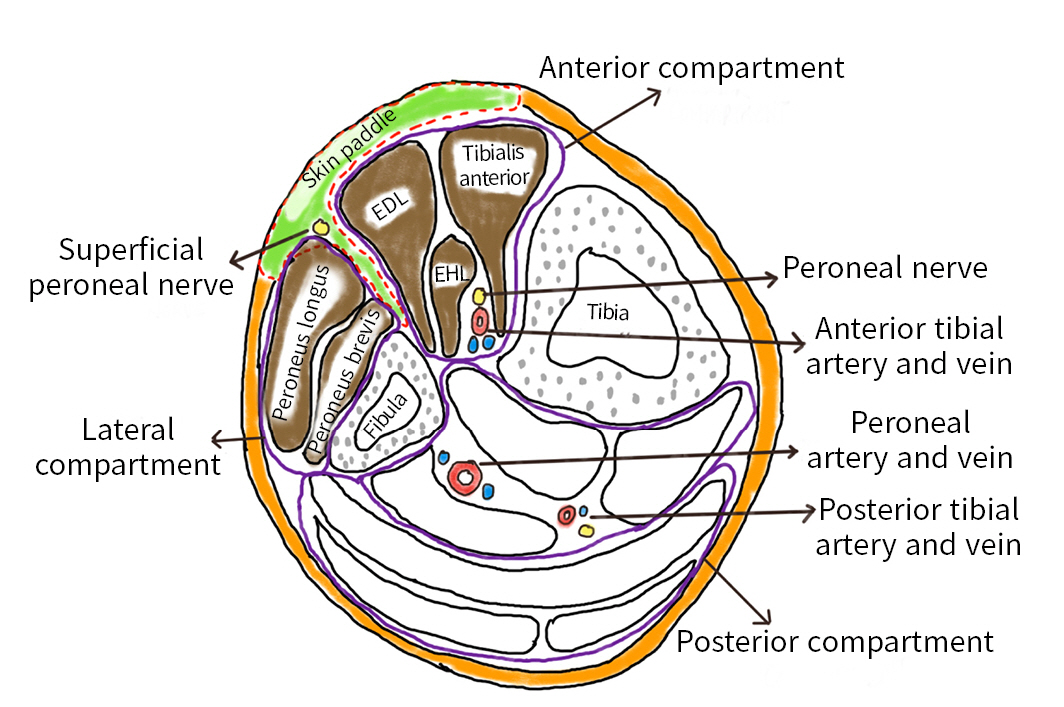
Cross-section of lower leg showing region of lateral supramalleolar skin flap. EDL, extensor digitorum longus; EHL, extensor hallicus longus.
Description of participants
Ten patients ranging from 17 to 67 years of age (eight male and two female patients) were included in the study, of whom nine (90%) were young to middle-aged and one (10%) was geriatric. The right foot was more commonly affected (80%). All patients (100%) presented within the 1st week of injury. The defect location was the distal dorsum of the foot in nine patients (90%) and the distal ankle in one patient (10%).
RESULTS
All cases (100%) were caused by RTAs. The average defect size was 5.8×4.7 cm, with a range from 4 to 8 cm. The average pedicle length was 8.6 cm. After passing through the interosseous membrane, the anterior perforating branch emerged an average of 5 cm superomedial to the tip of the lateral malleolus in the tibio-fibular groove. The first distal communication, namely the anterior lateral malleolar artery, was seen on average 3.8 cm distal to the lateral malleolus (range, 3–5 cm). The average pedicle width was 2.97 cm. The farthest extent of a flap was up to the base of the toes (Table 1, Fig. 4).

Demographic data of patients with details of the defects and distally based lateral supramalleolar flaps.
Islanded flaps were performed in all cases (100%). All flaps healed well and provided good coverage. Minor complications were seen in four cases. In two cases (20%) where congestion occurred in the distal few centimeters, one was relieved and healed well with conservative treatment, and the other developed partial necrosis of 2 cm, which required debridement and grafting. There was minimal graft loss in two cases over the donor area and pedicle, both of which were mended with skin grafts. The postoperative position was maintained with splint support (90%), and external fixation was used in one case (10%) to maintain the position. The mean hospital stay was 5 days.
DISCUSSION
The distal vasculature of the leg, ankle, and foot has been studied extensively, especially the septocutaneous perforators and communications between the peroneal artery and the anterior tibial artery. Several studies have discussed the distal anterolateral vascular communications in the lower leg and ankle, which form the basis of the lateral supramalleolar flap [1–3]. The lateral supramalleolar flap was first described by Romana and Masquelet [4] in 1989, as part of a detailed discussion of both the classical and the distally based lateral supramalleolar flaps. The relevant vasculature and its variations have been noted in detail by Cormac and Lamberty [5]. In the distally based lateral supramalleolar flap, septocutaneous perforators arising from the peroneal artery and its distal communications with the anterior tibial artery, namely the anterior lateral malleolar artery or the sinus tarsi artery, form the retrograde vascular supply from the anterior tibial artery. The flap marking and design have also been described in Grabb’s Encyclopedia of Flaps [6].
Several locoregional options have been described to cover defects in the ankle and foot region, including the dorsalis pedis flap [7], RSA flap [8,9], RPA flap [10], distally based fasciocutaneous flap [11], perforator-based propeller flap [12], peroneus brevis muscle flap [13], and lateral supramalleolar flap [4]. Each flap has its own advantages and disadvantages. Although the RSA flap is a general-purpose workhorse for lower leg, ankle, and proximal foot defects, it is prone to congestion. In addition, its reach is limited to the hind foot and mid-foot, and extending its reach requires prior delay for extended reach, which increases the number of operations and may pose a greater risk of complications. Although the RPA flap offers coverage for large defects of the distal foot and the sole, it involves sacrifice of a major vessel (the peroneal artery), tedious dissection, increased operative time, and relatively great expertise. The distally based dorsalis pedis flap also has limited reach for coverage of medium-sized defects of the lateral foot, compared to coverage of medium-sized defects anywhere on the dorsum of the foot. The peroneus brevis muscle flap is useful only for coverage of small defects of the proximal foot and ankle, and it sacrifices the muscle. The distally based fasciocutaneous and propeller flaps have limited reach and require tedious dissection and substantial expertise.
In contrast, the distally based lateral supramalleolar flap offers a unique solution for coverage of distal ankle and distal dorsal foot defects with fewer complications than with other pedicled flaps. The overall flap survival rate was 100%. The main advantages of this flap are as follows. First, the length and therefore the reach of the pedicle can be significantly increased by basing it on distal communications with the anterior tibial artery, which allows its reach to extend as far as the base of the toes. Second, the islanded flap eliminates the need for a secondary procedure. Third, the muscular bed at the flap donor site and the subcutaneous pedicle offer a reliable graft uptake. Fourth, this flap can cover small as well as moderately sized defects of the distal dorsal foot. Fifth, when microsurgical facilities are not available, the surgeon can use it as a lifeboat for a free flap, or even as a substitute for a free flap.
The drawbacks of the flap we encountered were that it is suitable only for moderately sized defects of the ankle and dorsal foot, the flap donor site leaves a scar in a relatively exposed area, and it cannot be used in weight-bearing areas, such as sole defects. In a recent study conducted by Mehmood Hashmi et al. [14] concerning 26 cases of classical (proximally based) supramalleolar flaps, two cases each of flap tip necrosis and venous congestion were observed. In contrast, in our study, which used distally based supramalleolar flaps, only one case of distal tip necrosis and two cases of venous congestion were observed.
In a study of seven distally based adipofascial lateral supramalleolar flaps, Lee et al. [15] observed that an adipofascial flap resulted in less damage to the donor site. An article by Uysal et al. [16] stated that because the distally based lateral supramalleolar flap is an adipofascial turnover flap, it is more prone to venous congestion, with an added risk of pedicle kinking. For this reason, they avoided creating a subcutaneous tunnel for the pedicle to pass through. In our study, which used a distally based adipofasciocutaneous lateral supramalleolar flap instead of an adipofascial flap, we similarly found that venous congestion occurred in two cases and preferred to avoid a subcutaneous tunnel. Instead, we raised subnormal flaps at the normal intervening skin between the defect and the skin paddle for the passage of our subcutaneous pedicle, which allowed a single-stage procedure without much damage to the surrounding tissues. Aside from the studies cited above, few studies have been published regarding either the distally based adipofasciocutaneous lateral supramalleolar flap or the distally based adipofascial lateral supramalleolar flap.
After defect measurement and planning in reverse, the course of the anterior perforating branch of the peroneal artery and the distal communications with anterior tibial artery were identified using a handheld Doppler device (8 MHz), and the flap area was marked. The limb was elevated, and a tourniquet was applied without exsanguination.
First, subdermal flaps (via a lazy-S incision) were elevated over the pedicle at the anterior boundary. The pedicle was elevated on one side, and the cutaneous branch to the skin paddle was identified. Then the anterior compartment tendons at the tibiofibular groove were retracted to demonstrate the perforating branch of the peroneal artery at the tibiofibular groove, as it emerges from the interosseous membrane. After that, the superior border was incised, and the superficial peroneal nerve was dissected and tagged to the skin paddle and deep fascia. Further dissection of the flap was carried out, and the lateral intermuscular septum was dissected between the peroneus brevis and extensor digitorum longus and included in the flap. Distally, subperiosteal dissection was required to elevate the pedicle from the fibula. To check the adequacy of retrograde supply, the perforating branch was clamped proximal to the bifurcation of the superficial and deep branches at its exit from the interosseous membrane. Then, the perforating branch was ligated and severed just proximal to the bifurcation of the superficial cutaneous and deep descending branches. Further dissection of the islanded pedicle continued until the distal communication with the anterior tibial artery and the flap’s reach were checked. The flap was then transposed onto the defect and inset. A split-thickness skin graft cover was applied over the flap donor site and the pedicle (Fig. 5). To maintain position, a splint or optional external fixation could be used.

Operative steps. (A) A lazy-S incision (line) over the pedicle. The proximal star represents the perforator for classical lateral supramalleolar flap, which has limited reach. The distal star represents the perforator for the distally based lateral supramalleolar flap, which has extended reach. (B) Entry of superficial cutaneous branch into the skin paddle (arrow and circle). (C) Emergence of the anterior perforating branch of peroneal artery through the interosseous membrane (arrow and circle). (D) Incision of the superior border of the flap and identification, transection, and inclusion of superficial peroneal nerve in the flap (circle). (E) Dissection of the lateral intermuscular septum between the extensor digitorum longus and peroneus brevis muscles detached from the fibula. (F) After confirmation of retrograde supply from the anterior tibial artery, ligation of the anterior perforating branch of peroneal artery just proximal to the bifurcation (arrow and circle). (G, H) Further elevation of the skin paddle until the distal communication with anterior tibial artery, and confirmation of flap reach by transposition onto the defect. (I) Final inset and skin graft cover over flap donor site and pedicle.
Limitations
This study had some limitations. This study was conducted at a single institute with 10 patients with the follow-up showing good functional as well as aesthetic recovery. While this surgical method is regarded as one of the best for treating patients with distal foot defects, a larger study population will be more helpful in determining whether this surgical procedure will be applicable in a diverse clinical scenario.
Conclusions
The distally based islanded lateral supramalleolar fasciocutaneous flap provides reliable cover for distal dorsal foot and ankle defects of moderate size. It can reach as far as the base of the toes with good wound healing and without major complications. It can be applied safely in all age groups and is safe following acute trauma. Islanding the flap makes it a single-stage procedure. It can be used as a lifeboat or even a substitute or alternative to free flaps.
Notes
Author contributions
Conceptualization: RKKG, LP, SP; Data curation: RKKG, LP, SP; Formal analysis: RKKG, LP, SP; Investigation: RKKG, LP, SP; Methodology: RKKG, LP, SP; Project administration: RKKG, LP, SP; Visualization: RKKG, LP, SP; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
The authors did not receive any financial support for this study.
Data availability
Data of this study are available from the corresponding author upon reasonable request.