Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(2); 2022 > Article
-
Case Report
Acute pyomyositis of the adductor magnus muscle involving the posterior and lateral thigh compartments: a case report of diagnosis and management -
Rajesh Bawale, FRCS
 , Jay Watson, FRCS
, Jay Watson, FRCS , Karshe Yusuf, MRCS
, Karshe Yusuf, MRCS , Dilip Pillai, FRCS
, Dilip Pillai, FRCS , Bijayendra Singh, FRCS
, Bijayendra Singh, FRCS
-
Journal of Trauma and Injury 2022;35(2):139-143.
DOI: https://doi.org/10.20408/jti.2021.0022
Published online: May 26, 2022
- 2,125 Views
- 39 Download
- 1 Crossref
Department of Trauma and Orthopaedics, Medway Maritime Hospital, Windmill Road, UK
- Correspondence to Rajesh Bawale, FRCS Department of Trauma and Orthopaedics, Medway Maritime Hospital, Windmill Road, Gillingham, Kent ME7 5NY, UK Tel: +44-7387-675218 E-mail: rajesh.bawale@nhs.net
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Bacterial infection of skeletal muscle can lead to the formation of abscesses. Primary pyomyositis is typically seen in tropical countries, and Staphylococcus aureus is the commonest causative organism. We present a case of acute adductor magnus muscle abscess (pyomyositis) with spread to adjacent thigh compartments via the perforators without iliopsoas muscle involvement. Due to the involvement of the entire thigh compartment, systemic antibiotic treatment alone was insufficient, whereas surgical drainage improved the clinical picture. The aetiological organism was S. aureus. Herein, we report the case of a patient who had primary pyomyositis, rather than a secondary type, that spread to the posterior and lateral aspect of the thigh through the second and third perforators, which pierce the adductor magnus muscle belly before entering the femur.
- We present a case of acute adductor magnus muscle abscess (pyomyositis) with spread to adjacent thigh compartments via perforators without iliopsoas muscle involvement. We also discuss the differential diagnosis and principles of management.
INTRODUCTION
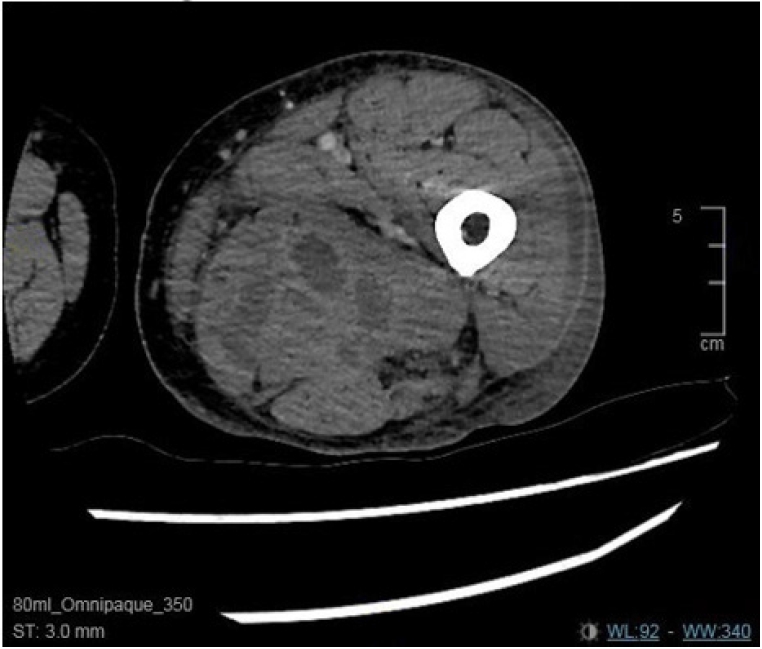
- A 59-year-old male patient presented to the emergency department with sepsis in the evening. The clinical examination noted left thigh pain associated with reduced movement and left lower leg swelling. The patient reported nontraumatic, sudden-onset left thigh pain and swelling, with a reduced range of movement in the hip/knee and inability to bear weight. On examination, he had a palpable swelling over the medial aspect of the left proximal thigh and a skin induration over the lateral aspect. His body temperature was 38.9°C, he had hypotension, and he showed confusion with facial flushing. He had a background of multiple sclerosis and autoimmune skin conditions, and he was on long-term high-dose prednisolone. On radiographs of the left thigh, soft tissue shadows were noted, and a complete blood count showed an elevated white cell count and a C-reactive protein (CRP) level of 625 mg/L. The differential diagnoses were iliopsoas abscess with spread to the adductor muscles and necrotising fasciitis. Blood cultures were taken, the patient was resuscitated with fluids, a urinary catheter was inserted, the intensive treatment unit team was involved, and the patient was kept nil by mouth and was sent for an urgent computed tomography (CT) scan of the left hip/thigh and pelvis to confirm the diagnosis. The CT scan showed multiple pockets of intramuscular abscesses in the belly of the adductor magnus muscle; no iliopsoas abscess or any communication with the iliopsoas was noted (Figs. 1–3). The CT scan did not show any collection of pus in the posterior and lateral thigh compartments. Due to the patient’s high temperature and very high CRP levels, a decision was made to take the patient to the emergency operating room on the same evening/night, and the patient was placed on the emergency operating room list. The patient and his next of kin received an explanation about the patient’s clinical status, laboratory results, the CT scan report (Figs. 1, 2), and the planned surgery (exploration and drainage of the collection).
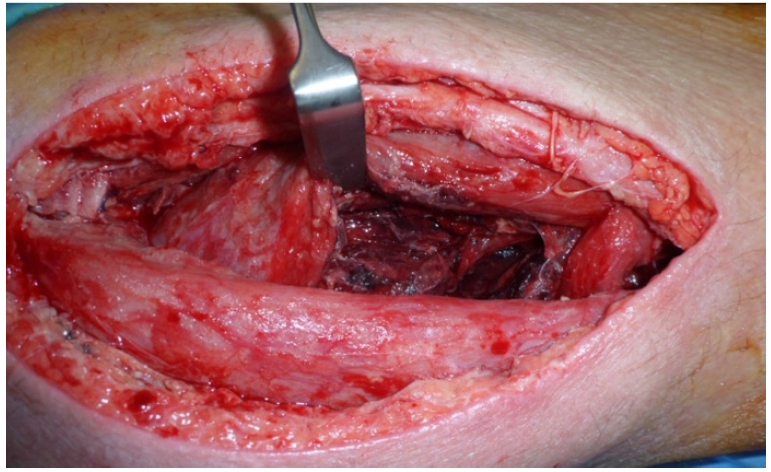
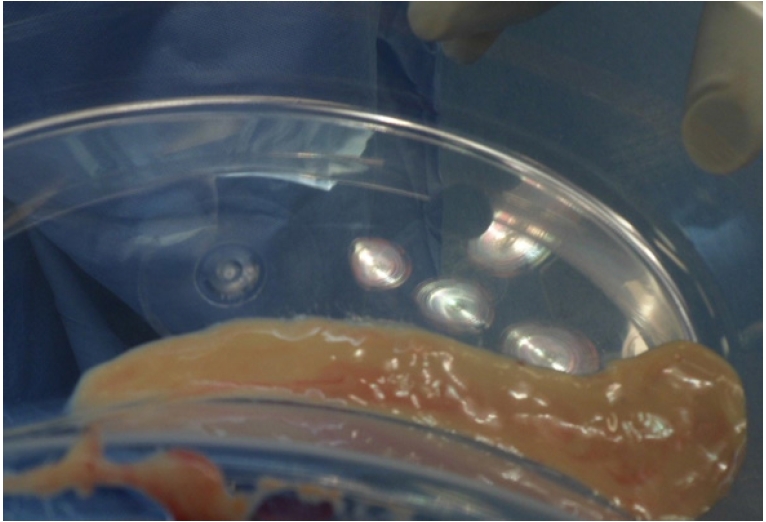
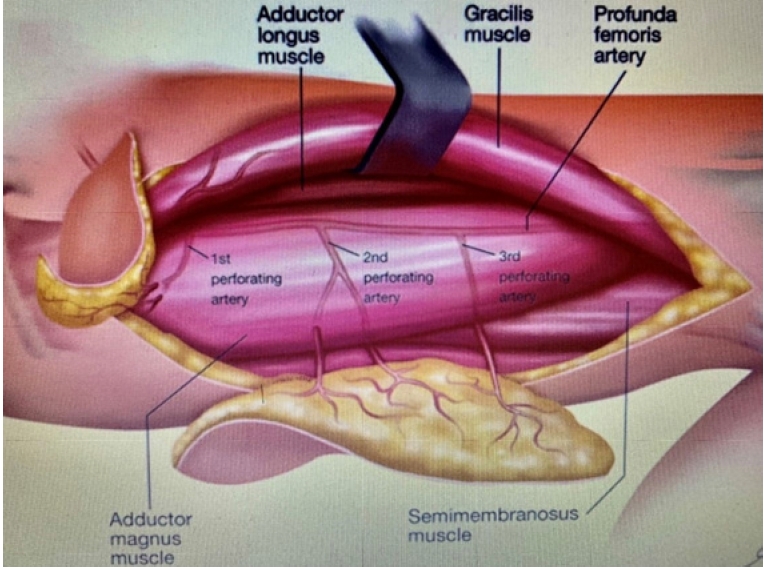
- A direct medial approach was performed posterior to the adductor longus, and the adductor magnus muscle belly was approached (Fig. 4). Blunt dissection revealed an intramuscular pus collection (approximately 50 mL) that was sent for an urgent microbiological examination (Gram stain, culture, and sensitivity). Even though the CT scan did not show any collection, the skin induration over the lateral aspect of the thigh prompted us to perform needle aspiration, which showed frank pus. Approximately 10 mL of pus collection was noted around the adductor magnus muscle attachment with the femur and tracked to the anterolateral aspect of the thigh, which was approached using two direct lateral incisions, as marked in Fig. 5, and approximately 20 mL of pus was drained (Fig. 6). The spread from the adductor magnus muscle to the posterior and lateral compartments of the thigh was explained by the anatomy of the second and third perforators piercing the adductor magnus muscle before entering the femur (Fig. 7).
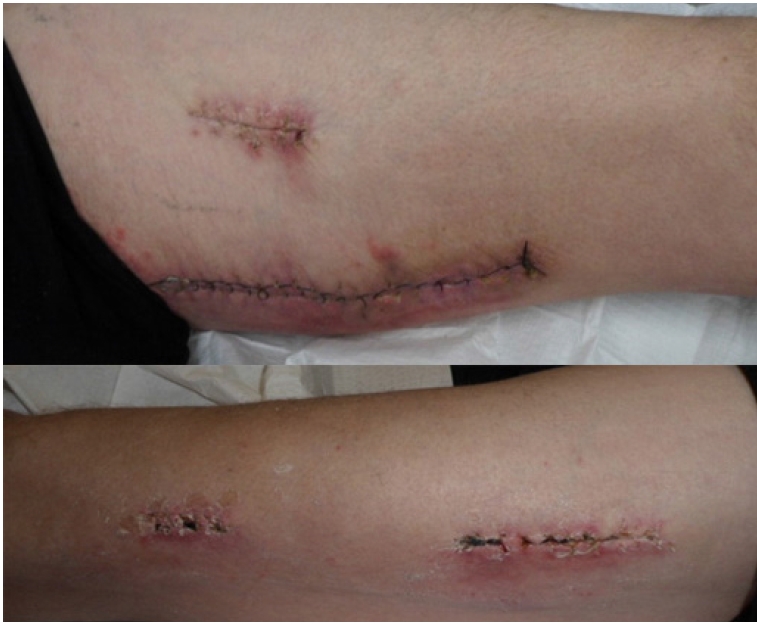
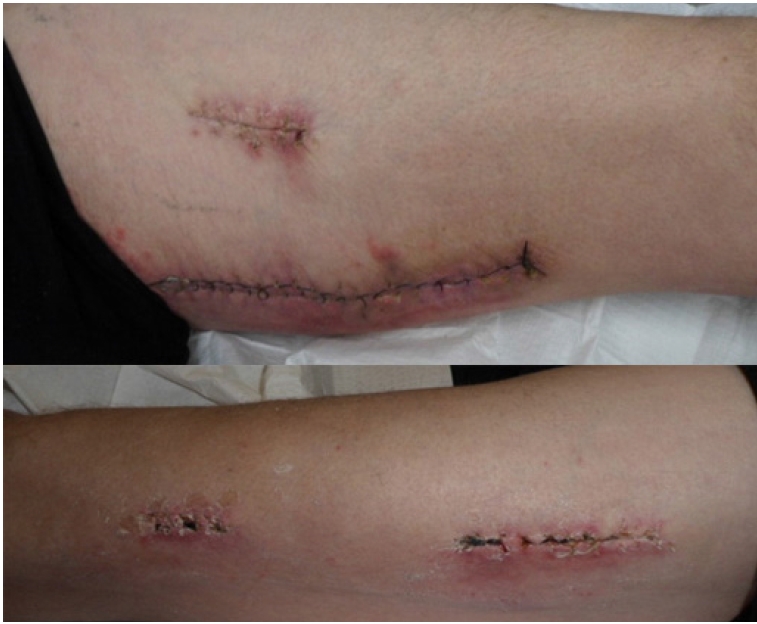
- A thorough washout was done and a vacuum dressing was applied (Fig. 8). The pus was sent for a microbiological examination. The Gram stain, culture, and sensitivity test showed Staphylococcus growth with sensitivity to flucloxacillin and metronidazole. Serial CRP examinations showed marked reductions in CRP levels, and the patient demonstrated clear clinical improvement. After four episodes of exploration and debridement, the wounds were closed (Fig. 9). Antibiotics were given intravenously during the hospital stay, a peripherally inserted central catheter line was inserted, and the patient was later discharged home with intravenous ceftriaxone (2 g, once a day) and oral metronidazole for 2 weeks.
- The patient showed consistent improvement and the wounds healed well. The patient was followed up until it was confirmed that he had recovered well. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
CASE REPORT
- Acute, isolated, spontaneous-onset adductor muscle abscesses are uncommon, as adductor muscle abscesses usually spread from the iliopsoas. The spread of infection to the posterior and lateral aspects of the thigh in this case is explained by the infection tracking along the second and third perforators, which pierce the adductor magnus muscle belly before entering the femur. The aetiology of acute muscle abscess is usually secondary to trauma, which is often trivial. Diabetes mellitus, steroid treatment, and immunodeficiency have been identified as predisposing factors [1]. In our case report, the patient was on long-term, high-dose oral prednisolone, which was the relevant predisposing factor. The clinical presentation of isolated adductor muscle abscess is variable and non-specific. Pyomyositis is relatively more common in children, and has an equal sex distribution. In rare cases, psoas abscesses can extend to the adductors [2]. Acute primary abscess or polymyositis is rare in the western world [3], and is more prevalent in tropical countries. Muscle abscesses secondary to intramuscular injections have been reported [4]. Staphylococcus aureus is the bacterium that is most commonly responsible for pyomyositis and was the responsible bacterium in our case. Other less commonly seen bacteria are group A streptococci and Staphylococcus pneumoniae. Unusual bacterial species include Escherichia coli, Salmonella typhi, Bacteroides fragilis, Neisseria gonorrhoeae, and Mycobacterium tuberculosis, and in some rare cases, muscle abscesses can be caused by fungal, parasitic, and viral agents [5].
- The diagnosis of muscle abscess is often difficult, and the differential diagnosis includes muscle strain, synovitis, tumour, septic arthritis, fracture secondary to trauma, osteomyelitis, inflammatory arthritis (rheumatoid arthritis, gout, psoriatic arthritis), and osteoarthritis. The clinical examination findings include a palpable mass, erythema, localised tenderness, reduced limb/joint movements, and associated low-grade fever, while rare complications include peripheral nerve palsy [6]. Our case report showed all of the above clinical findings except nerve palsy. The laboratory findings include raised white cell count and CRP levels, which were also noted in our case report. The blood cultures are usually positive and radiological investigations are the mainstay of diagnosis and treatment. Plain radiographs may show a soft tissue shadow, but a contrast CT scan, magnetic resonance imaging, or a gallium scan can show the underlying abscess findings [7,8]. The treatment of muscle abscess is drainage with the administration of intravenous antibiotics selected on the basis of culture and antibiotic sensitivity testing. Isolated adductor magnus muscle abscesses are uncommon, although they have been described with pathogens such as M. tuberculosis [9]. This case report highlights the importance of considering tuberculosis in the differential diagnosis of any unexplained soft tissue swelling in endemic areas. In our case report, the CT scan did not show any collection of pus in the posterior and lateral thigh compartments, or any communication with the iliopsoas muscle. The skin induration over the lateral aspect of the thigh prompted us to perform needle aspiration, which showed frank pus; based on this finding, we performed exploration and washout. With prompt diagnosis and management, a full recovery can be achieved with an excellent prognosis.
- The abscess in this patient was large and loculated inside the adductor magnus belly and its attachment with the femur. It spread to the posterior and lateral compartments of the thigh via the perforators, which pierce the adductor magnus muscle. A CT scan helped to make a definitive diagnosis and rule out an associated iliopsoas abscess. In this case, the CT scan did not show any collection of pus in the posterior and lateral thigh compartments; however, the skin changes over the lateral aspect of the thigh prompted us to perform needle aspiration, which showed frank pus. This led us to perform exploration and washout. The patient was treated successfully with emergency open surgical drainage and antibiotic therapy. Primary muscle abscess is a rare condition, but must be considered as a cause of leg/thigh/hip pain. We recommend a prompt clinical diagnosis with the use of imaging modalities, and urgent surgical exploration of suspected areas is the key to treat muscle abscesses.
DISCUSSION
-
Ethical statements
Informed consent for publication of the research details and clinical images was obtained from the patient.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: RB; Data curation: JW, KY; Project administration: RB, JW; Writing–original draft: RB; Writing–review & editing: RB, DP, BS.
All authors read and approved the final copy of the manuscript.
ARTICLE INFORMATION
- 1. Brown RL. Pyomyositis in patients with diabetes. Computed tomography as a key to diagnosis. Postgrad Med 1989;86:79–89. Article
- 2. Chalaupka FD. Acute iliopsoas and adductor brevis abscesses presenting with proximal leg muscle weakness. Neurol Sci 2006;27:125–8. ArticlePubMed
- 3. Christin L, Sarosi GA. Pyomyositis in North America: case reports and review. Clin Infect Dis 1992;15:668–77. ArticlePubMed
- 4. Harada K, Kashihara N, Iwamuro M, Otsuka F. Multiple abscesses caused by repetitive intramuscular injections. J Gen Fam Med 2017;18:301–2. ArticlePubMedPMC
- 5. Crum-Cianflone NF. Bacterial, fungal, parasitic, and viral myositis. Clin Microbiol Rev 2008;21:473–94. ArticlePubMedPMC
- 6. Pai VS, Yee E, Lawson D, Curtis G. Iliacus pyomyositis with involvement of lateral cutaneous nerve of the thigh. N Z Med J 1994;107:378–9. PubMed
- 7. Schiff RG, Silver L. Tropical pyomyositis. Demonstration of extent and distribution of disease by gallium scintigraphy. Clin Nucl Med 1990;15:542–4. PubMed
- 8. Struk DW, Munk PL, Lee MJ, Ho SG, Worsley DF. Imaging of soft tissue infections. Radiol Clin North Am 2001;39:277–303. ArticlePubMed
- 9. Arora S, Sabat D, Sural S, Dhal A. Isolated tuberculous pyomyositis of semimembranosus and adductor magnus: a case report. Orthop Surg 2012;4:266–8. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- Wheel of misfortune: A unique case of MRSA pyomyositis of the adductor muscle group from blunt unicycle trauma
Jordan I. Gaelen, Toluwalase Awoyemi, Emmanuel Okematti, Meera Ramanathan
Clinical Case Reports.2023;[Epub] CrossRef
 KST
KST





 PubReader
PubReader ePub Link
ePub Link Cite
Cite