Percutaneous two unilateral iliosacral S1 screw fixation for pelvic ring injuries: a retrospective review of 38 patients
Article information
Abstract
Purpose
Percutaneous iliosacral (IS) screw fixation for pelvic ring injuries is a minimally invasive technique that reduces the amount of blood loss and shortens the procedure time. Moreover, two unilateral IS S1 screws exhibit superior stability to a single IS screw and are also safer for neurological injuries than an S2 screw. Therefore, this study aimed to evaluate fixation using percutaneous two unilateral IS S1 screws for pelvic ring injuries and its subsequent clinical outcomes.
Methods
We retrospectively reviewed 38 patients who underwent percutaneous two unilateral IS S1 screw fixation for pelvic ring injuries. The procedure time, blood loss, achievement of bone union, radiological outcomes (Matta and Tornetta grade), and postoperative complications were evaluated.
Results
The mean procedure time, hemoglobin loss, bone union rate, and time to union were 40.1 minutes (range, 18–102 minutes), 0.6 g/dL (range, 0.3–1.0 g/dL), 100%, and 153.2 days (range, 61–327 days), respectively. The Matta and Tornetta grades were excellent, good, and fair in 24 (63.1%), 11 (28.9%), and three patients (7.9%), respectively, and the postoperative complications were S1 screw loosening, widening of the symphysis pubis (2.3 and 2.5 mm), lumbosacral plexopathy, and S1 radiculopathy in one (2.6%), two (5.3%), one (2.6%), and one patient (2.6%), respectively. However, all neurological complications recovered spontaneously.
Conclusions
Percutaneous two unilateral IS S1 screw fixation was useful for treating pelvic ring injuries. In particular, it involved a short procedure time with little blood loss and also led to 100% bone union and good radiological outcomes.
INTRODUCTION
Percutaneous iliosacral (IS) screw fixation for pelvic ring injuries is a minimally invasive technique that more effectively reduces blood loss and operative time than the open reduction technique [1–3]. Thus, it has several advantages, particularly in patients with unstable hemodynamic conditions. However, the use of one IS screw is inferior with respect to rotational stability and load cycles [4,5]. Therefore, the fixation of two unilateral IS S1 screws or the addition of an IS S2 screw is recommended in completely unstable pelvic ring injuries [4]. Among these two procedures, the fixation of two unilateral IS S1 screws can be a reasonable option for unstable pelvic ring injuries, considering that IS screw positioning in S1 is safer in iatrogenic neurological injuries than IS screw positioning in S2 [6].
However, limited data have been reported on the clinical outcomes of two unilateral IS S1 screw fixation. Only one study has evaluated the functional and radiological outcomes of two unilateral IS S1 screw fixation and compared them with the outcomes of single IS S1 screw fixation [7]. Moreover, no other studies have evaluated the clinical outcomes of two unilateral IS S1 screw fixation. Therefore, this study aimed to retrospectively review patients who underwent percutaneous two unilateral IS S1 screw fixation and evaluate their clinical outcomes.
METHODS
This study was a retrospective review of a prospectively collected cohort at a level 1 trauma center, Korea University Guro Hospital and approved by the Institutional Review Board of the Korea University Guro Hospital (No. 2021GR0439).
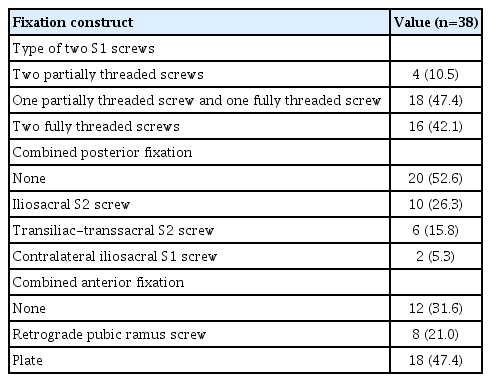
Patients
In total, 221 patients who underwent surgery for unstable pelvic ring injuries from May 2012 to May 2021 were reviewed. The inclusion criteria for these patients were as follows: (1) fixation of two ipsilateral IS S1 screws (7.3 or 7.0 mm); (2) fixation procedure performed percutaneously under two-dimensional fluoroscopic guidance; (3) at least a 1-year postoperative follow-up; and (4) available medical charts and radiographs to review exact data. Of the 221 patients, 38 patients were included in the analysis. Table 1 shows the included patients’ demographic data, and Table 2 shows the fixation constructs of the included patients.
Surgical technique
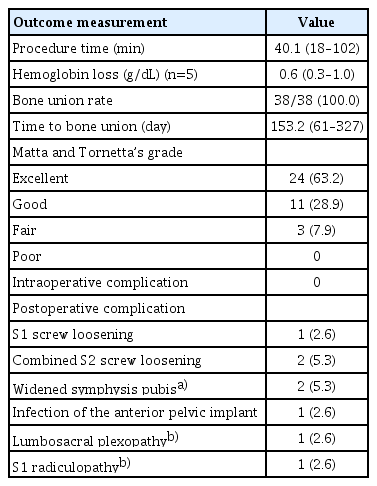
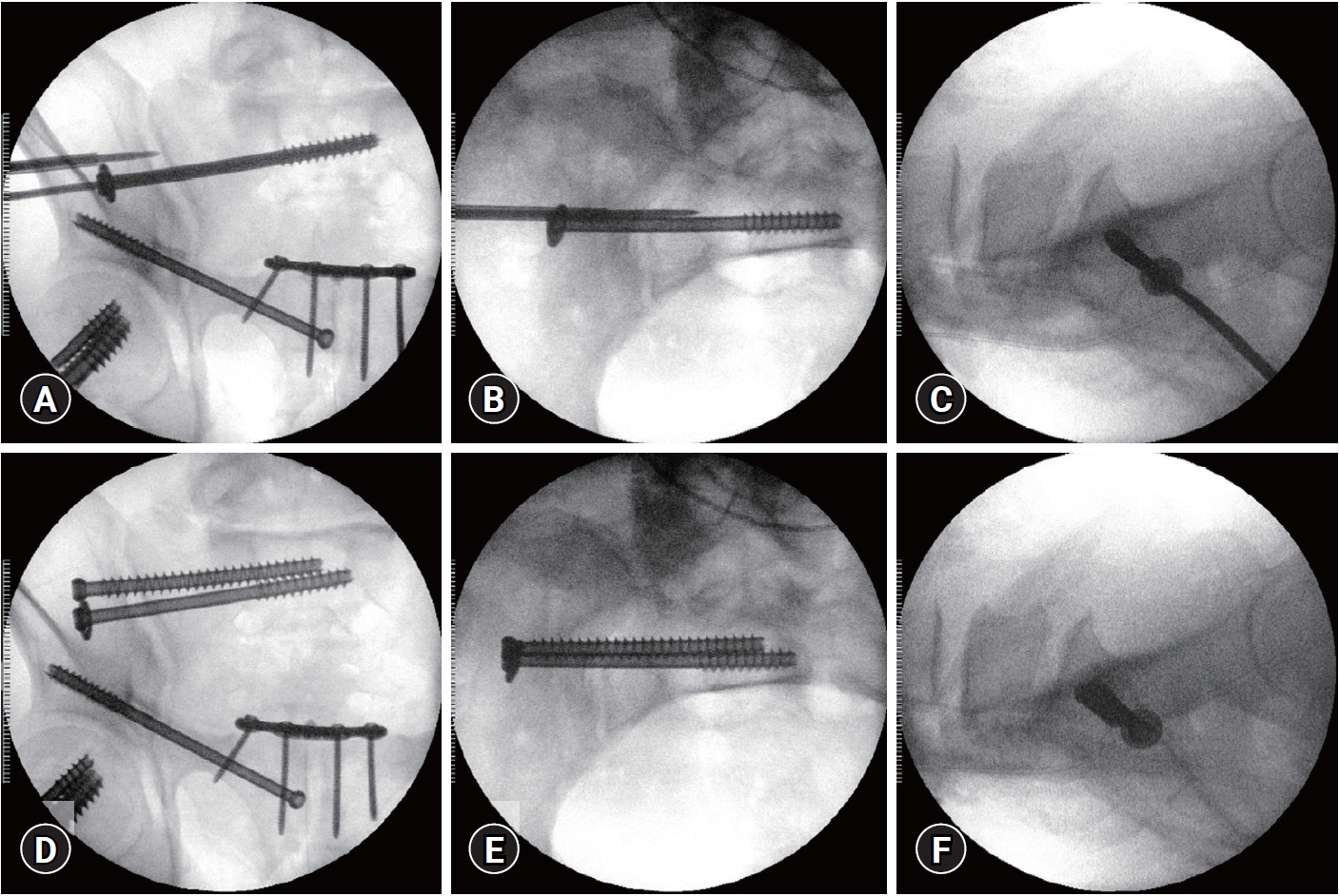
Before surgery, we measured the inlet angle, which is tangent to the anterior cortex of S1, and the outlet angle, which is perpendicular to the midline of the trapezoidal S1 body, using a midline sagittal computed tomography (CT) image (Fig. 1A). Based on the measured angles and fluoroscopic findings, we accurately determined the angle of the inlet and outlet views. The inlet view visualized the anterior cortex of the S1 body and spinal canal, whereas the outlet view visualized the sacral foramen (Fig. 2A). Lines perpendicular to the determined inlet and outlet angles were drawn on the patient along with the line of iliac cortical density (ICD), which could be confirmed in the true lateral view (Fig. 1B). Surgery was then performed on a radiolucent operating table, and the patient was prepared in the supine position. The entry of the first guide pin was made anterior in S1 and inferior to ICD. The height of the entry and coronal direction of the guide pin were determined via the outlet view, and the anterior-posterior position and direction were determined through the inlet view (Fig. 2B, C). The drawn perpendicular line of the determined inlet and outlet angles helped modify the position of the guide pin entry and direction of the guide pin. For example, if the guide pin position or direction needed modification in the outlet view, moving the pin along the line drawn perpendicular to the outlet angle could modify the position or direction of the pin effectively in the outlet view. After making the accurate position of entry and direction, we advanced the guide pin. The guide pin was advanced cranial to the S1 foramen in the outlet view and near the anterior cortex, but within it, in the inlet view (Fig. 2D, E). After passing the S1 foramen, the true lateral view was used to confirm that the ICD had not been penetrated, and the guide pin was then advanced to the S1 body (Fig. 2F). Finally, reaming was performed, and a cannulated screw with a washer was inserted via the guide pin. When tightening the screws, the obturator inlet view was used to confirm the narrowing of the sacroiliac joint gap, thereby confirming the precise state of the screw head and washer to prevent excessive intrusion (Fig. 2G–I). The second unilateral IS screw was fixed whenever possible; however, if the safe corridor was not sufficiently wide and pelvic dysmorphism was observed, the second screw was not used. The guide pin of the second screw was inserted; the guide pin of the first screw was not removed because it helped to guide the direction of the second guide pin (Fig. 3A). The second guide pin was positioned cranial to the first screw in the outlet view and positioned in a manner that did not penetrate the anterior cortex or the spinal canal in the inlet view and ICD in the lateral view (Fig. 3A–C). As a result, the second guide pin usually overlapped with or was slightly posterior to the first screw. The interval between the first screw and the second guide pin was at least half of the screw diameter to prevent collision between the screws. After confirming the adequate position of the second guide pin, the second screw was inserted (Fig. 3D–F). The type of screws was selected based on the need for compression. If compression was not required or overcompression needed to be avoided, a fully threaded screw was fixed. If compression was required, a partially threaded screw was fixed. Moreover, if additional compression was required after the first partially threaded screw fixation, the second screw was also selected for the partially threaded screw. A washer was routinely applied.

Computed tomography image and clinical photograph of the preoperative preparation. (A) The measured inlet angle is tangent to the anterior cortex of S1 (dotted line I) and the outlet angle is perpendicular to the midline of the S1 body (dotted line O). (B) The drawn lines are perpendicular to the determined inlet (line I') and outlet angles (line O'); and the drawn dotted lines are determined inlet angle (dotted line I) and outlet angle (dotted line O). The patient provided written informed consent for publication of the research details and clinical images.

Fluoroscopic images of the first iliosacral screw procedure. (A) Image of the outlet view visualizing the S1 foramen and determining the height of entry and coronal direction of the guide pin. The dotted line indicates the right S1 foramen. (B) Inlet view visualizing the anterior cortex of the S1 body and spinal canal and determining the anterior-posterior position and direction of the guide pin. The dotted lines indicate the anterior cortex of the S1 body, and the lines indicate the spinal canal. (C) Lateral view showing the iliac cortical density (ICD) line. The dotted lines indicate the ICD. (D) Outlet view showing that the guide wire should be cranial to the S1 foramen. (E) Inlet view showing that the guide wire should not penetrate the anterior cortex or the spinal canal. (F) Lateral view demonstrating that the guide wire is not penetrating the ICD after passing the S1 foramen. (G, H) Outlet and oblique inlet views show the sacroiliac joint gap and precise state of the screw and washer before tightening of the screw. (I) Oblique inlet view demonstrates both a compressed sacroiliac joint and an unintruded screw head and washer into the ilium. The patient provided written informed consent for publication of the research details and clinical images.
Fluoroscopic images of the second iliosacral screw procedure. (A) Outlet view showing that both the first and second screws are cranial to the S1 foramen and that the first guide pin was not removed to help guide the first guide pin. (B) Inlet view showing that the second guide pin is not penetrating the anterior cortex or the spinal canal. (D) Lateral view showing that the second guide pin is not penetrating the iliac cortical density line. (E, F) Final position of the second iliosacral screw. The patient provided written informed consent for publication of the research details and clinical images.
Postoperative management
All patients were instructed to perform a hip joint range of motion exercise and quadriceps strengthening exercises immediately after surgery. Furthermore, “toe-touch” weight-bearing to partial weight-bearing immediately after surgery was initially advised to patients with vertically stable injuries. However, patients with vertically unstable injuries started partial weight-bearing 4 to 6 weeks postoperatively. Thereafter, we progressively increased the amount of weight-bearing according to patients’ tolerance. The patients were followed up at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively.
Outcome measurements
The procedure time was evaluated using fluoroscopic data. Because all procedures were performed under fluoroscopic guidance, we could determine the exact start and end times of the procedure using fluoroscopic data. If surgery involved only percutaneous two ipsilateral S1 screw fixation with intraoperative transfusion, blood loss was evaluated using hemoglobin (Hb) loss between the preoperative and postoperative periods. Intraoperative complications (e.g., guide wire breakage) were also evaluated. Bone union was defined as the absence of a fracture line. In addition, the time to union was evaluated. Moreover, we measured radiological outcomes using the method of Matta and Tornetta [8]; reductions were graded as excellent (<4 mm), good (5–10 mm), fair (11–20 mm), and poor (>20 mm) using maximal displacement measured on the three standard radiographic views of the pelvis. The bone union and radiographic outcomes were determined by a consensus of two orthopedic trauma fellowship-trained independent observers who were blinded to clinical information. Finally, several postoperative complications, including reduction loss, implant loosening or failure, neurological complication, and infection, were evaluated.
RESULTS
The mean procedure time was 40.1 minutes (range, 18–102 minutes). Blood loss was evaluated in five patients, and the mean Hb loss was 0.6 g/dL (range, 0.3–1.0 g/dL). There were no intraoperative complications. Bone union was achieved in all 38 patients; hence, the bone union rate was 100%. The mean time to union was 153.2 days (range, 61–327 days). The Matta and Tornetta grades were as follows: excellent in 24 (63.2%), good in 11 (28.9%), fair in three (7.9%), and poor in zero patients. S1 screw loosening was observed in one patient, combined S2 screw loosening in two patients, widening of the symphysis pubis (2.3 and 2.5 mm) in two patients, and infection of the anterior pelvic implant in one patient. Moreover, lumbosacral plexopathy was observed in one patient and S1 radiculopathy in one patient; however, all cases recovered spontaneously (Table 3, Fig. 4).
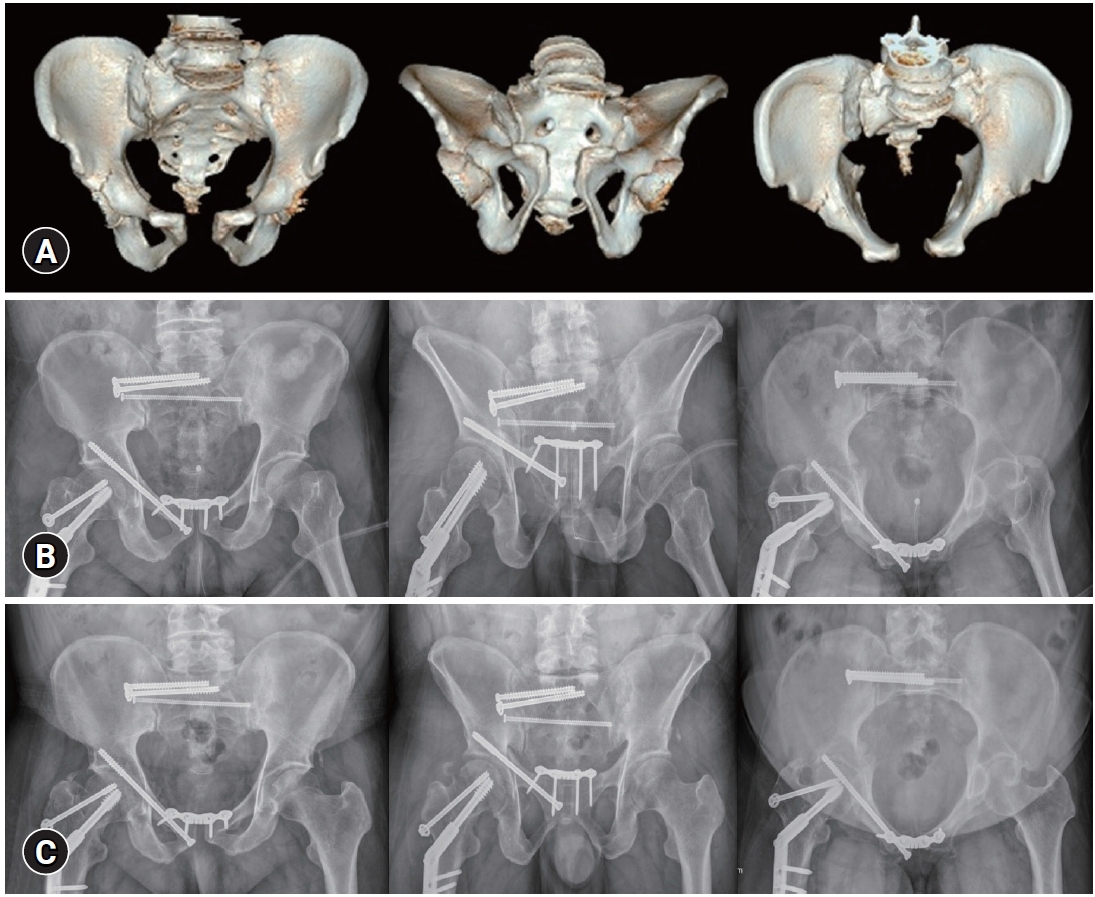
A 46-year-old male patient suffered from an anterior-posterior compression type III pelvic ring injury after a crushing injury with an Injury Severity Score of 9. (A) Preoperative three-dimensionally reconstructed computed tomography images (anteroposterior [AP], outlet, and inlet). (B) Immediate postoperative plain radiographs (AP, outlet, and inlet) after percutaneous two ipsilateral iliosacral S1 screw fixation, transiliac-transsacral S2 screw fixation, retrograde pubic ramus screw, and anterior plate fixation. Percutaneous two ipsilateral iliosacral S1 screw fixation required 30 minutes, and no intraoperative complications were observed. (C) Follow-up plain radiographs (AP, outlet, and inlet) 97 days postoperatively. Radiographs showed bone union, and the outcomes were excellent according to the Matta and Tornetta grade. However, widening of the symphysis pubis (<2.5 mm) was noted. The patient provided written informed consent for publication of the research details and clinical images.
DISCUSSION
The present study demonstrated that percutaneous two unilateral IS S1 screw fixation for pelvic ring injuries required a mean procedure time of 40.1 minutes and led to a mean Hb loss of 0.6 mg/dL during the procedure, a union rate of 100%, and an excellent to good radiological grade of 92.1%.
The biomechanical analysis of IS screws has been performed in several studies. Yinger et al. [9] compared nine different posterior pelvic ring fixation methods on hard plastic pelvic models, and the results revealed that two unilateral IS S1 screws were significantly stiffer in horizontal plane gapping and coronal plane rotation than single IS S1 screws, two anterior sacroiliac plates, one posterior pelvic tension band plate, one posterior pelvic tension band plate combined with one IS S1 screw, two transiliac bars, two transiliac bars combined with an IS screw, and one transiliac bar with one IS S1 screw. van Zwienen et al. [4] compared two unilateral IS S1 screws and a single IS S1 screw in a type C pelvic ring injury cadaveric model. The results showed that the two unilateral IS S1 screws were significantly stiffer in terms of rotation and load to failure than a single IS S1 screw. Moreover, Salari et al. [10] compared two unilateral IS S1 screws and one IS S1 screw with a transsacral S1 screw in a type C pelvic ring injury cadaveric model. They concluded that although a transsacral screw may appear to be more stable, the use of two long unilateral IS SI screws yielded adequate stability in a single-limb stance-testing model compared with transsacral S1 screws. These studies demonstrated the usefulness of two unilateral IS S1 screws with respect to mechanical stability.
Only one study, however, has evaluated the clinical outcomes of two unilateral IS S1 screws to date. The authors compared radiological outcomes via the Matta and Tornetta grade and functional outcomes using the Majeed scoring system. Although the outcomes of both groups were comparable to those of other studies with respect to pelvic ring injuries, the outcomes showed no statistically significant differences between the two groups [7]. However, they did not report patient-related variables (e.g., age, fracture type, or combined injury) of each group and their differences. Therefore, selection bias could not be excluded with regard to the results of the previous study [7]. Suda et al. [5] recently evaluated the safety of two unilateral IS S1 screws in a three-dimensional dataset of 1,000 hemi-pelvises of 500 patients with trauma. They concluded that 99% of male and 96% of female hemi-pelvises had adequate room to place two 7.3-mm screws at a 5-mm distance into the S1 vertebra. In addition, they stated that two unilateral IS S1 screws increased the mechanical stability and posed a lower risk for neurological injuries than the positioning of additional S2 screws.
In the present study, the mean procedure time of percutaneous two unilateral IS S1 screw fixation was 40.1 minutes, which is comparable to the procedure time in previous studies that used a single IS screw. Routt et al. [11] reported that one percutaneous IS screw required a mean procedure time of 26 minutes, implying that 2-screw fixation would require a mean time of 52 minutes. Gras et al. [12] reported a mean time of 62 minutes for one percutaneous screw fixation for pelvic ring injury. Although positioning the second IS S1 screw to avoid the first IS S1 screw can be intuitively difficult and may need a longer time, it did not require more time in the present study. Thus, two unilateral IS S1 screws still have the advantage of a short procedure time for performing the percutaneous IS screw technique. We evaluated blood loss by measuring the decrease in Hb levels between the preoperative and postoperative periods, although most other studies utilized intraoperative blood loss volume. Because intraoperative blood loss volume cannot be evaluated objectively and is often estimated, we used Hb loss instead. The mean Hb loss of 0.6 g/dL was small, which is beneficial for hemodynamically unstable patients. Moreover, all patients showed bone union, and bone union required a mean duration of 153.2 days. These results are comparable to those of other studies that used percutaneous IS screws or open reduction and plate fixation [12–14]. The results of the Matta and Tornetta grades were also comparable to or better than those of other studies. Matta and Tornetta et al. [8] reported an excellent grade in 67% of patients, good in 28%, fair in 4%, and poor in 1%. In addition, Suzuki et al. [15] reported an excellent grade in 51% of patients, good in 23%, fair in 16%, and poor in 10%. Furthermore, Khaled et al. [7] reported an excellent grade in 71.4% of patients, good in 20.8%, fair in 7.8%, and poor in none. There were no intraoperative complications; however, eight patients developed postoperative complications. In particular, S1 screw loosening (2.6%), widening of the symphysis pubis (5.3%), lumbosacral plexopathy (2.6%), and S1 radiculopathy (2.6%) were directly related to two unilateral IS S1 screws. Moreover, all neurological deficits recovered spontaneously; the 2.3- and 2.5-mm widenings of the symphysis pubis after surgery were relatively smaller than the mean values in previous studies [16–19]. The results for complications are also comparable to the findings of a study on a single IS screw; Osterhoff et al. [1] performed percutaneous single IS screw fixation on the S1 or S2 vertebrae in 38 patients and reported persistent hypoesthesia in L5/S1 dermatomes in two patients (5.3%); screw malpositioning or loosening, which needed secondary surgery, in four (10.5%); pulmonary embolism in one (2.6%); and nonunion in one (2.6%). Zwingmann et al. [20] evaluated the intraoperative and postoperative complications of the CT guidance and conventional technique groups for percutaneous IS screws in 784 patients and reported intraoperative and postoperative complications in 8.8% and 26.3% of patients in the CT guidance group and 5.9% and 29.3% of patients in the conventional technique group, respectively. Therefore, in this study, percutaneous two unilateral IS S1 screw fixation required a short procedure time and showed a small amount of blood loss, 100% bone union rate, comparatively good radiological outcomes, and few complications.
The limitations of this study are the retrospective study design and small number of cases, particularly for the outcome of Hb loss. In addition, this study was a case series and did not include a control group. Moreover, the outcomes of this study included many variables that were not controlled, including the initial fracture type or the fixation construct of the anterior pelvic ring. Thus, an additional study with a large number of cases and high power is needed.
In conclusions, percutaneous two unilateral IS S1 screw fixation is a useful option for pelvic ring injuries. In particular, the procedure requires less time and causes little blood loss, as well as leading to a 100% bone union rate and good radiological outcomes.
Notes
Ethical statement
This study was a retrospective review of a prospectively collected cohort at a level 1 trauma center, Korea University Guro Hospital and approved by the Institutional Review Board of the Korea University Guro Hospital (No. 2021GR0439). Written informed consent was waived due to the retrospective nature of this study.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: WSS, JWC, JKO; Data curation: HJK, NYK; Formal Analysis: NJC; Investigation: JMC; Methodology: JMC, NJC; Project administration: JKO, NYK; Resources: JKO; Software: WSS; Supervision: CWC, HJK; Validation: HJK; Visualization: WSS; Writing–original draft: WSS; Writing–review&editing: WSS, HJK, JWC, JKO.
All authors read and approved the final copy of the manuscript.