Portal vein embolization in intrahepatic portal vein injury after blunt trauma: a case report
Article information
Abstract
Mortality from hepatic injury has declined over the last several decades for various reasons, including nonoperative management, such as angioembolization, in more than 80% of cases. Conversely, surgical treatment is preferred in intrahepatic portal vein injury due to several reasons. Here, we report a case that treatment of blunt traumatic liver injury accompanied by intrahepatic portal vein injury through portal vein embolization. A 29-year-old female patient was transferred to our trauma center for vehicular accident injuries. Contrast-enhanced abdominal computed tomography showed a massive hemoperitoneum and liver laceration (grade IV) with contrast extravasation suspected of the right portal vein branch but no other organ injury. Since vital signs were stable, we decided to perform nonsurgical radiologic intervention. Portography showed active bleeding of the posterior branch of the right portal vein. A pseudoaneurysm in the portal vein was embolized through percutaneous transhepatic portal vein puncture. On follow-up liver dynamic computed tomography performed 2 days after embolization, the posterior branch of the right portal vein was sufficiently embolized, and no liver parenchymal necrosis was observed. The patient was discharged without any complications 2 weeks later. This report suggests portal vein embolization as a good alternative treatment method for portal vein injury in patients with stable vital signs.
INTRODUCTION
The liver is the most frequently injured abdominal organ following abdominal trauma. Fortunately, mortality from hepatic injury has declined over the past several decades for various reasons, including the evolution to the current approach of nonoperative management of hepatic trauma in more than 80% of cases [1]. Conversely, surgical treatment is preferred in intrahepatic portal vein injury due to several reasons. This report describes the nonsurgical treatment of a case involving blunt traumatic liver injury accompanied by intrahepatic portal vein injury through portal vein embolization (PVE) and establishes the characteristics of intrahepatic portal vein injury and indications for PVE. The patient provided informed consent for publication of the research details and clinical images.
CASE REPORT
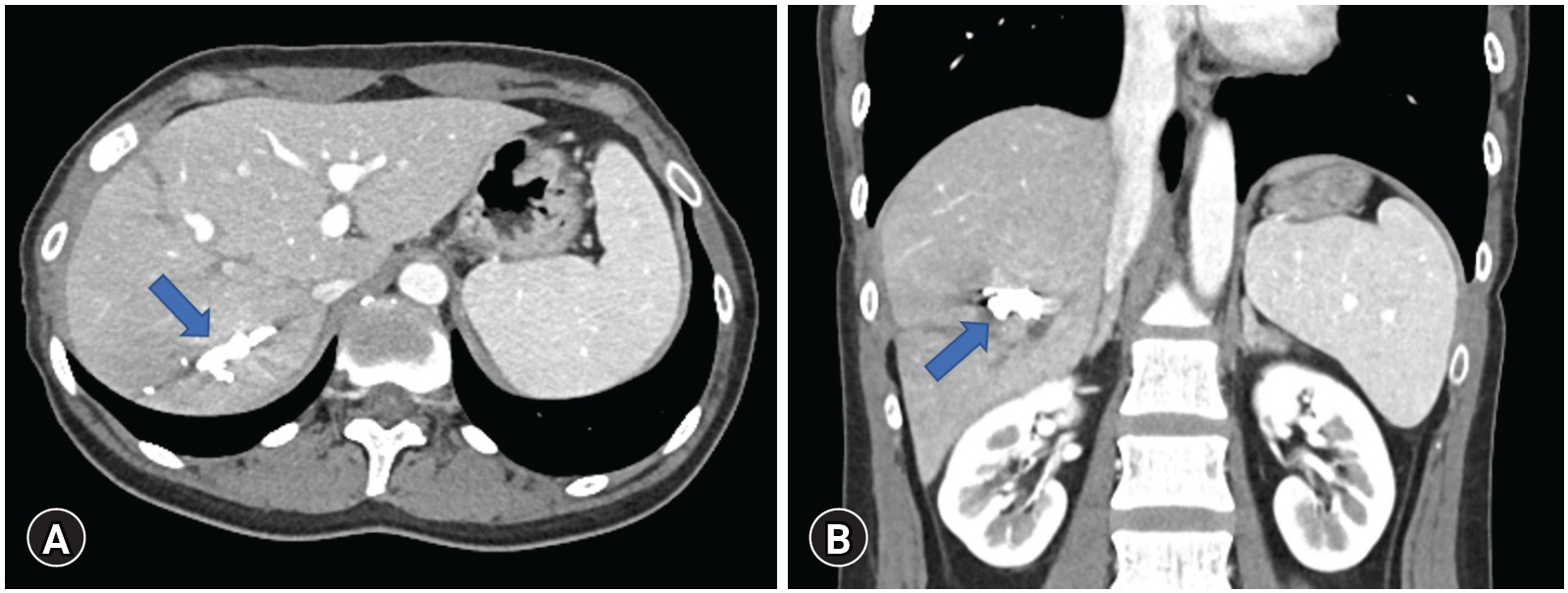
A 29-year-old female patient with no medical history was transferred to the Trauma Center of Kyungpook National University Hospital for injuries sustained after a passenger car accident. Her initial blood pressure was 115/81 mmHg and heart rate was 112 beats/min. Hemoglobin and platelet count was 14.3 g/dL and 190,000 /µL, respectively. Contrast-enhanced abdominal computed tomography showed a massive hemoperitoneum and liver laceration (grade IV) with contrast extravasation suspected of the right portal vein branch, but no other organ injury (Fig. 1).
Contrast-enhanced computed tomography of (A) axial and (B) coronal view, showing a massive hemoperitoneum and liver laceration (grade IV) with extravasation suspected of the right portal vein branch (arrows).
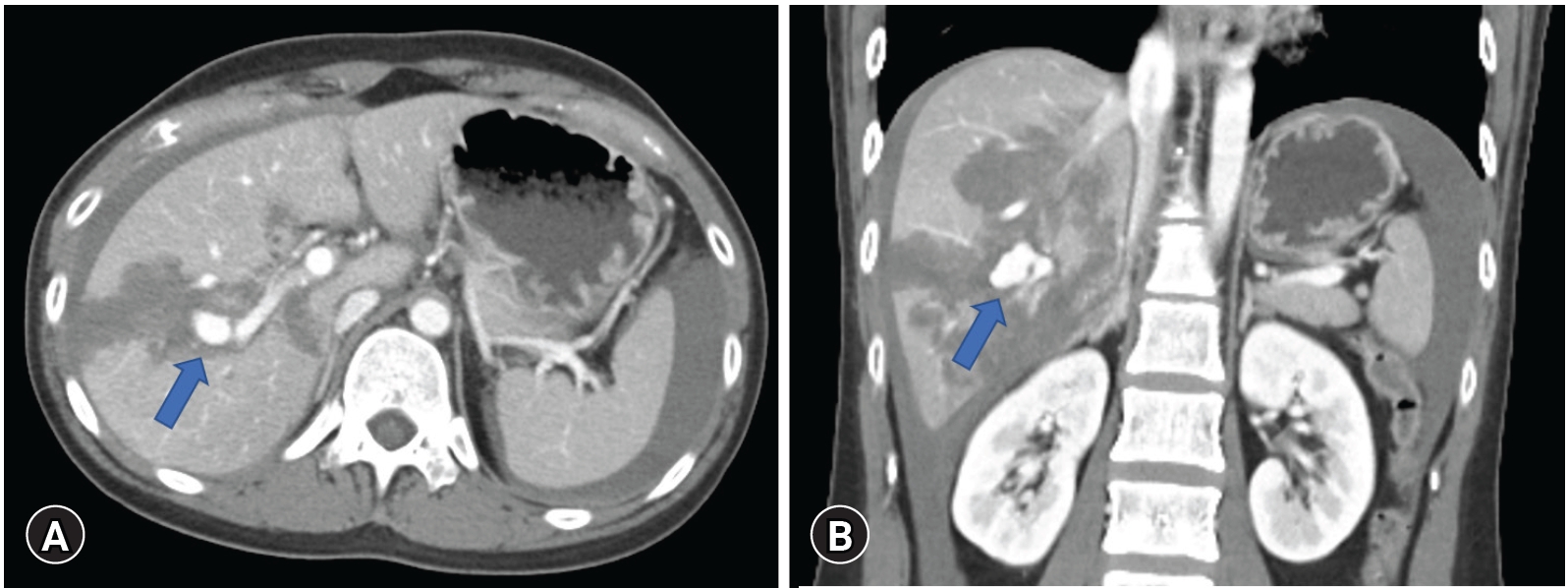
Since the patient’s vital signs were stable, we decided to perform nonsurgical radiologic intervention rather than surgery. The celiac artery angiography did not show active bleeding of the hepatic artery branch, but portography following superior mesenteric artery angiography showed a pseudoaneurysm in the posterior branch of the right portal vein (Fig. 2A). An angiography sheath was inserted through the P5 portal vein branch by percutaneous transhepatic approach to access the proximal portion rather than the injured portal vein branch, and portography showed a pseudoaneurysm at the proximal portion in posterior branch of right portal vein (Fig. 2B, C). The pseudoaneurysm was embolized using a mixture of glue (Histoacryl; B. Braun, Melsungen, Germany) and lipiodol (Lipiodol Ultra-Fluid; Guerbet, Villepinte, France). Portography performed after the procedure no longer showed active bleeding (Fig. 2D).

Portography showed (A) active bleeding of posterior branch of right portal vein (arrow) and (B) pseudoaneurysm at proximal portion in posterior branch of right portal vein (arrow). (C) Portography performed after selection of injured portal vein branch. (D) The pseudoaneurysm was embolized and no longer showed active bleeding sign in portography (arrow).
On follow-up liver dynamic computed tomography performed 1 month after embolization, intraabdominal hematoma was decreased, the posterior branch of the right portal vein was sufficiently embolized, and no bleeding sign or liver parenchymal necrosis was observed (Fig. 3). Additionally, the patient’s aspartate aminotransferase/alanine aminotransferase were 599/550 U/L in the initial laboratory test, with the highest measurements obtained the next day at 857/802 U/L. The levels gradually decreased to 35/125 U/L after a week.
DISCUSSION
The liver is the most commonly injured abdominal organ following blunt abdominal trauma. However, mortality from hepatic injury has declined over the last several decades. Richardson et al. [2] proposed that the reasons for the decreased mortality from hepatic trauma over the past 25 years are improved results with gauze packing and reoperation, use of arteriography and embolization, advanced operative techniques for major hepatic injuries, and decrease in the surgical treatment of hepatic venous injuries [1,2]. Additionally, the current approach to hepatic trauma has evolved to nonoperative management in more than 80% of cases [1]. Recently, a more extensive series of angiography for control of hepatic hemorrhage has been reported with increasing success, with the identification and control of bleeding rates ranging from 68% to 87%. Therefore, angiography and embolization or stenting are considered to be very useful adjunctive techniques in stable patients and are being managed nonoperatively [3].
Hepatic arterial injury from blunt hepatic trauma is a common cause of massive hemorrhage, but significant bleeding from the portal venous system is rare because the portal venous pressure is usually low. In addition, portal vein injuries are generally associated with severe injuries affecting adjacent organs that often require surgical treatment, such as gauze packing, vessel ligation, and venorrhaphy [4–6]. As such, angioembolization enables nonoperative management of arterial bleeding in blunt traumatic liver injury, but portal vein injury suitable to performing PVE is very rare. PVE is a preoperative treatment commonly performed to increase the volume of the remaining liver in patients undergoing major liver resection. It is a safe and effective method for inducing selective hepatic hypertrophy of the non-diseased portion of the liver and may thereby reduce morbidity and shorten hospital stays after resection [7].
In our patient, we decided to perform nonsurgical radiologic intervention because her vital signs were stable. If we decided to operate regardless, damage-control surgery, including gauze packing and reoperation, would have been performed and would have led to several postoperative complications, such as prolonged use of the mechanical ventilator, prolonged hospital stay, and even poor prognosis. Additionally, conservative treatment without intervention in this patient who with grade IV liver laceration accompanied by capsule injury, massive hemoperitoneum and active bleeding in the portal vein could worsen the condition even led to death.
According to our experience, several conditions are necessary in performing PVE in patients with intrahepatic portal vein injury. First, the most important condition is stable vital signs. Next, the patient must be cleared of any other organ injuries requiring surgery. Furthermore, unlike elective PVE, the intervention for trauma patients is urgent. An experienced radiologist must be present for accurate identification of trauma lesions and determination of the portal vein puncture site. Anatomic variants of the portal vein are uncommon but, when present, are important to recognize because they may have profound implications for PVE [7]. Finally, the surgical team should be prepared to perform emergency surgery immediately if the procedure fails.
In summary, our report demonstrates that PVE could be a good alternative treatment for portal vein injury in patients with stable vital signs.
Notes
Ethical statements
Informed consent for publication of the research details and clinical images was obtained from the patient.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: KHL; Project administration: SHC; Visualization: all authors; Writing–original draft: SHC; Writing–review & editing: all authors.
All authors read and approved the final manuscript.