Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(2); 2022 > Article
-
Original Article
The incidence of unexpected delays in uploading outside radiologic images in the transfer of patients with major trauma -
Si Jun Woo, MD
 , Yong Oh Kim, MD
, Yong Oh Kim, MD , Hyung Il Kim, MD
, Hyung Il Kim, MD
-
Journal of Trauma and Injury 2022;35(2):92-98.
DOI: https://doi.org/10.20408/jti.2021.0039
Published online: May 11, 2022
- 1,613 Views
- 43 Download
Department of Emergency Medicine, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- Correspondence to Hyung Il Kim, MD Department of Emergency Medicine, Dankook University Hospital, Dankook University College of Medicine, 201 Manghyang-ro, Dongnam-gu, Cheonan 31116, Korea Tel: +82-41-550-6840 E-mail: hilovesjj@naver.com
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Critically ill patients are frequently transferred from one point of care to a hospital that can provide a higher level of care. To achieve optimal treatment within the targeted window of time necessary for time-sensitive cases like major trauma, rapid transportation and decision making are essential. Transferred patients have often undergone radiologic imaging at the referring hospital. Examining these outside images is paramount. Therefore, this study was conducted to estimate the upload time of outside images.
-
Methods
- This retrospective study was conducted from January to April 2020. Patients transferred from other hospitals with digitally recorded CDs or DVDs of radiologic or diagnostic images were included. When the patients were registered at the emergency department reception desk, the digital images were transmitted to our picture archiving and communication system using transmission software. The time of upload and the numbers of digital images were recorded. The time interval from patient registration to the time of upload was calculated.
-
Results
- The median number of images was 688 in the trauma team activation (TTA) group (688 in the TTA group, 281 in the non-TTA trauma group, and 176 in the nontrauma group, respectively; P<0.001). The median upload time was 10 minutes. The longest upload time was 169 minutes. The upload time was more than 20 minutes in 12 cases (19.4%).
-
Conclusions
- Patients with major trauma bring more images than patients with other diseases. Unexpected delays (>20 minutes) were noted in approximately 20% of cases. It is necessary to minimize this time.
- Critically ill patients are frequently transferred to a hospital that can provide a higher level of care. Acute myocardial infarction (AMI), acute stroke, and major trauma are time-sensitive diseases and are also the three major categories of severe medical emergencies in Korea. For AMI, the recommended time from the first medical contact to percutaneous coronary intervention is 70 minutes (120 minutes including transfer time if the patient first visits a percutaneous coronary intervention noncapable institution) [1–3]. Fibrinolysis is recommended, when indicated, within 3 hours of symptom onset in acute ischemic stroke [4,5]. In major trauma, the concept of the “golden hour” or time from the accident to definitive care is important and the recommended allowed time in the field is less than 10 minutes [6,7].
- In recent years, cardiovascular centers or trauma centers have been established and helicopter emergency medical services (HEMS) have become available, reducing the mortality and complications of these diseases in Korea. Of the 389,269 AMI, acute stroke, and major trauma patients in 2019, 5.9% were transferred to other hospitals [8]. To achieve the right treatment at the right time for these time-sensitive diseases, rapid transportation and decision making are essential. Sometimes, the transferred patients have undergone radiologic imaging at the referring hospital. It is paramount that the physicians in the receiving hospital examine these outside images. Therefore, this study was conducted to estimate the upload time of outside images to our picture archiving and communication system (PACS; ViewRex 3, Techheim, Seoul, Korea).
INTRODUCTION
- This is a retrospective study conducted at Dankook University Hospital, an academic tertiary medical center in Korea. The approval from the Institutional Review Board and informed consents were not obtained due to the retrospective and observational nature of the study. The study period was from January to April 2020. Dankook University Hospital is a regional emergency center and level I trauma center where a physician-staffed HEMS is available. Emergency cardiac angiography and acute stroke care are available 24 hours per day, 7 days per week. Therefore, many patients are transferred to this institution. Approximately 42,000 patients visit the emergency department (ED) annually. During the study period, patients transferred from other hospitals with digitally recorded radiologic or diagnostic images on CD or DVD were included. This study excluded patients with radiologic images on film, those with paper electrocardiography strips, and those with only a medical record or referral order without digital images. On arrival at our ED, the patient was registered at the reception desk and if a CD/DVD accompanied them, the digital images were transmitted to our PACS using transmission software. A few minutes later, the images from the referring hospital were available for review on our PACS. The time of upload and the number of digital images were recorded. The time interval from patient registration to the time of upload was calculated. The time intervals for X-ray images, computed tomography (CT) scans, and magnetic resonance imaging (MRI) were estimated separately, and the final upload time was defined as the longest time interval (the last uploaded images) among them.
- The digital images were categorized as follows: X-ray, CT, MRI, electrocardiography, angiography, endoscopy, and ultrasonography. Ultrasonography included obstetric or traumatic ultrasonography and cardiac echocardiography. According to the body parts imaged, facial and cranial X-ray images were classified as head X-rays (skull series, water’s view, orbital view, nasal view, etc.). Neck images, such as those of the cervical spine and lateral neck or air tracheograms, were classified as cervical spine X-rays. Chest X-rays included chest posteroanterior/anteroposterior images, rib series, and lateral sternum. Abdominal X-rays included the abdomen, erect/supine, or kidney/ureter/bladder. Classifications for CT scans included brain and facial CT, classified separately. Again, the major examined body parts were considered; thereby, CT pulmonary angiography was classified as chest CT and vascular CT for the detection of arteriosclerosis obliterans or deep vein thrombosis was classified as extremity CT.
- The categorical data were shown as numbers and percentages. The numerical data were represented as mean±standard deviation or median (interquartile range). Frequency was compared using the chi-square method. Mean values were compared using the Kruskal-Wallis test or Mann-Whitney U-test as appropriate. Statistical analysis was conducted using IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA) and P-values below 0.05 were considered statistically significant.
METHODS
- This study enrolled 321 patients who were treated during the study period. Their mean age was 58.9 years and 190 (59.2%) were male patients. Of these, there were 148 trauma patients (46.1%) and the trauma team was activated in 62 cases (19.3%). Eight patients were categorized as having ischemic stroke, seven as having hemorrhagic stroke, 105 as having a medical disease, and 13 as having a surgical disease. Of the 321 patients enrolled, 133 (41.4%) were admitted and 147 (45.8%) were discharged from the ED (Table 1).
- Outside images based on radiologic modality
- The most frequently conducted X-rays at the referring hospitals (225, 70.1%) were chest X-rays (Table 2). The median number of chest X-ray images was one. The median upload time was 14 minutes; the longest time was 83 minutes. Brain CT was the most common CT from the referring hospitals, followed by chest and abdominal CT. Brain CT was reviewed in 167 patients (52%) and the median number of CT images was 118. The median upload time was 12 minutes (maximum, 78 minutes). Nineteen patients came with brain MRI images. The median number of brain MRI images was 198. The median upload time was 16 minutes (maximum, 74 minutes). The median number of images was the largest in angiography (median, 1,041).
- The number of images and upload times according to disease category
- Among trauma patients, the trauma team was activated in 62 and not activated in 89. There were 170 nontraumatic patients. Chest, pelvis, and cervical X-rays and brain, face, chest, abdominal, and cervical CT scans were frequently done at the referring hospitals in the trauma team activation (TTA) group (Table S1).
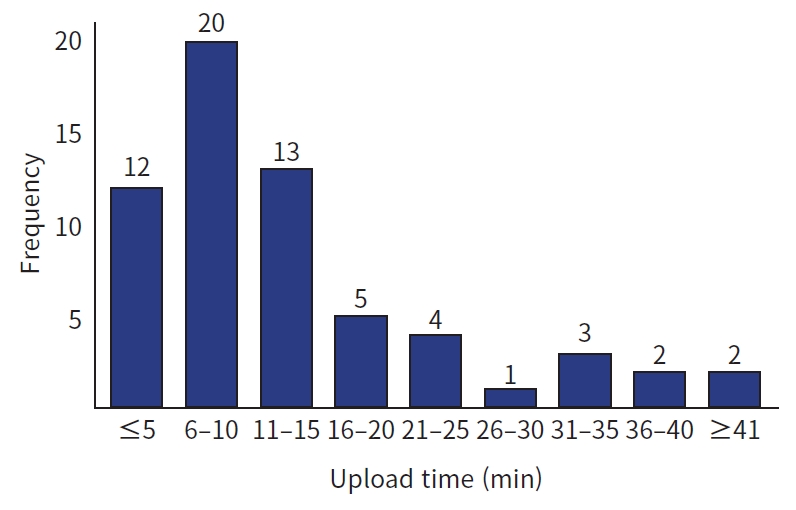
- In the subgroup analysis, the number of images was higher and the upload time was shorter in the TTA group than in the nontrauma or non-TTA trauma groups. No significant differences were observed between the nontrauma and non-TTA trauma groups. The median number of images was higher (688, 281, and 176, respectively; P<0.001), and the median upload time was shorter (10, 14, and 15 minutes, respectively; P=0.001) in the TTA group (Table 3). The longest upload time was 169 minutes. The upload time was longer than 20 minutes in 12 cases (19.4%) (Fig. 1).
- The number of images and upload times between the TTA groups and the stroke group
- The median number of images was higher in the TTA group than in the stroke group (688.0 vs. 159.5, P=0.009) (Table 4). The median upload time was longer, but the difference was not statistically significant (10.0 minutes vs. 7.5 minutes, P=0.123).
RESULTS
- AMI, acute stroke, and major trauma are time-sensitive diseases. These are also the three major categories of severe emergency diseases in Korea. Of the 389,269 patients with these diseases, 22,867 (5.8%) were transferred to other hospitals [8] including 1,865 of the 37,988 patients with AMI, 7,212 of the 120,584 with acute stroke, and 13,790 of the 230,697 with major trauma. Currently, 17 level I trauma centers exist in Korea and specialty hospitals for cardiovascular or cerebral care are increasing. Critically ill patients with time-sensitive diseases are transported by the physician-staffed HEMS. In multiple respects, efforts have been made to enhance the system of care. For time-sensitive diseases, it is important to ensure the optimal timing for the right treatment, rapid transportation, and quick decision making. Transferred patients are often accompanied by CD/DVDs of digitally recorded images done at the referring hospital. Confirming the care provided and any imaging done at the scene or the referring hospital is essential for proper decision making. Physicians at the receiving hospital can easily review the care provided in the medical record sent by the inter-hospital transfer communications system. However, the outside images must be viewed directly. Without the ability to review them, repetition of the same imaging studies is inevitable. Cost increase, radiation hazard, and preadministered intravenous contrast-induced image inadequacy could occur with repetition of imaging. Moreover, if the patient is unstable, a further diagnostic/radiologic study may not be possible. Therefore, physicians must review outside images, and time is required for this process. Therefore, the upload times need to be verified.
- In our study, the median number of outside images was 688 in the TTA group, which was greater than that of the non-TTA or nontrauma groups. However, the median upload time was shorter (10 minutes). In the TTA group, the upload time was shorter despite the much higher number of outside images. There is a reason for this discrepancy. When a transferred patient arrives at the ED, the accompanying CD/DVD could be reviewed directly on the ED computer before transmission to the PACS. This is not typically done by physicians treating patients with major trauma. The care of trauma patients often includes many specialists who each check the images separately. Therefore, quickly uploading the CD to the PACS is most efficient. However, for patients with other diseases, the outside CD could be reviewed on the ED computer before transmission to the PACS. This is why the upload time was shorter for the large number of images in the TTA group.
- Three more key points should be made. First, regarding the definition of upload time, the images are transmitted randomly, in no particular order (such as X-ray→CT→MRI or in order of the study date). Therefore, outside images can only be read after the transmission of all images is completed. The upload time was calculated based on the last image uploaded. Therefore, a result of 10 minutes is just a theoretical time interval of the image displaying system. More time is required in reality. Even if physicians wait for images to be uploaded without doing any other work, at least 10 minutes would be required. Moreover, it is difficult to tell whether all the images on the CD have been uploaded or are still in progress in the PACS. In general, the transmission completion is not obvious until there no more images are being uploaded. After that, the physicians must read the images in detail, which takes more time. The upload times shown in this study are literally the shortest possible time, and longer times are realistically required in most clinical situations. This 10- to 20-minute time difference may not have a significant impact on patients with certain diseases, but it can have an important negative impact on time-sensitive diseases.
- A second important point is that 169 minutes were taken for one patient, and image uploading took more than 20 minutes for 12 patients (Fig. 1). Taking more than 20 minutes to read the radiologic images of an unstable patient with major trauma means that outside images can be unhelpful. Because the radiologic diagnosis is essential for proper decision making, repetition of the radiologic study is inevitable if the outside images cannot be read within 20 minutes. If the patient’s condition does not allow obtaining additional images, the physician has to make a decision without radiologic evidence. Unexpectedly prolonged times were observed when the CD arrived late with a patient’s guardian, the CD was lost, or there was transmission error. Because such outliers exist, interpretations based only on average or median times can be skewed. In addition to delays, a focus on prolonged upload times is also necessary. The number of images may be high because past images were included, not just those done on that day. However, the receiving hospital is unable to address this; it is up to the referring hospital to separate and copy only images from the relevant day.
- A third important point is the interpretation of the relationship between the number of images and upload time, as shown in Table 2. No substantial difference was observed in the upload times based on image modality, such as X-rays with few images and CT or MRI with many images. This occurs because the images in the CD are uploaded randomly without a particular order (e.g., X-ray→CT→MRI). In addition, if the patient had a CT scan with a large number of images (e.g., 400 images), the numerous images are uploaded at the same time in our PACS, and when the CT images are uploaded, other images such as X-ray or MRI are uploaded as well. As a result, X-rays with fewer images were not necessarily uploaded quickly, and CT or MRI scans with many images were not necessarily uploaded late, but the overall upload time was longer because of the large number of images. In the same patient, the upload times appeared approximately the same regardless of the number of images, based on image modality.
- In AMI patients, any paper electrocardiogram strips can be located immediately upon patient arrival and a repeat electrocardiogram can be done quickly if necessary. However, in stroke and major trauma patients, outside images were read directly from the PACS. Trauma patients often have many images. In our study, the median number of images in the TTA patient group was 688, 4.3 times that of stroke patients (Table 4), and longer upload times were observed. Both trauma and stroke are time-sensitive diseases and the outside images of patients with both trauma and stroke are directly uploaded to our PACS. Therefore, this study compared these two conditions. This finding means that longer upload times are required for higher numbers of images. Prior research showed that reading of outside images in transferred trauma patients resulted in significant delays (up to 25 minutes) [9], and that repeated CT scans increased the workload and use of resources at receiving hospitals [10].
- For critical or time-sensitive diseases, efforts are required to reduce the time needed to make outside images ready for physician review and to avoid duplicate imaging. One possible option is a remote emergency consultation system for medically vulnerable areas. This is a system in which radiologic images or electrocardiograms performed at a referring hospital can be uploaded to a website and medical staff (primarily emergency physicians) at the predesignated receiving hospital can review the images and provide appropriate consultation. One study also found that this type of remote viewing by emergency consultation systems could reduce unnecessary transfers to a level I trauma center by 40% [11]. However, it assumed that the medical staff at the receiving hospital was available to review the uploaded images in advance during patient transfer, thereby minimizing the time taken after arrival.
- When transporting patients with AMI using HEMS, the door-to-balloon time was reduced by 16 minutes compared to when ground transportation was used [12]. Comparing ground transportation and HEMS, the number of patients who received care within the targeted window of time increased with the use of HEMS (11.4% and 40.5%, respectively). Considering this, simply being able to check outside images in advance could replicate the time-saving effects of helicopter transfers. Another advantage of this system is minimizing the risk of lost or late CD/DVDs or transmission errors.
- It may be possible to open an imported CD directly on the computer before uploading. However, if the patient has to be evaluated or treated by multidisciplinary specialists (e.g., major trauma), it is not efficient to check one CD in one ED computer, eventually leading to unnecessary duplicate images, loss of necessary images, and time delay. Therefore, patients with major trauma need a system making it possible to check outside images done at referring hospitals in advance before arrival.
- This study had several limitations. Since it was a retrospective study, it was difficult to investigate the exact reasons for the significant delays in all cases, and transmission error rates during the upload were not estimated. Because this was a single-center study, it was not confirmed whether the type of PACS software or computer specifications would affect the upload time. Furthermore, the prognosis of the patients affected by delayed upload times remains unknown.
- In conclusion, patients with major trauma bring more images than patients with other diseases. Unexpected delays (>20 minutes) were noted in approximately 20% of them. It is necessary to minimize this time by actively utilizing a system that allows medical staff to view the outside images in advance before patient arrival.
DISCUSSION
SUPPLEMENTARY MATERIALS
Table S1.
-
Ethical statements
Not applicable.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: HIK, YOK; Data curation: all authors; Formal analysis: HIK; Writing–original draft: SJW, HIK; Writing–review & editing: YOK.
All authors read and approved the final manuscript.
ARTICLE INFORMATION
| Characteristic | Value |
|---|---|
| Age (yr) | 58.9±21.2 (0–90) |
| Male sex | 190 (59.2) |
| Korean triage and acuity scale | |
| I | 31 (9.7) |
| II | 53 (16.5) |
| III | 143 (44.5) |
| IV | 84 (26.2) |
| V | 10 (3.1) |
| Systolic blood pressure (mmHg) | 136.4±30.0 |
| Diastolic blood pressure (mmHg) | 80.7±18.0 |
| Heart rate (/min) | 89.3±21.5 |
| Respiration rate (/min) | 17.5±5.9 |
| Body temperature (°C) | 36.5±0.8 |
| Disease categories | |
| Trauma | 148 (46.1)a) |
| Medical disease | 105 (32.7) |
| Ischemic stroke | 8 (2.5) |
| Hemorrhagic stroke | 7 (2.2) |
| Other neurologic disease | 15 (4.7) |
| Drug intoxication | 1 (0.3) |
| Postcardiac arrest status | 18 (5.6) |
| Psychiatric disease | 1 (0.3) |
| Surgical disease | 13 (4.0) |
| Peripheral vascular disease | 2 (0.6) |
| Foreign bodies | 3 (0.9) |
| Trauma team activation | 62 (19.3) |
| Treatment outcome | |
| Admission | 133 (41.4) |
| Discharge from emergency department | 147 (45.8) |
| Transfer | 20 (6.2) |
| Discharge against medical advice | 15 (4.7) |
| Expired | 6 (1.9) |
| Variable | TTA (n=62) | Non-TTA trauma (n=89) | Nontrauma (n=170) | P-value |
|---|---|---|---|---|
| No. of images | ||||
| Minimum | 1 | 2 | 1 | - |
| Maximum | 3,309 | 2,022 | 4,954 | - |
| Median (IQR) | 688 (292.0–1,117.8) | 281 (97.0–589.0) | 176 (49.5–676.0) | <0.001 |
| Ta) | ab) | b, c | c | - |
| Upload time (min) | ||||
| Minimum | 1 | 2 | 1 | - |
| Maximum | 169 | 65 | 138 | - |
| Median (IQR) | 10 (6.0–16.3) | 14 (9.0–18.0) | 15 (10.0–25.0) | 0.001 |
| Ta) | ab) | b, c | c | - |
| ≤20 | 50 (80.6) | 71 (79.8) | 109 (64.1) | 0.048 |
| 21–30 | 5 (8.1) | 8 (9) | 30 (17.6) | - |
| 31–40 | 5 (8.1) | 6 (6.7) | 13 (7.6) | - |
| >40 | 2 (3.2) | 4 (4.5) | 18 (10.6) | - |
- 1. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119–77. ArticlePubMed
- 2. Shavadia JS, French W, Hellkamp AS, et al. Comprehensive electrocardiogram-to-device time for primary percutaneous coronary intervention in ST-segment elevation myocardial infarction: a report from the American Heart Association mission: lifeline program. Am Heart J 2018;197:9–17. ArticlePubMed
- 3. Wong GC, Welsford M, Ainsworth C, et al. 2019 Canadian Cardiovascular Society/Canadian Association of Interventional Cardiology guidelines on the acute management of ST-elevation myocardial infarction: focused update on regionalization and reperfusion. Can J Cardiol 2019;35:107–32. ArticlePubMed
- 4. Warner JJ, Harrington RA, Sacco RL, Elkind MS. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. Stroke 2019;50:3331–2. ArticlePubMed
- 5. Furie KL, Jayaraman MV. 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke 2018;49:509–10. ArticlePubMed
- 6. American College of Surgeons. ATLS advanced trauma life support: student course manual. 10th ed. Chicago: American College of Surgeons; 2018.
- 7. Campbell J, Alson R, Han K. International trauma life support for emergency care providers. 9th ed. Illinois: Pearson; 2019.
- 8. National Emergency Medical Center. 2019 statistics of national emergency department information system. Seoul: Minsitry of Health and Welfare; 2020.
- 9. Emick DM, Carey TS, Charles AG, Shapiro ML. Repeat imaging in trauma transfers: a retrospective analysis of computed tomography scans repeated upon arrival to a level I trauma center. J Trauma Acute Care Surg 2012;72:1255–62. ArticlePubMed
- 10. Sung JC, Sodickson A, Ledbetter S. Outside CT imaging among emergency department transfer patients. J Am Coll Radiol 2009;6:626–32. ArticlePubMed
- 11. Moya M, Valdez J, Yonas H, Alverson DC. The impact of a telehealth web-based solution on neurosurgery triage and consultation. Telemed J E Health 2010;16:945–9. ArticlePubMed
- 12. Kim HI, Cho HY, Choi HJ. Analysis of the treatment-time reduction of ST elevation myocardial infarction patients transferred by helicopter-based emergency medical services in Korea. J Korean Soc Emerg Med 2020;31:586–94.
REFERENCES
Figure & Data
References
Citations

 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


