Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(3); 2022 > Article
-
Original Article
Acute pain management in the trauma patient population: are we doing enough? A prospective observational study -
Segni Kejela, MD
 , Nebyou Seyoum, MD
, Nebyou Seyoum, MD
-
Journal of Trauma and Injury 2022;35(3):151-158.
DOI: https://doi.org/10.20408/jti.2021.0068
Published online: June 3, 2022
- 2,676 Views
- 146 Download
Department of Surgery, Tikur Anbessa Specialized Hospital, Addis Ababa University, College of Health Sciences, Addis Ababa, Ethiopia
- Correspondence to: Segni Kejela, FINAL DEGREE Department of Surgery, Tikur Anbessa Specialized Hospital, Addis Ababa University College of Health Sciences, Addis Ababa 5657, Ethiopia Tel: +251-911-569184 E-mail: segnikejo@gmail.com
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- There is a strong correlation between trauma and pain. Pain increases the rate of depression, posttraumatic stress disorder, and even mortality in trauma patients.
-
Methods
- This institution-based, provider-blinded and patient-blinded, observational study was conducted among trauma patients treated at kur Anbessa Specialized Hospital. Over the course of 3 months, this study included patients who had no prior pain management at other hospitals before presentation, and who presented within 24 hours of the traumatic event.
-
Results
- Of the 74 patients evaluated, none of the patients had their pain level scored. The researcher-provided pain scale showed a severe subjective pain score for 79.7% of the patients and a severe functional activity score for 59.5% of the patients. Analgesia was provided at an average of 55.4 minutes after presentation and all patients received either diclofenac or tramadol. Satisfactory pain reduction after analgesia was 28.8% for patients initially complaining of severe pain, 54.6% for moderate pain, and 66.7% for mild pain, with the difference being statistically significant (P<0.05). Forty percent of patients discharged home received no analgesia after the first dose provided upon presentation.
-
Conclusions
- Pain scoring was nonexistent during the course of the study. The poor utilization rate of analgesia combination and opioids led to unsatisfactory pain outcomes in patients evaluated and followed for 24 hours after presentation.
- Trauma is a global health burden, with a reported 973 million injuries needing some level of medical attention, 4.8 million trauma-related deaths, and 247.6 lost disability-adjusted life years in 2013 alone [1]. Trauma-related deaths account for 9% of the total death toll worldwide, predominantly affecting the younger, economically productive segment of the population [2–4]. The Ethiopian experience with trauma is similar to the global trend with regards to the age groups affected and its impact [5].
- Trauma and pain are strongly correlated, as evidenced by studies showing the prevalence of pain upon admission and discharge among trauma patients to be 91% and 86%, respectively [6]. The relationship between trauma and pain is far-reaching and possibly lifelong. A large-scale study done on over 3000 patients with major trauma reported that 1 year after trauma, 62.7% of the patients complained of pain at the site of injury with pain severity in the moderate range (5.5 points on a 10-point pain scale) [7].
- Pain in trauma patients potentiates the stress response, which increases tachycardia, oxygen consumption, hyper-coagulation, and immunosuppression. In addition, this response prolongs the recovery time [8]. Beyond the psychological relief when pain is decreased, management of pain in trauma patients has been shown to decrease morbidity and mortality [9]. Yet, adequate and organized pain management in trauma patients has not always been practiced in many trauma centers, especially in developing countries [10].
- Studies conducted in Ethiopia on trauma and pain are scarce in the literature. Therefore, this study aimed to determine the adequacy of pain management among acute trauma patients in the emergency department of a level III hospital in the capital of Ethiopia. We assessed the practice of evaluating patients for pain, organizing pain care, and the follow-up of patients in pain, including possible changes made in the management of pain based on re-evaluation by the treating team.
INTRODUCTION
- Ethical statements
- Before data collection, approval was obtained from the Research Ethics Committee of the Department of Surgery, Faculty of Medicine, Addis Ababa University. All participants over the age of 18 years, were asked for their consent, and all measures of confidentiality were ensured. Those participants between the ages of 13 and 18 years were asked for assent, and consent was acquired from the parents or legal guardians on site.
- Study design and setting
- Tikur Anbessa Specialized Hospital is the largest public hospital in Ethiopia. It serves approximately 500,000 patients a year, with 24-hour, 7-day-a-week emergency services provided alongside elective and emergency multidisciplinary surgical services at a level III designation.
- This was a facility-based observational study with data gathered from the patients and their charts over 3 months. The survey design was aimed at providing descriptive data of acute pain care among trauma patients in Tikur Anbessa Specialized Hospital. Each observation commenced at the time of presentation to the emergency department (ED), and the follow-up period was 24 hours for every patient or until discharge. This was a blinded study, in which both the patient and the treating team were unaware of the study, to avoid observational bias.
- Study population and variables
- All trauma patients who were admitted, observed, discharged, or referred were evaluated using a survey format only if they presented within 24 hours of the trauma and had received no analgesia at the referring facility. The independent variables were age, sex, occupation, region, time of arrival (day/night), duration between trauma and presentation, anatomic site of trauma, mechanism of injury, outcome of trauma, and training level of the evaluating physician. The dependent variables were pain scoring documentation, type and dose of analgesic given, delay of analgesia from presentation (in hours), pain rescoring after analgesia, the interval between doses of analgesia, and changes in analgesics.
- Sample size determination
- The population proportion could not be determined. Therefore, an initial pilot study of 20 patients analyzed the rate of pain scoring done by treating physicians. In the pilot study, pain scoring was done for one patient (5%) of the 20 patients who were initially evaluated, so a population proportion of 5% was used for sample size calculation.
- Data collection and data quality control
- Data were collected using a structured researcher-provided questionnaire. The data were collected over 1 month by a single trained data collector, with 1 month allotted for preliminary data collection to ensure that the data collector was accustomed to the data collection process. All incomplete data were discarded.
- Data processing and analysis
- The collected data were analyzed using IBM SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA). A descriptive analysis was conducted to describe the sociodemographic characteristics of the study population. Univariable logistic regression was utilized to evaluate the associations between pain and analgesia based on different scoring models.
METHODS
- In this study, 74 consecutive patients, fulfilling all the strict inclusion criteria, were analyzed. Among these 74 patients, 57 patients (77%) were male and 55 patients (74.3%) were under the age of 45 years. More than half (n=41, 55.4%) of the trauma victims were married, and close to half (n=36, 48.6%) were from Addis Ababa. Only 13 patients (17.8%) had a college education, and the same number of participants were uneducated (defined as not having attended primary school). Most patients were categorized as private employees (n=19, 26%) and students (n=13, 17.8%). The time of presentation after trauma ranged from 1 to 24 hours, with a mean of 9.19±7.62 hours. Fifty patients (67.9%) presented during the daytime (Table 1).
- Among other characteristics, 66 patients (89.2%) were primarily evaluated by interns and 72 patients (97.3%) were evaluated by residents, either primarily or following an intern’s evaluation. Orthopedic residents were involved in patient evaluation in 48 cases (64.9%), general surgery residents in 13 cases (17.6%), emergency medicine residents in eight cases (10.8%), and neurosurgery residents in three cases (4.1%). Regarding residents' years of training, 27 patients (36.5%) were evaluated by first-year residents, 23 (31.1%) by second-year residents, 20 (27.8%) by third-year residents, and two (2.8%) by fourth-year residents.
- As for the trauma mechanisms and circumstances, blunt trauma (n=66, 89.2%) was the most common mechanism. From the blunt trauma group, 27 (40.9%) were injured by pedestrian versus motor vehicle accidents. On the primary survey, there was no patient with airway compromise, but four patients (5.5%) had either labored or gasping-type breathing. Two patients presented with hypotension and six patients with a Glasgow Coma Scale of 13 or 12. Twenty-nine patients (39.2%) presented with tachycardia (heart rate >100 beats/min). The most common sites of injury were the extremities, with a fracture or dislocation reported in 59 patients (79.7%). This was followed by pelvic injury in 23 patients (31.1%), and traumatic brain injury in 16 patients (21.6%). Six patients (8.1%) had alcohol intoxication at presentation. Most patients (n=51, 68.9%) were kept at the ED for observation and investigation beyond the first 24 hours, while 15 (20.3%) were discharged home after evaluation within 24 hours of presentation (Table 2).
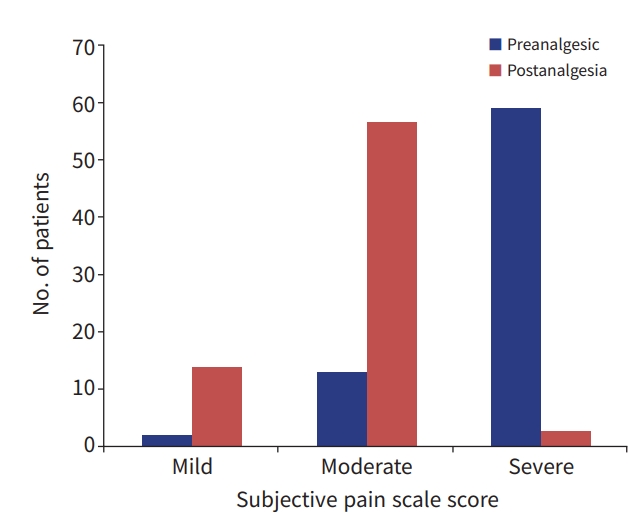
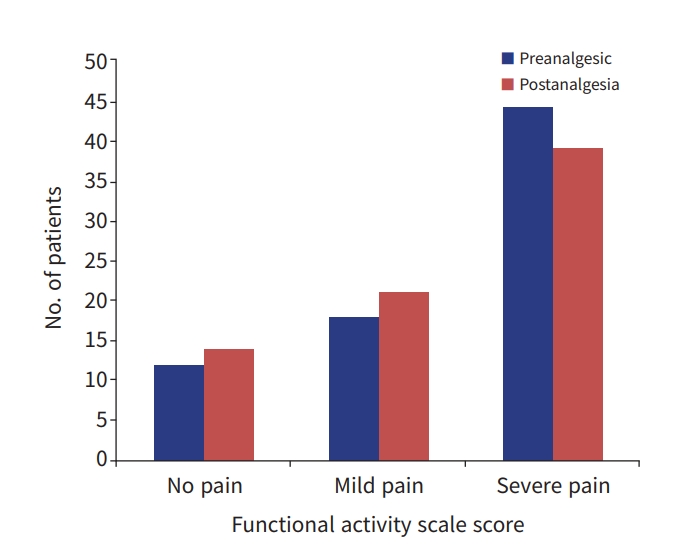
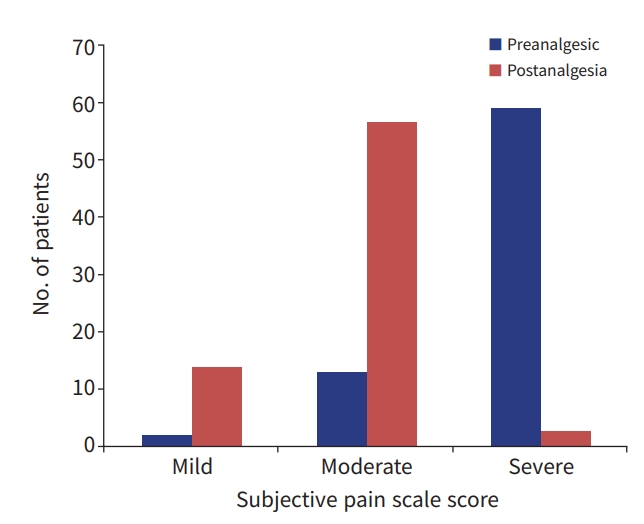
- No patient had any pain score recorded in their charts upon the initial evaluation or during the follow-up evaluations. Researcher-provided preanalgesia scores, based on a subjective pain scale (SPS) and a functional activity scale (FAS), were calculated for all patients. Based on the SPS, 59 patients (79.7%) were in severe pain, 13 (17.6%) were in moderate pain, and two (2.7%) were in mild pain. The FAS showed severe pain in 44 patients (59.5%), while moderate/mild pain and no pain were recorded in 18 (24.3%) and 12 patients (16.2%), respectively (Figs. 1, 2).
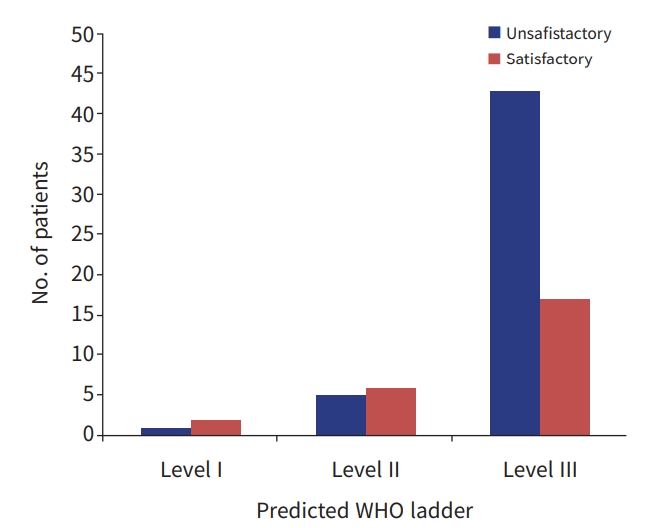
- The need for analgesia and the type of analgesia needed were determined by the researchers based on the researcher-provided pain scores and stratified, based on the World Health Organization (WHO) trauma pain management ladder, as levels I, II, or III. For prediction purposes, both functional activity scores and subjective pain scores were utilized and the more severe score of the two was used for designation on the WHO ladder. Based on this, 60 patients (81.1%) were initially categorized as level III on the WHO ladder, 11 (14.9%) as level II, and three (4.1%) as level I.
- All patients were provided with analgesia by the treating team and all analgesics given were in levels I and II of the WHO ladder. The utilized drugs were tramadol (50 mg intravenous/intermuscular) in 65 patients (87.8%) and diclofenac (75 mg intramuscular) in nine patients (12.2%). No patient received a combination of analgesics. All patients provided with diclofenac (WHO ladder level I medication) had severe pain. The time from presentation to analgesia ranged from 20 minutes to 240 minutes, with a mean of 55.4±35.3 minutes. At 60 minutes after presentation, three patients (100%) were predicted to be on level I of the WHO ladder, 10 patients (90.9%) on level II of the WHO ladder, and 54 patients (90%) on level III of the WHO ladder had received the first dose of analgesia. There was no correlation between the predicted level of the WHO ladder (as a measure of severity of pain) and time to first dose of analgesia in the logistic regression analysis (P=0.639).
- We attempted to retrieve response to analgesia data from patient chart documentation and no patient pain-level scoring after analgesia was provided. The researcher-provided pain scoring data were done at a mean time of 114.3±59.7 minutes after the first dose of analgesia. Using SPS parameters, three (4.1%), 57 (77%), and 14 patients (18.9%) had severe, moderate, and mild pain, respectively. Utilizing the FAS, 39 (52.7%), 21 (28.4%), and 14 patients (18.9%) had severe, mild/moderate, and no pain, respectively. Based on satisfaction stratification (with “unsatisfactory” including residual moderate or severe pain on the SPS and severe residual pain on the FAS), 50 patients (67.6%) had an unsatisfactory pain response based on the FAS and 49 patients (66.2%) had an unsatisfactory score based on the SPS (Figs. 1, 2).
- An analysis of the relationship between the predicted preanalgesia WHO ladder and satisfaction based on the postanalgesia SPS satisfaction rate showed an unsatisfactory pain response in 43 out of 60 patients (71.2%) stratified at level III on the WHO ladder and five of 11 patients (45.4%) at level II of the WHO ladder. In an analysis of the correlation between the predicted preanalgesia WHO ladder and postanalgesia FAS-based satisfaction, 44 of 60 patients (73.3%) stratified at level III of the WHO ladder had an unsatisfactory pain response and five of 11 patients (45.4%) stratified at level II of the WHO ladder had an unsatisfactory pain outcome. This difference was statistically significant in univariable logistic regression analysis, with P-values of 0.05 and 0.04, respectively (Table 3, Fig. 3).
- Of the patients treated by junior residents (first-year and second-year residents), 34 of 50 patients (68%) had unsatisfactory scores. Similarly, 15 of the 20 patients (68.2%) treated by senior residents had unsatisfactory responses. The year of residency was not associated with level of satisfactory response to pain treatment (P=0.98). The field of study of the treating residents was also not associated with the level of satisfaction with care for pain (P=0.34).
- During their stay in the ED, 14 patients (18.9%) had a change of analgesics. Five patients (6.75%), initially on diclofenac with an unsatisfactory pain response were upregulated to tramadol, while one patient with a satisfactory pain response with diclofenac was also upregulated to tramadol. Four patients (two diclofenac and two tramadol) with unsatisfactory pain responses after the initial dose were given no further analgesia while three patients initially on tramadol with a satisfactory pain response were also given no further analgesia, resulting in a total drug discontinuation rate of 9.4%. One additional patient, initially on tramadol with an unsatisfactory pain response, was downregulated to diclofenac. All patients who were kept in the ED, admitted to the wards, referred, or who underwent emergency procedures were continued on tramadol. Six of 15 patients (40%) were sent home without analgesics.
RESULTS
- The sociodemographic variables gathered from this study were not unique and reflected the general demographics of the country [11–15]. The majority of patients were evaluated by interns. This may not be a major factor in trauma patient pain management, as most patients were also evaluated by residents. One striking finding was the poor involvement of emergency medicine residents in the evaluation of the patients, which might have affected pain management. Regardless, a recent publication, addressing the knowledge and perception of pain management by residents, showed poor medical school curricular structures for teaching proper pain management. We have also found this to be true in Ethiopia, where no dedicated module or rotation in pain care is available during medical training [16].
- The prevalence of blunt trauma over penetrating trauma, as well as the prevalence of motor vehicle-related injuries, has been reported both nationally and internationally [17–19]. A notable finding was the higher prevalence of pedestrian-vehicle traffic accidents over motor vehicle collisions, as reported in studies of Ethiopian national data [20]. The extremities and pelvis were the most common anatomic sites of injury, followed by the head. Orthopedic injury and head trauma predominated in both civilian and combat casualty patients [21,22].
- The average time of patient presentation posttrauma was slightly more than 9 hours. For the patients in this study, no analgesia was given at the scene or during transport from the referring hospital. Such a delay in pain care is shown to have lasting implications for long-term physical and psychological health and is linked to an increased risk of chronic pain, depression, and posttraumatic stress disorder [23–25].
- Preanalgesia pain scoring by the treating team was not performed for any of the trauma patients evaluated in this study. This is staggeringly low when compared to studies from developed countries which have reported a pain scoring rate as high as 73% [26]. Using the researcher-collected data, the preanalgesia pain score for severe pain was close to 60% and 80% with the SPS and FAS scoring systems, respectively. This correlates well with other studies [27,28]. Every patient was provided with analgesia, with a mean door-to-needle time of 55 minutes. This value is not disappointing when compared to studies from other low-income countries [10]. The predicted WHO ladder was based on both the SPS and the FAS scores, with the more severe score used to predict the type of analgesia needed. The WHO ladder level predicted for more than 80% of the patients was level III (strong opioid) [9]. All analgesics provided were from the WHO ladder level I (diclofenac) and level II (tramadol). These were provided regardless of the level of pain reported by the patients. This was evidenced by the fact that all patients provided with diclofenac were in the severe pain group and were predicted to receive WHO ladder III analgesics. Failure of the treating team to score the pain level of the patients led to more than three-quarters of the patients having an unsatisfactory outcome. This is in comparison to almost half of the patients in the predicted WHO ladder level II and only a third of patients in the WHO ladder level I groups with unsatisfactory outcomes. This difference was statistically significant. This highlights the need for pain scoring before analgesia and for adherence to the regimens of the assigned WHO ladder category to achieve proper analgesia for every individual patient.
- In this study, no relationship was found between the level of residency training and the primary outcome of satisfactory pain control in acute trauma patients. This indicates that the topic of comprehensive management of acute pain in trauma patients had not been addressed at any level during the residents’ training. The field of study of the residents involved in the care of the trauma patients did not have an impact on the care provided for acute pain, indicating that the lack of proper acute pain management transcends departmental boundaries.
- An analysis of ongoing pain management beyond the first dose of analgesia showed that 14 of 74 patients had a change in pain regimen within 24 hours; four patients (5.4%) requiring upregulation were withdrawn from the medications instead, while three patients requiring maintenance with the initial satisfactory response were also withdrawn. This outcome is evidence that pain management was not based on patient response to analgesia, but rather depended on the discretion of the physician. A more worrying outcome is the fact that 40% of patients discharged home were sent home without analgesia. As one study from the Netherlands showed, two-thirds of patients discharged from the ED with musculoskeletal pain had moderate to severe pain at the time of discharge. This study showed the need to maintain analgesia for patients being discharged after acute trauma.
- The concept of acute pain management is certainly not new, but the practice seems quite variable across centers and countries. The institution of interest, in one of the low-income countries, showed nonexistent pain scoring practice, disorganized analgesia provision, and poor pain care for discharged patients. In addition, in groups managed with some sort of analgesia, no combination of analgesics was provided and no strong opioid was prescribed. As a result, more than two-thirds of patients with severe pain were not treated to the level at which the pain was satisfactorily manageable for the patients. Based on these findings, we recommend curricular inclusion of pain management for all trainees and implementation of a guideline-based pain management culture. Provision of proper analgesia, including strong opioids, along with monitoring of their appropriate utilization is needed. We also recommend ensuring the availability of pain management experts in large metropolitan hospitals.
DISCUSSION
-
Ethical statements
This study was approved by the Research Ethics Committee of the Department of Surgery, Faculty of Medicine, Addis Ababa University. Informed consent was obtained from all participants or the participants’ parents or legal guardian.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: SK; Data curation: NS; Formal analysis: SK; Methodology: SK; Project administration: NS; Visualization: SK; Writing–original draft: SK; Writing–review & editing: NS.
All authors read and approved the final manuscript.
ARTICLE INFORMATION
- 1. Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev 2016;22:3–18. PubMed
- 2. World Health Organization (WHO). Injuries and violence: the facts 2014. Geneva: WHO; 2014.
- 3. Bolandparvaz S, Yadollahi M, Abbasi HR, Anvar M. Injury patterns among various age and gender groups of trauma patients in southern Iran: a cross-sectional study. Medicine (Baltimore) 2017;96:e7812. PubMedPMC
- 4. Fazel MR, Fakharian E, Mahdian M, Mohammadzadeh M, Salehfard L, Ramezani M. Demographic profiles of adult trauma during a 5 year period (2007-2011) in Kashan, IR Iran. Arch Trauma Res 2012;1:63–6. ArticlePubMedPMC
- 5. Gemechu T, Tinsae M, Ashenafi S, et al. Most common causes of natural and injury-related deaths in Addis Ababa, Ethiopia. Pathol Res Pract 2009;205:608–14. ArticlePubMedPMC
- 6. Berben SA, Meijs TH, van Dongen RT, et al. Pain prevalence and pain relief in trauma patients in the accident & emergency department. Injury 2008;39:578–85. ArticlePubMed
- 7. Rivara FP, Mackenzie EJ, Jurkovich GJ, Nathens AB, Wang J, Scharfstein DO. Prevalence of pain in patients 1 year after major trauma. Arch Surg 2008;143:282–8. ArticlePubMed
- 8. Hedderich R, Ness TJ. Analgesia for trauma and burns. Crit Care Clin 1999;15:167–84. ArticlePubMed
- 9. Ahmadi A, Bazargan-Hejazi S, Heidari Zadie Z, et al. Pain management in trauma: a review study. J Inj Violence Res 2016;8:89–98. PubMedPMC
- 10. Kabore RA, Ki KB, Traore AI, et al. Assessment of the care of acute pain at the Trauma Center of Ouagadougou. Int J Clin Anesthesiol 2013;1:1016.
- 11. Ayele TA, Zeleke BM, Tessema GA, Melak MF. Magnitude and patterns of injuries among patients in Gondar University Hospital, northwest Ethiopia: an institutional-based study. Open Access Surg 2017;10:25–31.
- 12. Gebremichael M, Guta M, Gedefaw M, et al. Prevalence and determinants of road traffic injuries in Ethiopia: based on the 2015 STEPS survey findings. Ethiop J Health Dev 2017;31(Special Issue):340–7.
- 13. Byun CS, Park IH, Oh JH, Bae KS, Lee KH, Lee E. Epidemiology of trauma patients and analysis of 268 mortality cases: trends of a single center in Korea. Yonsei Med J 2015;56:220–6. ArticlePubMedPMC
- 14. Moodley NB, Aldous C, Clarke DL. An audit of trauma-related mortality in a provincial capital in South Africa. S Afr J Surg 2014;52:101–4. ArticlePubMed
- 15. Ethiopian Public Health Institute (EPHI); ICF. Ethiopia mini demographic and health survey 2019: key indicators. Rockville: ICF; 2019.
- 16. Garcia J, Ohanisian L, Sidley A, et al. Resident knowledge and perception of pain management. Cureus 2019;11:e6107. ArticlePubMedPMC
- 17. Li Q, Alonge O, Lawhorn C, et al. Child injuries in Ethiopia: a review of the current situation with projections. PLoS One 2018;13:e0194692. ArticlePubMedPMC
- 18. DiMaggio C, Ayoung-Chee P, Shinseki M, et al. Traumatic injury in the United States: in-patient epidemiology 2000-2011. Injury 2016;47:1393–403. ArticlePubMedPMC
- 19. Negussie A, Getie A, Manaye E, Tekle T. Prevalence and outcome of injury in patients visiting the emergency Department of Yirgalem General Hospital, Southern Ethiopia. BMC Emerg Med 2018;18:14. ArticlePubMedPMCPDF
- 20. Abegaz T, Gebremedhin S. Magnitude of road traffic accident related injuries and fatalities in Ethiopia. PLoS One 2019;14:e0202240. ArticlePubMedPMC
- 21. Janak JC, Mazuchowski EL, Kotwal RS, et al. Patterns of anatomic injury in critically injured combat casualties: a network analysis. Sci Rep 2019;9:13767. ArticlePubMedPMCPDF
- 22. Pan RH, Chang NT, Chu D, et al. Epidemiology of orthopedic fractures and other injuries among inpatients admitted due to traffic accidents: a 10-year nationwide survey in Taiwan. ScientificWorldJournal 2014;2014:637872. ArticlePubMedPMCPDF
- 23. Katz J, Jackson M, Kavanagh BP, Sandler AN. Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. Clin J Pain 1996;12:50–5. ArticlePubMed
- 24. Norman SB, Stein MB, Dimsdale JE, Hoyt DB. Pain in the aftermath of trauma is a risk factor for post-traumatic stress disorder. Psychol Med 2008;38:533–42. ArticlePubMed
- 25. Saxe G, Stoddard F, Courtney D, et al. Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adolesc Psychiatry 2001;40:915–21. ArticlePubMed
- 26. Silka PA, Roth MM, Moreno G, Merrill L, Geiderman JM. Pain scores improve analgesic administration patterns for trauma patients in the emergency department. Acad Emerg Med 2004;11:264–70. ArticlePubMed
- 27. Rahman NH, Ananthanosamy C. The display effects of patients’ self-assessment on traumatic acute pain on the proportion and timing of analgesics administration in the emergency department. Int J Emerg Med 2014;7:36. ArticlePubMedPMCPDF
- 28. Albrecht E, Taffe P, Yersin B, Schoettker P, Decosterd I, Hugli O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in prehospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth 2013;110:96–106. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite