Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(3); 2022 > Article
-
Original Article
Initial assessment of hemorrhagic shock by trauma computed tomography measurement of the inferior vena cava in blunt trauma patients -
Gun Ho Lee, MD
 , Jeong Woo Choi, MD
, Jeong Woo Choi, MD
-
Journal of Trauma and Injury 2022;35(3):181-188.
DOI: https://doi.org/10.20408/jti.2021.0066
Published online: June 10, 2022
- 1,957 Views
- 80 Download
Department of Emergency Medicine, Jeonbuk Regional Trauma Center, Wonkwang University Hospital, Iksan, Korea
- Correspondence to Jeong Woo Choi, MD Department of Emergency Medicine, Wonkwang University Hospital, 895 Muwang-ro, Iksan 54538, Korea Tel: +82-63-859-1175 E-mail: dream-02@daum.net
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Inferior vena cava (IVC) collapse is related to hypovolemia. Sonography has been used to measure the IVC diameter, but there is variation depending on the skill of the operator and it is difficult to obtain accurate measurements in patients who have a large amount of intestinal gas or are obese. As a modality to obtain accurate measurements, we measured the diameters of the IVC and aorta on trauma computed tomography scans and investigated the correlation between the IVC to aorta ratio and the shock index in blunt trauma patients.
-
Methods
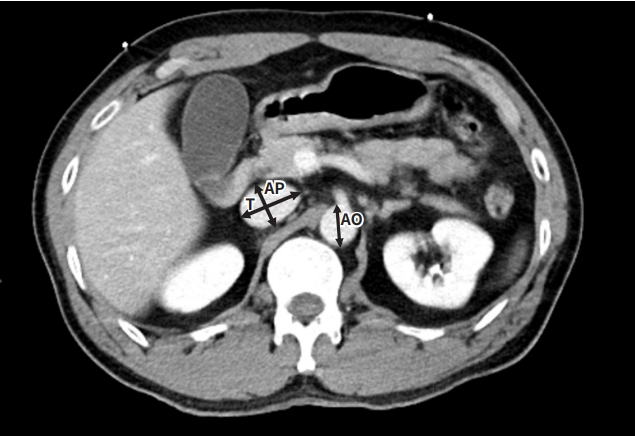
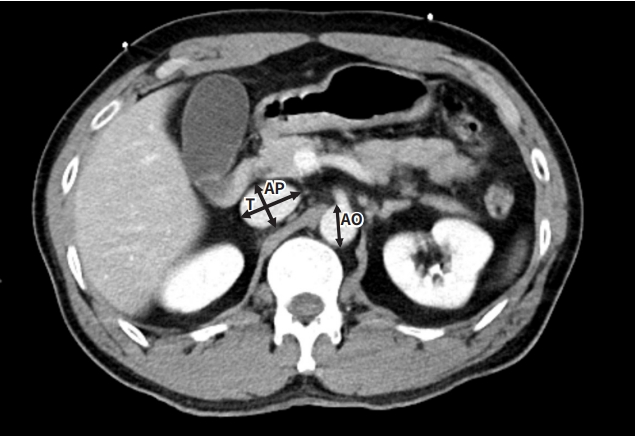
- We retrospectively analyzed the medical records of 588 trauma patients who were transferred to the regional trauma center (level 1) of Wonkang University Hospital from March 2020 to February 2021. We included trauma patients 18 years or older who met the trauma activation criteria and underwent trauma computed tomography scans with intravenous contrast within 40 minutes of admission. The shock index was calculated from vital signs before trauma computed tomography scan, and measurements of the anteroposterior diameter of the IVC (AP), the transverse diameter of the IVC (T), and aorta were made 10 mm above the right renal vein in the venous phase.
-
Results
- Overall, 271 patients were included in this study, of whom 150 had a shock index ≤0.7 and 121 had a shock index >0.7. The T to AP ratio and AP to aorta ratio were significantly different between groups. Cutoffs were identified for the T to AP ratio and AP to aorta ratio (2.37 and 0.62, respectively) that produced clinically useful sensitivity and specificity for predicting a shock index >0.7, demonstrating moderate accuracy (T to AP ratio: area under the curve, 0.71; sensitivity, 59%; specificity, 87% and AP to aorta ratio: area under the curve, 0.70; sensitivity, 55%; specificity, 91%).
-
Conclusions
- The T to AP ratio and AP to aorta ratio are useful for predicting hemorrhagic shock in trauma patients.
- Shock is a clinical condition that can arise from multiple etiologies; in blunt trauma patients, hemorrhagic shock is the leading etiology in most cases and can be rapidly fatal. Early detection of hemorrhagic shock and resuscitation are critical for the proper treatment of trauma patients. Hemodynamically unstable patients are rapidly transfused and intervened upon. However, in the absence of stage III or stage IV shock, the autoregulatory mechanisms of the body can readily compensate for volume depletion to maintain adequate blood pressure, pulse rate, and mental status. It is well-known that blood pressure is not decreased in states of shock until approximately 30% to 40% of the circulating blood volume has left the intravascular compartment [1]. In addition, the other signs of early shock (tachycardia, low blood pressure, pallor) may easily be overlooked or confounded by pain or anxiety, sympathetic surge, pharmaceutical and illicit drugs, and environmental factors in the trauma resuscitation room. Therefore, objective methods to diagnose early actual or impending shock following injury are needed.
- The inferior vena cava (IVC) collapses with shock because of absolute or relative hypovolemia [2]. Sonography has been used effectively as a primary screening procedure upon hospital entry in mass casualty patients with trauma, with an average of 4 minutes for each patient [3]. It has been used to measure IVC diameter, but variation exists depending on the skill of the operator and it is difficult to obtain accurate measurements if the patient has a large amount of intestinal gas or is obese. Another limitation is that multiple sites cannot be measured at the same time.
- Therefore, the authors measured the diameters of the IVC and descending aorta on computed tomography (CT) scans of blunt trauma patients, and indirectly assessed the volume of body fluid using the calculated ratio. The purpose of this study was to determine whether this method is useful for predicting hemorrhagic shock in blunt trauma patients.
INTRODUCTION
- We retrospectively analyzed the medical records of 588 trauma patients who were transferred to the regional trauma center (level 1) of Wonkang University Hospital. This facility is a tertiary healthcare center with 796 beds and a referral center supporting a region with a population of approximately 300,000. The need for informed consent was exempted due to the retrospective nature of the study.
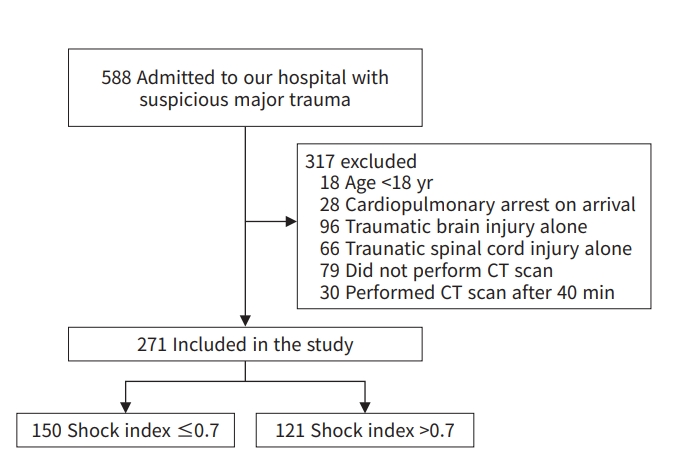
- The criteria included trauma patients 18 years or older who met the trauma activation criteria and underwent trauma CT scans with intravenous contrast within 40 minutes of admission. The exclusion criteria included patients under 18 years; those with cardiopulmonary arrest on arrival, traumatic brain injury alone, or a traumatic spinal cord injury alone; and those who did not receive a CT scan within 40 minutes (Fig. 1).
- Emergency transfusion (ET) was defined as transfusion within 1 hour. The total transfusion amount was defined as the transfusion amount during 24 hours.
- All trauma CT scans were performed with a 128-slice Stellar detector CT scanner (SOMATOM Definition Edge; Siemens, Washington, DC, USA). In our hybrid emergency room, it usually takes 5 to 10 minutes, including transfer and scanning with contrast medium, to perform CT scans in trauma patients. CT scans are typically performed within 40 minutes of arrival to the trauma center. Arterial and venous phase contrast-enhanced CT scans were reviewed. The anteroposterior diameter of the IVC (AP), the transverse diameter of the IVC (T), and aorta were measured 10 mm above the right renal vein in the venous phase (Fig. 2). AP corresponds to the smallest dimension of the IVC, and T represents the largest dimension of the IVC. One chief resident of emergency medicine, who was blinded to patients’ vital signs and laboratory data, retrospectively reviewed each CT scan for the size of the IVC and aorta.
- The following data were collected from patients’ medical records: age; sex; Injury Severity Score (ISS); vital signs, such as the mean arterial pressure (MAP), heart rate, respiratory rate, body temperature; calculated data, such as the shock index; measured data, such as the IVC diameter; laboratory data, such as hemoglobin, lactate, amount of ET, total amount of transfusion within 24 hours; and outcomes (length of intensive care unit admission and hospital stay).
- Demographic factors, laboratory results, physiological variables, and resource use were summarized using descriptive statistics (Table 1). IBM SPSS ver. 26.0 (IBM Corp., Armonk, NY, USA) was used for statistical analyses. In multiple comparisons involving multiple variables, post hoc analysis was performed using the independent sample t-test and one-way analysis of variance. For continuous variables, the analysis was performed using the independent sample t-test and logistic regression analysis. A P-value <0.05 was considered to indicate statistical significance.
METHODS
- In total, 588 patients suspected to have experienced major trauma who met the trauma activation criteria were admitted to our hospital during the study period. After applying the exclusion criteria, the 271 remaining patients were ultimately included in the analysis (Fig. 1). Of note, although the study protocol specified excluding patients with aortic aneurysms and aortic stenosis, there were no cases of prominent aortic aneurysms or aortic stenosis among the 588 patients.
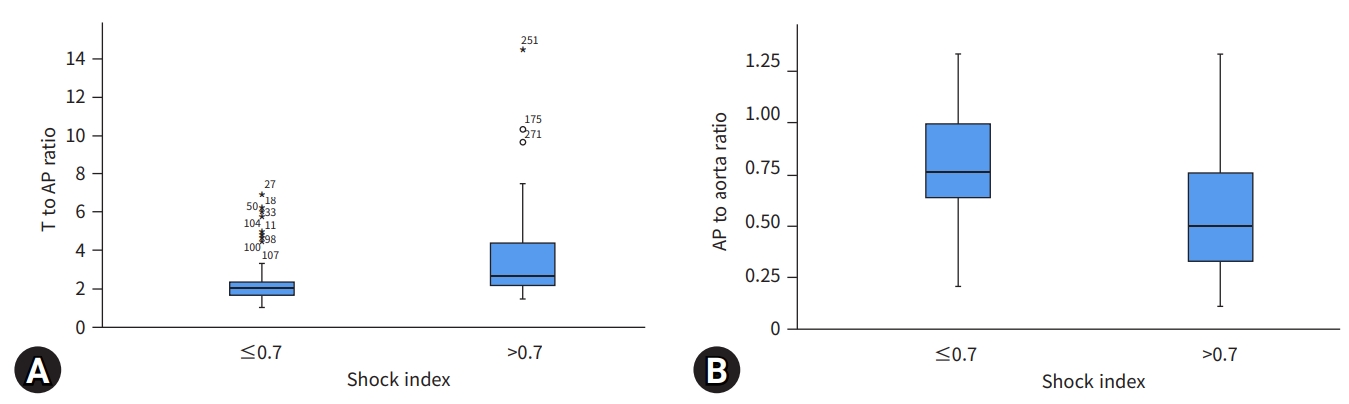
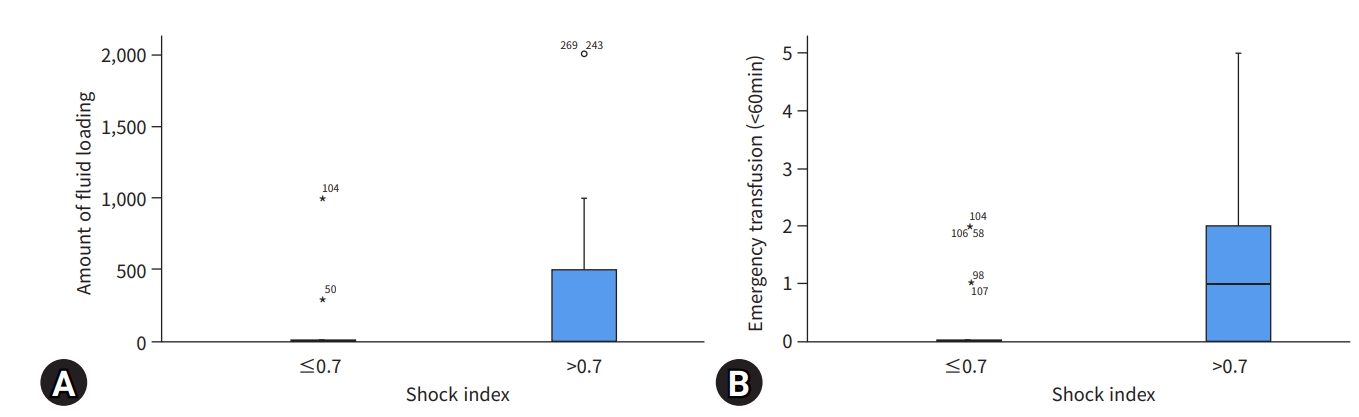
- Overall, 271 patients were included in this study, of whom 150 had a shock index ≤0.7 and 121 had a shock index >0.7. There were no significant differences between the two groups in age, sex, respiratory rate, body temperature, aorta diameter, hemoglobin, or time until the CT scan was performed. Significant differences between the two groups were observed in ISS, MAP, heart rate, shock index, T, AP, the T to AP ratio, the AP to aorta ratio, lactate, ET amount, total amount of transfusion within 24 hours, MAP, total fluid volume for resuscitation, length of intensive care unit admission days, and length of hospital stay (Table 1).
- The T to AP ratio and AP to aorta ratio were significantly different between the groups. We also examined the sensitivity and specificity of the cutoff of a shock index >0.7 in predicting IVC collapse via a cutoff point analysis. Cutoffs were identified for the T to AP ratio and AP to aorta ratio that produced clinically useful sensitivity and specificity for predicting a shock index >0.7 (Table 2).
- We performed a receiver operating characteristic curve analysis and calculated the area under the curve (AUC) to clarify which factor was the most useful predictor for shock (Fig. 3). Table 2 shows the respective AUCs, cutoff levels, sensitivities, and specificities for predicting shock. The cutoff of 2.37 for the T to AP ratio demonstrated moderate accuracy (AUC, 0.71; sensitivity, 59%; specificity, 87%), and a cutoff of 0.62 for the AP to aorta ratio likewise demonstrated moderate accuracy (AUC, 0.70; sensitivity, 55%; specificity, 91%).
- We compared multiple indices according to the cutoff levels of the T to AP ratio and AP to aorta ratio. Significant differences between the two groups defined using these cutoff points were observed in ISS, MAP, heart rate, shock index, ET amount (within 1 hour), total amount of transfusion within 24 hours, total fluid volume for resuscitation, length of intensive care unit stay, and length of hospital stay (Table 3).
RESULTS
- The detection of occult shock and impending shock in trauma patients who arrive with normal vital signs following injury remains difficult. In an earlier study, an T to AP ratio >2.5 on CT was defined as a flat IVC, which was found to be useful as a marker for measuring occult shock or hypoperfusion [4]. Another study of 114 patients found that an T to AP ratio of 4:1 was associated with shock [5].
- Given that the majority of trauma patients with stable or transient unstable vital signs undergo CT scans, we sought to determine whether the static T to AP ratio and AP to aorta ratio on trauma CT scans are associated with hemorrhagic shock, the need for emergency blood transfusion, total fluid volume for resuscitation, length of hospital stay, or other relevant factors.
- The IVC is a highly compliant vessel, the size and dynamics of which vary with changes in total body water and respiration. Although conflicting results have been published about respiration-related variations in the ultrasonographic appearance of the IVC, most authors have stated that the caliber of the normal IVC diminishes with inspiration and increases during expiration [6].
- The physical examination findings and vital signs of trauma patients are often unreliable for several reasons [7]. The unreliability of physical and laboratory evaluations combined with a lack of history and patient cooperation due to serious injury or an altered level of consciousness makes the clinical assessment of blood loss in these patients a difficult task. These uncertainties can potentially lead to inappropriate resuscitation–either too little or too much [8]. Measurement of the IVC diameter, therefore, can be a very useful way to evaluate the patient’s hemodynamic status [3]. In recent years, trauma centers have been rapidly performing early CT scans to assess organ damage. These scans are also useful to check along with other shock parameters since measurements of the IVC diameter are helpful for predicting shock even before confirmation of hemoglobin decrease, lactate increase, or metabolic acidosis.
- The presence of shock was assessed using the shock index. Because of the known lack of sensitivity of blood pressure as a predictor of shock, we opted to examine the correlation between the IVC ratio and the shock index. A shock index ≥0.7 is associated with a 20% likelihood of needing massive transfusion, and an increasing shock index has been shown to be directly proportional to worsening base deficit, ISS, and mortality risk [9–11].
- An advantage of sonography is that it can be performed repeatedly as a noninvasive modality, but CT scans can detect the IVC more easily than sonography because bowel air and abdominal fat impair acoustic penetration, resulting in poorer image quality. In addition, it is difficult to attach the sonographic probe to an open wound of the abdominal wall. As a result, the use of sonography is limited for patients who are obese and those who have a full stomach or an open abdominal wound [12].
- The T to AP ratio measured on CT scans was significantly elevated in patients with a shock index >0.7, and AP to aorta ratio was significantly lower in those shock index >0.7. In some exceptional cases, the IVC and aorta diameter did not correlate with the shock index due to fluid loading after insertion of a central line into the femoral vein or injury to a vein derived from the IVC (renal vein, lumbar vein, etc.) (Fig. 4). In a similar study, no correlation was found between IVC size and shock [11]. However, CT scans were not performed quickly in that study (in contrast to the mean interval of 13.2 minutes in our study) and CT scans were not performed in patients with unstable vital signs in this study.
- At the university hospital where the study was conducted, if necessary, within 60 minutes of the patient’s arrival, an ET of up to four units of red blood cells (type O) and four units of fresh frozen plasma, regardless of the patient’s blood type, is performed. Similar to a previous study on the correlation between IVC and massive transfusion, fluid loading was significantly greater and emergency transfusions were significantly more common in patients with a shock index >0.7, and the AP/aorta index was low in these patients [13] (Fig. 5).
- The T to AP ratio showed a relatively high correlation with lactate in patients with an T to AP ratio ≥2.37, but lactate levels were not checked in all trauma patients and this association did not show statistical significance (P=0.396) (Table 3).
- The shock index showed a relatively high correlation with the ISS in patients with a shock index >0.7, but the relevance of this finding is limited since the ISS score does not reflect only hemorrhagic shock (Fig. 6).
- Other studies have reported significant correlations between the IVC/aortic index and central venous pressure or body fluid volume as evaluated through CT or ultrasound is significant [14–16]. In comparison with the previous study, this study compared the correlations between the results (central venous pressure, IVC/aorta index) on rapid CT scans in patients with unstable vital signs. However, this was a retrospective study, and in the trauma bay, central venous pressure measurements were not performed before transferring patients to the operating room or ward, limiting the comparison of correlations. Another study found significant results for the correlation between prognosis and IVC measurements in patients with septic shock; therefore, we conducted a similar comparative analysis in trauma patients [17]. However, in cases of minor trauma or limb fractures, regardless of the patient's severity, the length of hospital stay increased due to complications such as infection or rehabilitation period. Therefore, it would be difficult to say that there was a significant correlation in all trauma patients.
- This study had several limitations. First, it was a retrospective cohort study conducted at a single center, which introduced potential selection bias. Moreover, uncontrolled confounding factors may have existed. Second, factors that affect the IVC size, such as positive end-expiratory pressure during CT, were not evaluated because of the nature of the retrospective study. Third, the study cohort mostly consisted of blunt trauma patients, and the results may not be applicable to patients with penetrating trauma. Finally, the cohort in this study was relatively small. For these reasons, as well as given the results of previous studies, further study will be required.
- In conclusion, the T to AP ratio and AP to aorta ratio were found to correlate with hemorrhagic shock in blunt trauma patients. Therefore, measurements of IVC size and aorta diameter on trauma CT scans for trauma patients to calculate the T to AP ratio and AP to aorta ratio are clinically relevant and can be used to predict shock or rapid transfusion.
DISCUSSION
-
Ethical statements
The need for informed consent was exempted due to the retrospective nature of the study.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: JWC; Data curation: GHL; Formal analysis: JWC; Methodology: JWC; Project administration: JWC; Writing– original draft: GHL, JWC; Writing–review & editing: GHL, JWC.
All authors read and approved the final manuscript.
ARTICLE INFORMATION


Values are presented as number (%) for categorical variables and mean (range) for continuous variables.
MAP, mean arterial pressure; T, transverse diameter of the inferior vena cava; AP, anteroposterior diameter of the inferior vena cava; PRC, packed red cells; CT, computed tomography; ICU, intensive care unit.
| Variable | AUC | Standard error | Optimal cutoff | P-value | Sensitivity | Specificity |
|---|---|---|---|---|---|---|
| T to AP ratio | 0.71 | 0.032 | 2.37 | <0.001 | 0.59 | 0.87 |
| AP to aorta ratio | 0.70 | 0.033 | 0.62 | <0.001 | 0.55 | 0.91 |
- 1. Henry S, Brasel K, Stewart RM. Advanced trauma life support. 10th ed. Chicago: American College of Surgeons; 2018.
- 2. Johnson JJ, Garwe T, Albrecht RM, et al. Initial inferior vena cava diameter on computed tomographic scan independently predicts mortality in severely injured trauma patients. J Trauma Acute Care Surg 2013;74:741–5. ArticlePubMed
- 3. Sefidbakht S, Assadsangabi R, Abbasi HR, Nabavizadeh A. Sonographic measurement of the inferior vena cava as a predictor of shock in trauma patients. Emerg Radiol 2007;14:181–5. ArticlePubMedPDF
- 4. Nguyen A, Plurad DS, Bricker S, et al. Flat or fat? Inferior vena cava ratio is a marker for occult shock in trauma patients. J Surg Res 2014;192:263–7. ArticlePubMed
- 5. Matsumoto S, Sekine K, Yamazaki M, et al. Predictive value of a flat inferior vena cava on initial computed tomography for hemodynamic deterioration in patients with blunt torso trauma. J Trauma 2010;69:1398–402. ArticlePubMed
- 6. Grant E, Rendano F, Sevinc E, Gammelgaard J, Holm HH, Gronvall S. Normal inferior vena cava: caliber changes observed by dynamic ultrasound. AJR Am J Roentgenol 1980;135:335–8. ArticlePubMed
- 7. Wo CC, Shoemaker WC, Appel PL, Bishop MH, Kram HB, Hardin E. Unreliability of blood pressure and heart rate to evaluate cardiac output in emergency resuscitation and critical illness. Crit Care Med 1993;21:218–23. ArticlePubMed
- 8. Porter JM, Ivatury RR. In search of the optimal end points of resuscitation in trauma patients: a review. J Trauma 1998;44:908–14. PubMed
- 9. Mutschler M, Nienaber U, Munzberg M, et al. The Shock Index revisited: a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit Care 2013;17:R172. ArticlePubMedPMC
- 10. Vandromme MJ, Griffin RL, Kerby JD, McGwin G Jr, Rue LW 3rd, Weinberg JA. Identifying risk for massive transfusion in the relatively normotensive patient: utility of the prehospital shock index. J Trauma 2011;70:384–8. ArticlePubMed
- 11. Radomski M, Agnihothri R, Knapp S, et al. Inferior vena cava size is not associated with shock following injury. J Trauma Acute Care Surg 2014;77:34–9. ArticlePubMed
- 12. Yanagawa Y, Nishi K, Sakamoto T, Okada Y. Early diagnosis of hypovolemic shock by sonographic measurement of inferior vena cava in trauma patients. J Trauma 2005;58:825–9. ArticlePubMed
- 13. Takada H, Hifumi T, Yoshioka H, et al. Initial inferior vena cava diameter predicts massive transfusion requirements in blunt trauma patients: a retrospective cohort study. Am J Emerg Med 2018;36:1155–9. ArticlePubMed
- 14. Yang JI, Han KH, Cho SU, et al. Correlation between sonographic inferior vena cava/aorta diameter index and central venous pressure. J Korean Soc Emerg Med 2010;21:341–6.
- 15. Oh SK, Cho YC, Koo DH, et al. Correlation between inferior vena cava/aorta diameter index and CVP: a retrospective study. J Korean Soc Emerg Med 2010;21:652–6.
- 16. Seo JH, Kim YW, Park DH, Cha JH, Choi JC, Yoon YS. Comparison of central venous pressure and the inferior vena cava/aorta diameter index for evaluation of body fluid status. J Korean Soc Emerg Med 2012;23:68–73.
- 17. Kim JH, Kim WY, Oh J, Kang H, Lim TH, Ko BS. Association of inferior vena cava diameter ratio measured on computed tomography scans with the outcome of patients with septic shock. Medicine (Baltimore) 2020;99:e22880. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite