Pneumoperitoneum from vaginal cuff dehiscence following blunt trauma in a patient with a history of robotic hysterectomy in Korea: a case report
Article information
Abstract
Pneumoperitoneum usually presents as a surgical emergency, especially in patients with a history of trauma. However, we recently encountered an atypical case of pneumoperitoneum at a hysterectomy site following blunt trauma, indicating that immediate laparotomy may not always be necessary. In this report, we present the case of a 45-year-old woman who was transferred to our trauma center from a local hospital after being involved in a traffic accident the day before. Although she underwent an emergency laparotomy, no bowel perforation was detected. Instead, a rupture was found at the site of a hysterectomy that had been performed 8 months earlier. After repairing the hysterectomy site, the pneumoperitoneum resolved, and the patient was subsequently discharged without further complications.
INTRODUCTION
Pneumoperitoneum usually results from bowel perforation, which typically necessitates an emergency laparotomy [1]. Although there have been reports of nonsurgical pneumoperitoneum, emergency laparotomy is still required when patients present with abdominal pain. Nonsurgical pneumoperitoneum usually originates from thoracic or abdominal sources, with genitourinary causes being relatively rare [2]. There have also been instances of trauma-induced nonsurgical pneumoperitoneum; however, laparotomy is often performed to rule out gastrointestinal perforation [3]. In this study, we present a recent case of pneumoperitoneum that developed following blunt trauma at the site of a previous hysterectomy.
CASE REPORT
A 45-year-old woman was transferred to Southern Gyeonggi Trauma Center, Ajou University Hospital (Suwon, Korea) following the detection of pneumoperitoneum on a computed tomography (CT) scan (Fig. 1). She had been involved in a taxi accident and was wearing her seat belt correctly at the time of the incident. However, she did not seek immediate medical attention after the rear-end collision. The following day, she began to experience abdominal pain and subsequently visited a local hospital.
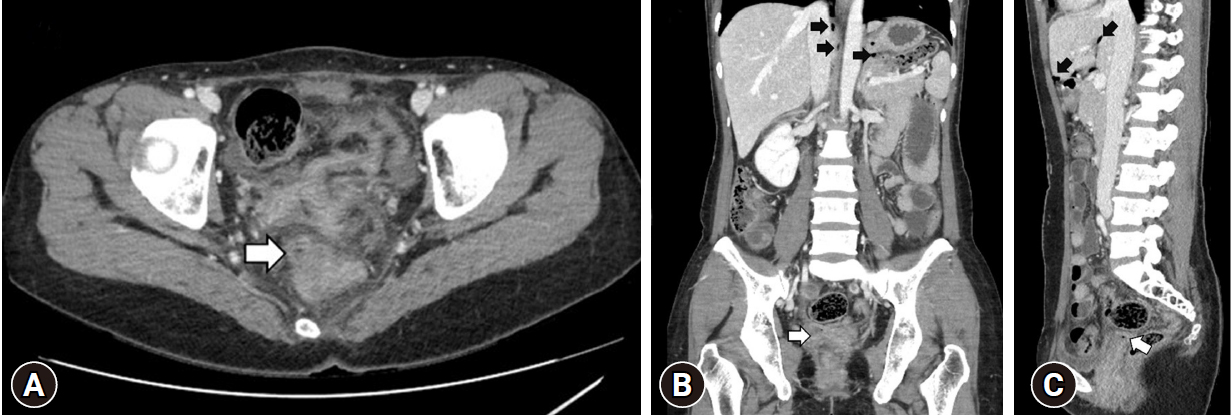
Computed tomography findings of vaginal cuff dehiscence. (A) Axial image, showing vaginal cuff dehiscence (arrow). (B) Coronal reconstruction image, showing the injury site (white arrow) and pneumoperitoneum (black arrows). (C) Sagittal reconstruction image, showing the injury site (white arrow) and pneumoperitoneum (black arrows).
Her medical history was unremarkable, except for a robotic hysterectomy performed 8 months prior due to uterine adenomyosis. Laboratory findings revealed leukocytosis with a white blood cell count of 17,330/µL and a normal hemoglobin level of 13.8 g/dL. A CT scan confirmed the presence of pneumoperitoneum, prompting her transfer to our trauma center. Upon arrival, she exhibited generalized abdominal tenderness, which necessitated an emergency laparotomy. Although no bowel perforation was detected during the surgery, contusions on the small bowel were noted. The primary issue identified was a ruptured hysterectomy wound, which was the cause of the pneumoperitoneum (Fig. 2). The wound was surgically repaired, and a drain was inserted. Antibiotics were administered in response to the presence of abdominal exudates. The drain showed no evidence of bile, and the patient's white blood cell count returned to normal within 2 days. She was discharged on the 10th postoperative day without any complications.

Surgical findings of vaginal cuff dehiscence, with the opening site into the area of vaginal cuff dehiscence (arrow).
Ethics statement
The patient provided written informed consent for publication of the research details and clinical images.
DISCUSSION
Pneumoperitoneum, a serious posttrauma finding, may arise from nonsurgical causes such as pneumothorax, rib fractures, or lower extremity fractures. Nevertheless, it is critical to prioritize an emergency surgical approach when indicated [3]. If a patient presents with abdominal pain or exhibits a seatbelt sign, a laparotomy should be conducted without delay [4]. In this case, an emergency laparotomy was carried out. Although the procedure might have appeared unnecessary due to the minimal damage found, the decision was justified, as the patient's symptoms should always drive the decision-making process for performing a laparotomy. It is worth noting that the repair of the vaginal cuff wound was successful.
Identifying the exact source of air entry into the abdomen can be challenging, even after a negative laparotomy for trauma-related pneumoperitoneum [2–5]. Suspected sources of air entry into the abdomen may be undiagnosed. In this case, however, the patient had no other injuries or definitive signs of wound rupture that would indicate pneumoperitoneum.
Nonsurgical pneumoperitoneum can be categorized into five groups: pseudopneumoperitoneum, abdominal, thoracic, gynecologic, and miscellaneous causes [2]. Gynecologic causes are relatively rare and typically involve the introduction of air through the genital tract. There have been several documented instances of pneumoperitoneum occurring after a hysterectomy, often in association with coitus [6–9]. Vaginal cuff dehiscence, which can be precipitated by coitus, is a known cause of pneumoperitoneum. Although it was unclear whether the patient had engaged in coitus, seatbelt injuries have been known to elevate the intra-abdominal pressure, which could lead to the breakdown of a vaginal wound. In the case presented, the surgical repair of the vaginal cuff dehiscence resulted in an improvement of symptoms.
In conclusion, a hysterectomy site may act as a source of pneumoperitoneum, although this is very infrequent. When assessing cases of pneumoperitoneum, surgical causes should be prioritized, with vaginal inspection considered only after other potential causes have been excluded following a hysterectomy.
Notes
Author contributions
Conceptualization: all authors; Methodology: all authors; Project administration: all authors; Visualization: all authors; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
The authors did not receive any financial support for this study.
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
