Humeral intramedullary nail bending following trauma: a case report
Article information
Abstract
The surgical approach for humeral implant failure can be challenging due to neurovascular anatomy and the possible necessity of osteosynthesis removal. We present a rare case of humeral nail bending after secondary trauma in a patient with preexistent nonunion of the humerus after intramedullary nailing. During revision surgery, the nail was sawed in half and the distal part was removed, followed by plate osteosynthesis with cable fixation to achieve absolute stability. The patient regained a full range of motion 1 year after surgery, and complete healing of the fracture was seen on imaging.
INTRODUCTION
Humeral fractures can occur proximally, midshaft, or distally and are categorized as having simple, wedge, or complex (comminuted) patterns. Midshaft humeral fractures account for 2% of all fractures [1]. Since humeral shaft fractures have an excellent consolidation ability due to the rich vascularization by soft tissue and surrounding muscles, the majority of these fractures can be treated conservatively [2]. With nonoperative management, union rates of more than 90% have been described in the literature [2]. Because of the large range of motion of the shoulder and elbow joint, rotatory and angulatory deformities can be compensated for. The most common complications associated with shaft fractures include neurovascular compromise (radial nerve) and nonunion.
Nonunion after a humeral fracture presents a challenge for the surgeon and is often debilitating for the patient. Humeral nonunion is defined as the absence of bone healing 6 to 12 months after initial injury [3], and it can be subdivided as atrophic and hypertrophic [4]. After operative treatment of humeral shaft fractures, an incidence of nonunion between 2.5% and 13% has been reported [2]. Compared to plate osteosynthesis, intramedullary nailing may be superior for reducing blood loss and postoperative infections [5]. However, due to more movement at a fracture site with an intramedullary nail, plate fixation is regarded as superior in preventing nonunion in comparison with intramedullary nail fixation [5,6].
The surgical approach for humeral nonunion after operative treatment is extremely challenging because of the complex neurovascular anatomy and the possible necessity of osteosynthesis removal. In this report, a rare case of humeral nail bending after secondary trauma in a patient with preexisting nonunion of the humerus is presented.
CASE REPORT
Initially, a 71-year-old, right-hand-dominant male patient presented to the Department of Accidents and Emergency following an ice-skating accident. The patient had made a misstep and fell on his left arm. Directly after the injury, he complained of pain and his upper arm showed a deformation. The neurovascular function of his arm was intact on clinical examination. An X-ray showed a bending wedge fracture of the humeral diaphysis with a butterfly fragment on the medial side (AO-12-B2) (Fig. 1). Closed reduction and internal fixation were performed using a long MultiLoc nail (270 mm) with two screws proximally as well as distally. Adequate reduction could be achieved during this procedure. The butterfly fragment was located sufficiently and the implant position was secured. Postoperatively, no complications occurred. During outpatient follow-up, the bone seemed to be healing well 2 months after surgery (Fig. 2A). After 6 months, his range of motion was unrestricted. An X-ray examination showed delayed union of the fracture (Fig. 2B). Because the patient had no pain or other symptoms at this stage, no intervention was done and a wait-and-see policy was applied.

X-ray showing an oblique fracture of the humeral diaphysis with a butterfly fragment on the medial side.
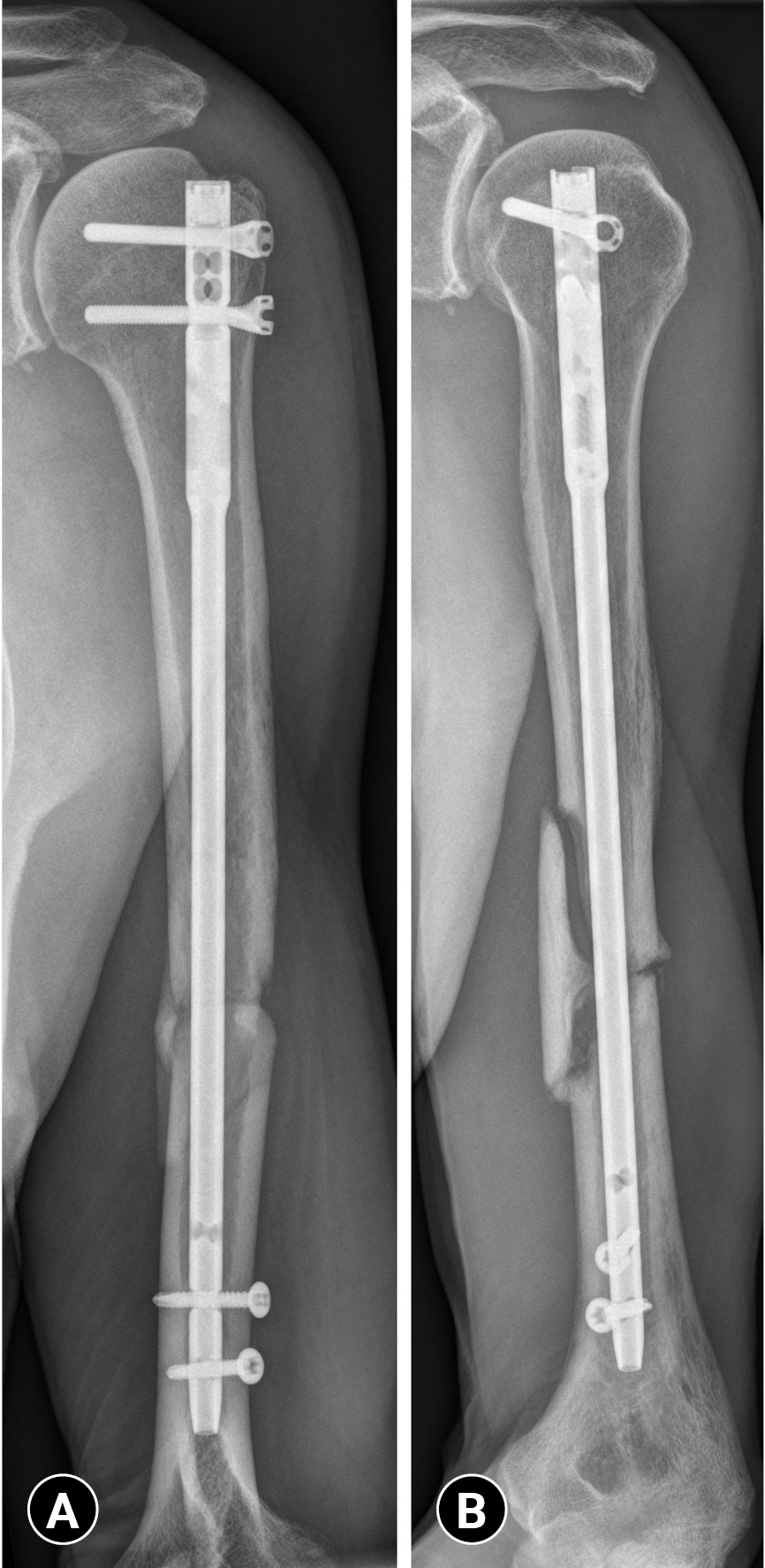
Postoperative radiographs (A) after MultiLoc fixation (2 months), showing (B) delayed union (6 months).
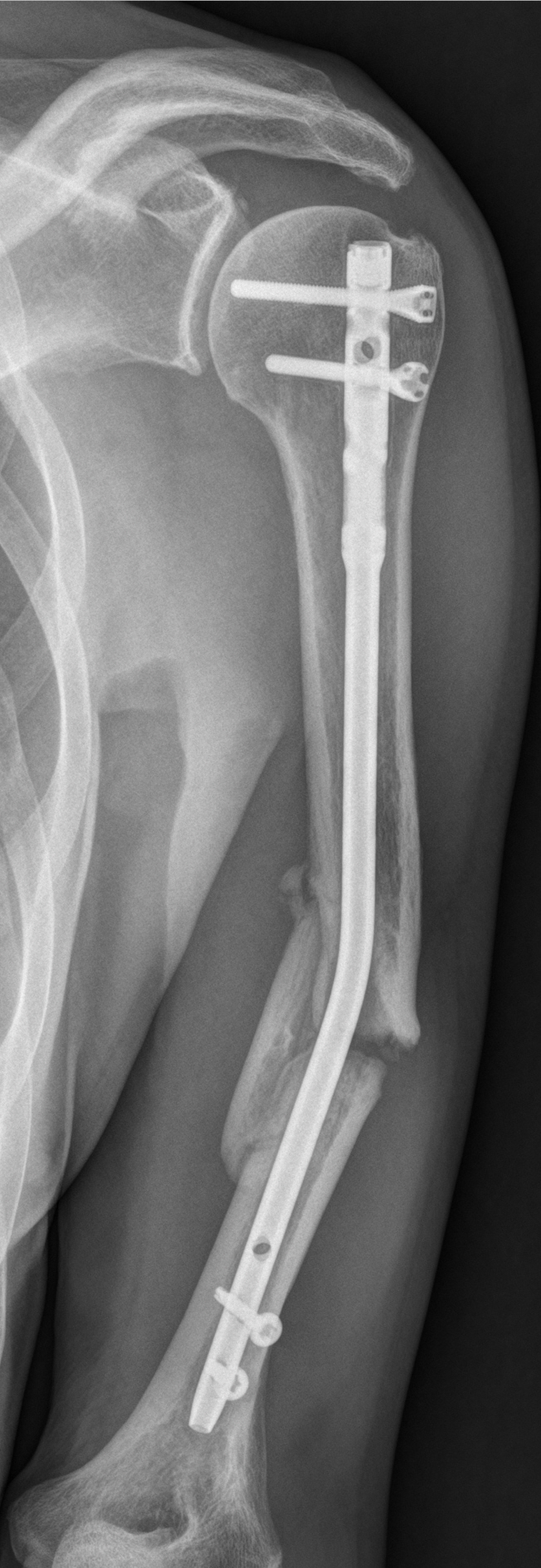
However, 1 year after initial surgery, the patient experienced a new trauma to his left arm during a second fall while ice-skating. Upon presentation to the Accidents and Emergency Department, he was in pain and had restricted movements of the upper arm. An X-ray revealed a bent humeral nail with nonunion of the humerus (Fig. 3). The image suggested that the nail was intact but had undergone plastic deformation. The patient consented to a second operation.
The second procedure was performed with the patient in the prone position, with the injured arm hanging over a cushion, using a posterior triceps-sparing approach to the humeral shaft. First, the distal screws were removed. Then, the nonunion was explored and hypertrophic callus formation was removed. The bent nail was now visible and could be sawed in half. During this phase, the tissues and bone were cooled using sterile ice water (normally used by the cardiothoracic surgical team). The aim of cooling was to prevent thermic injury to the tissues, which would negatively influence the healing potential in the future. The distal part of the intramedullary nail could now be removed without any difficulty. The proximal part was left in place because removal of the proximal screws would mean that the patient’s position would have to be changed and additional damage to the soft tissue (and rotator cuff) could occur. Re-assessment of the nonunion site showed that compression was possible while using plate fixation. Adequate stability and compression were assessed to be necessary to achieve bone healing. Bone grafting was deemed unnecessary because of the hypertrophic character of the nonunion [7]. Therefore, no bone grafting was applied; however, compression was achieved and the possible shortening of the humerus during this procedure was accepted. Eventually, absolute stability was achieved by using a Zimmer Cable Ready plate fixation system (Zimmer Biomet, Warsaw, IN, USA; eight holes, 246 mm) on the dorsal humerus shaft. Distally, three angle-stable screws were used, while proximally three cortical screws with cable grip fixation were applied so that the proximal part of the nail could be kept in place (6 weeks after surgery) (Fig. 4A). The radial and ulnar nerves were exposed perioperatively and protected during closure. In total, the operation took 2.5 hours and there was 0.4 L of blood loss.

X-ray showing postoperative consolidation of the humeral diaphysis with the dorsal shaft plate and proximal half of the nail in place. Postoperative (A) 6 weeks, (B) 4 months, and (C) 1 year.
Postoperatively, the patient developed sensory loss in his fifth finger and the ulnar part of the fourth finger without any motor loss. There were no abnormalities of the ulnar nerve on ultrasound localisation. On electromyography, axonal neuropathy was seen. Consequently, his complaints were interpreted as axonotmesis of the ulnar nerve. Due to a Martin-Gruber anastomosis, additional compensation of sensation and function was possible and no peripheral neurosurgery was performed. Approximately 4 months after the operation, partial consolidation was seen (Fig. 4B). One year after surgery, during follow-up in the outpatient clinic, the patient had a full range of motion again and was very satisfied with the results. An X-ray examination and computed tomography scan showed complete healing of the fracture (Fig. 4C). After 2 years, the function of the ulnar nerve had returned to normal.
DISCUSSION
Removal of a bent or broken intramedullary nail is a rare but challenging problem. Several case reports have reported the management of this condition in the lower extremity [8,9]. However, to the best of our knowledge, bending of a humeral nail has not previously been reported. Currently, there is no review or algorithm that provides guidance on how to manage patients with this problem.
Various mechanisms have been described as potential causes of intramedullary nail failure [10]. Bending of an intramedullary nail is most commonly linked to trauma, while breakage of the nail primarily occurs in cases of nonunion and unstable or pathologic fractures due to metal fatigue [11,12]. This condition is generally the result of repetitive cycles of stress. Patient characteristics such as age, bone quality, smoking, and alcohol abuse influence this process as well. Nevertheless, in most cases, a fracture of the bone will happen, rather than implant bending itself.
Revision surgery in cases with bending of a nail is complex and challenging. The extraction of a bent nail seems to be more complicated than removing a broken nail because deformation usually results in blockage of the intramedullary canal [13,14]. Furthermore, soft-tissue damage and associated lesions may be expected in these situations. In our case, we chose to partially extract the nail, remove the hypertrophic tissue, and perform open reduction and internal fixation by plate osteosynthesis. Removing the distal part of the nail by sawing it in half was crucial for adequate reduction of the fracture. One should acknowledge that sawing of a nail requires special equipment, and that metal debris, thermal injury, and soft-tissue injury can occur during this process. We advise using a small circular saw and cooling the nail and surrounding tissues with sterile ice water. In our case, we decided to keep the proximal part in place for several reasons. First, plate fixation with a cable fixation system resulted in a compression-type stable situation allowing the hypertrophic nonunion to heal with adequate bone healing. Second, removal of the proximal part of the nail required repositioning of the patient (from prone to supine). This maneuver would possibly be a risky event, since the combination of an unstable humerus and the sharp end of the nail could injure the surrounding soft tissue. Moreover, before the second fall, the patient had recovered without limitations in shoulder function. Therefore, we did not want to risk additional damage to the rotator cuff.
Another major challenge in this injury was the preexisting nonunion. The first principle in this type of nonunion should be removal of the fibrinous tissue at the fracture site, which interferes with bone bridge formation [15]. During exploration of the nonunion site, a hypertrophic nonunion was diagnosed with large bony activity surrounding the nonunion without bridging the gap. The diamond concept was applied for an adequate assessment of compression and stabilization of the nonunion site (and ultimately bone healing). The plate was placed via a posterior triceps-sparing approach (triceps-on) to the humeral shaft allowing adequate exposure of the nonunion. The applied approach was chosen based on the surgeon’s preference, the position of the nonunion, and the bending of the nail. In our case, the plate was placed primarily on the dorsal side. Alternative approaches, such as from the anterior side, could have been considered as well.
In general, we advise discussing these cases in a team with trauma and/or orthopaedic surgeons. Since there is no uniform treatment practice, combining the strengths of various specialists ultimately benefits the patient. Furthermore, hospital-wide support, including peripheral neurology specialists, physiotherapy, and casting technicians, is essential to provide good clinical care for these patients.
This is an exceptional case of humeral nail bending in an older man after re-injury of his left upper arm. A second operation with removal of the distal nail and obtaining absolute stability by cable-ready plate fixation was performed to achieve fracture healing with good clinical results.
Notes
Ethical statements
Written informed consent for publication of the research details and clinical images was obtained from the patient.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: all authors; Visualization: AG; Writing–original draft: SW; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Acknowledgements
We appreciate all the resident doctors of the departments of surgery and anesthesia, the nursing staff in the operating room, intensive care unit and the surgical wards that assisted in the management of this patient.