Incidental traumatic right diaphragmatic rupture: a missed case after trauma
Article information
Abstract
Traumatic diaphragmatic hernia is among the most uncommon conditions after severe trauma, and it is associated with high morbidity and mortality. The diagnosis is difficult and might be missed, but a multimodal investigation might help in terms of diagnostic yield. In this case report, we present a missed right diaphragmatic rupture 14 years after the trauma.
INTRODUCTION
Severe trauma can cause diaphragmatic rupture, along with other abdominal or chest injuries. A ruptured diaphragm is associated with high morbidity and mortality, and its diagnosis is crucial. Hence, many cases in the literature have been published to help identify and manage this rare condition.
CASE REPORT
A 20-year-old female patient known to have asthma presented to Tawam Hospital as a referral for her incidental missed traumatic right diaphragmatic hernia. The patient had a motor vehicle accident in another country 14 years ago. There was no report of her injuries, but according to the family and the patient, she had right hemothorax that was treated with the insertion of a chest tube.
The patient had a recurrent cough, shortness of breath, and fever. The initial assumption was exacerbation of her asthma and her ingestion of raw camel milk.
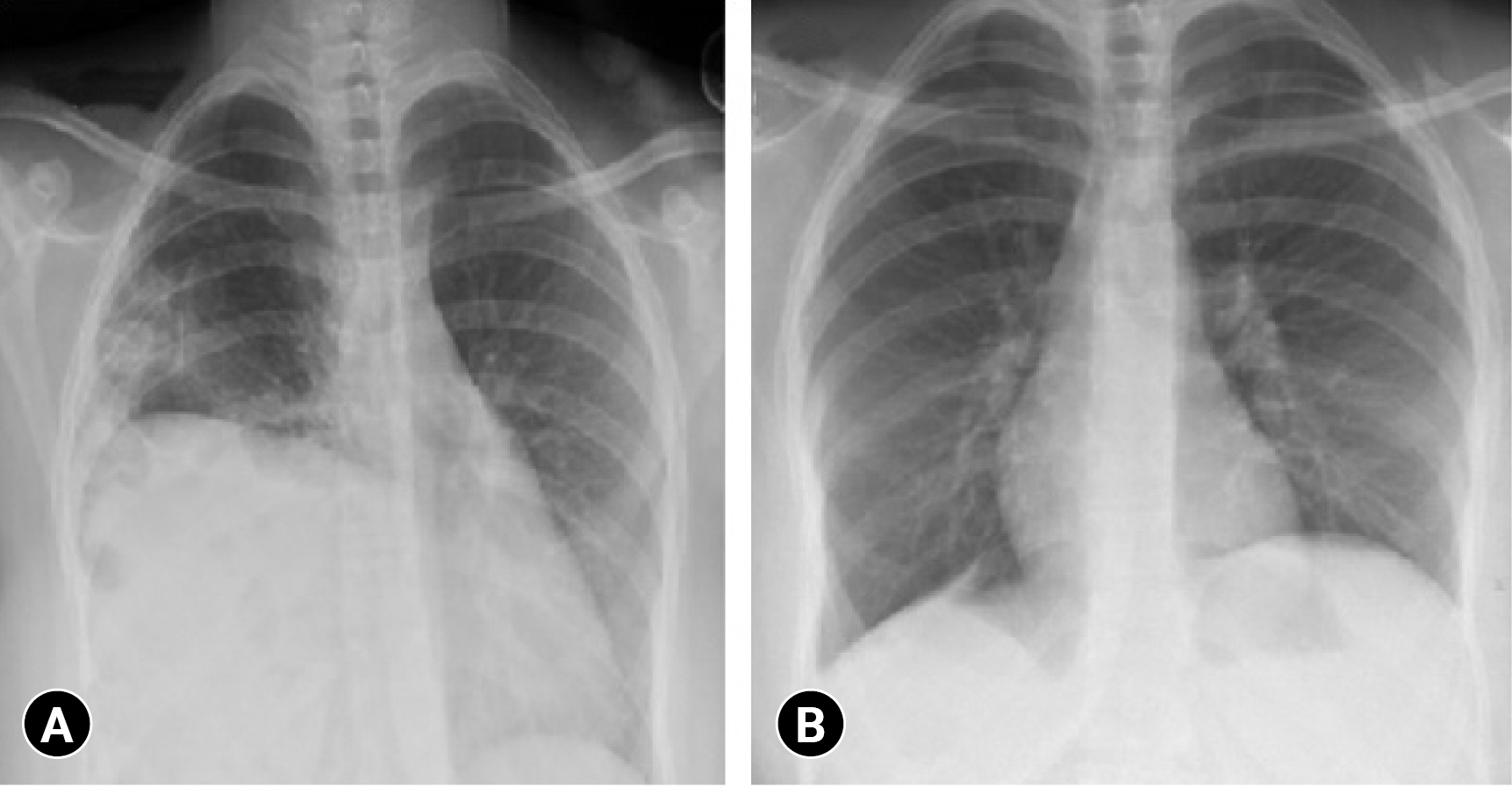
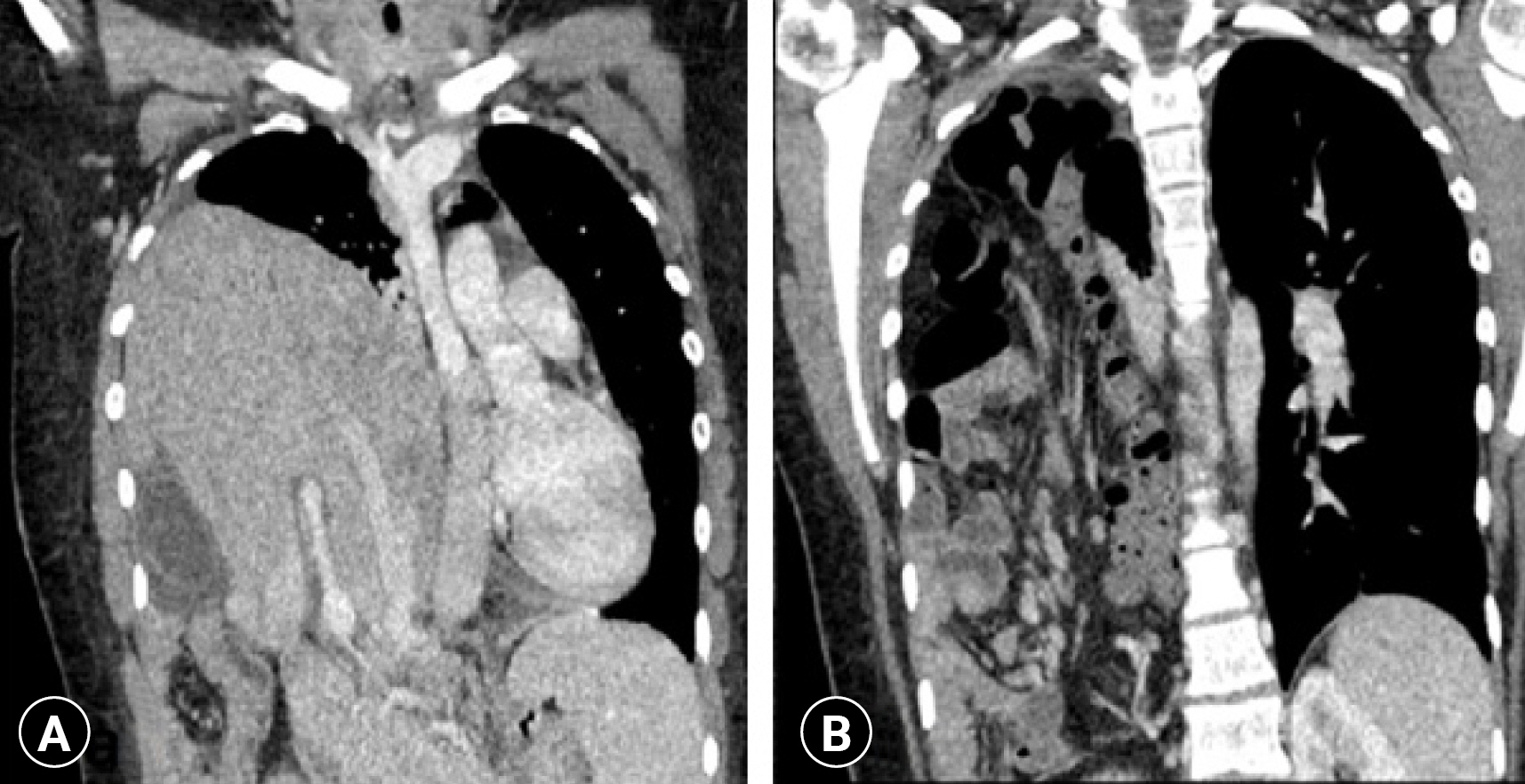
Initially, a chest X-ray was done, which showed an elevated right hemidiaphragm (Fig. 1). Computed tomography (CT) was obtained and it showed a large defect in the right dome of the diaphragm, predominantly in the posterior two-thirds, with herniation of the right lobe of the liver and presence of the small and large bowel in the thoracic cavity. The herniated right lobe of the liver was seen displacing the mediastinum to the left. There was atelectasis of the right middle lobe and near-complete atelectasis of the right lower lobe, while the left dome of the diaphragm was normal in continuity (Fig. 2).
The patient was referred to the thoracic surgery department for definitive management, but unfortunately, she was lost to follow-up until recently when she agreed to operative management due to exacerbation of her respiratory symptoms. The decision regarding the operation was to repair the defect through the abdomen depending on the CT findings of the liver and other organs in the chest. This was also discussed with the thoracic surgery team, and it was agreed to perform the repair through the abdomen. The patient had a very long-standing diaphragmatic hernia, and was short and obese (body mass index, 31 kg/m2); therefore, we were concerned about possible loss of the domain and we thought that the abdominal cavity might not have enough space to accommodate the abdominal organs after reduction. We were prepared to resect the greater omentum, leave the abdomen open, or even consider partial liver resection if needed. Surgery was started using the laparoscopic technique, which was converted to open surgery with a midline incision because the hernial defect was obscured by the liver. The intraoperative findings showed the full right lobe of the liver, as well as the gallbladder, in the right thoracic cavity and multiple loops of the small bowel and ascending and transverse colon in the right thoracic cavity (Fig. 3). The stomach was redundant, distended, and reached the pelvic cavity. A large right diaphragmatic hernial defect was seen, with the posterior edge of the defect attached to the upper posterior surface of the liver (segments 7 and 8). The portal system ran along the posterior edge of the hernial defect longitudinally and the inferior vena cava and aorta just at the medial edge of the defect.
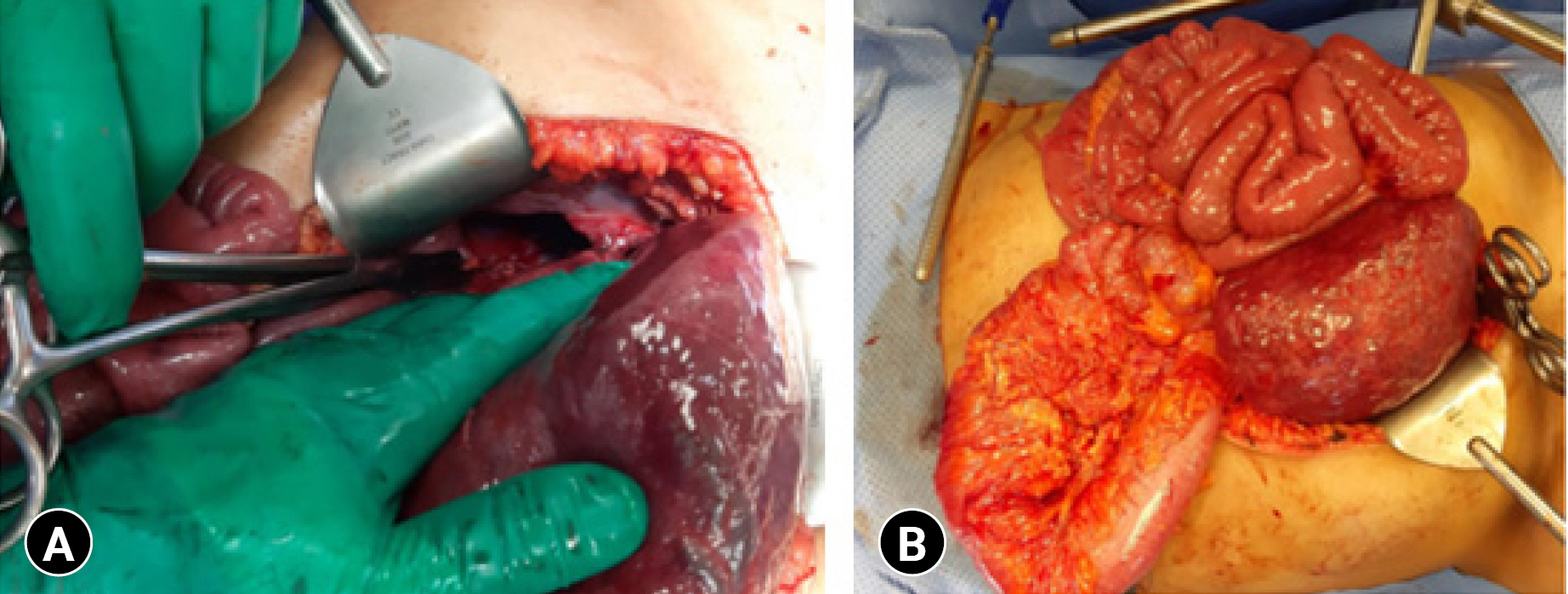
Intraoperative findings of the liver and the bowel (A) in the thoracic cavity and (B) after reduction.
Adhesiolysis was done by cautery, and all organs were reduced to the abdomen. Primary repair of the diaphragm was done with no tension using 2-0 Prolene continuous sutures and reinforce using a composite mesh cut to an appropriate size. Cholecystectomy was performed, as the wall of the gallbladder was thickened and edematous; pathology later showed chronic cholecystitis. The patient did well after surgery with no further complaints about the respiratory symptoms that she previously experienced before surgery. A chest X-ray was repeated 6 months after surgery and showed no recurrence (Fig. 1B). The patient provided written informed consent for publication of the research details and clinical images.
DISCUSSION
Right traumatic diaphragmatic rupture is a rare condition, which is missed most of the time due to the difficulty in the diagnosis and the need for further investigations [1]. The causes of diaphragmatic rupture can be divided into direct diaphragmatic trauma (penetrating injuries such as a direct stab wound to the diaphragm or a gunshot) and indirect diaphragmatic trauma (blunt trauma) [2]. Injuries contributing to the development of diaphragmatic rupture include motor vehicle accidents (79.5%) and falls from heights (15.9%) [3].
The diagnosis of traumatic diaphragmatic rupture is indicative of severe trauma that has caused the intraabdominal organs to translocate into the thoracic cavity [4]. Up to 3.6% of cases with traumatic diaphragmatic rupture are due to blunt traumas, although around 66% of them are missed [3].
Most cases of diaphragmatic rupture occur on the left side (75%), with the spleen being the most common injured organ [5]. Due to the cushioning effect of the liver on the right side, injuries to the right diaphragm are less traumatic, which is why right diaphragmatic rupture is less common [6]. Nevertheless, an increase in the number of reported cases of right diaphragmatic rupture has been noticed, mostly due to the improvement of posttrauma investigations and high clinical suspicion [5].
The diagnosis of traumatic diaphragmatic hernia is mostly missed. The cases that are not missed are diagnosed either preoperatively (39%) or intraoperatively (45%), during either first-look or second-look surgery [7].
Imaging studies and a high suspicion for these injuries can help in the diagnosis. Initially, a chest X-ray with an abdominal X-ray might show the diaphragmatic rupture by capturing the elevated hemidiaphragm with or without the presence of intraabdominal organs in the chest, while the use of CT might be more appropriate for the diagnosis. A previous study suggested that in up to 59% of cases, a chest X-ray was an inconclusive method, whereas a CT scan showed the defect in the diaphragm [8].
Since the diagnosis of diaphragmatic rupture is important to prevent posttrauma diaphragmatic hernia and other serious complications such as strangulation of the ascended organs [9], other modalities such as ultrasonography and magnetic resonance imaging might be indicated. Nevertheless, the use of magnetic resonance imaging might be limited due the need for continuous monitoring and the patient’s condition, while the use of ultrasonography might be helpful in detecting the functional status of the diaphragm and the presence of intraabdominal organs in the thoracic cavity [10].
The surgical management of ruptured diaphragmatic injury depends on the patient’s condition and the presence of other injuries. The surgical approach can be divided into the abdominal approach (laparotomy or laparoscopy), which is appropriate for unstable patients with abdominal injuries, and the thoracic approach (thoracotomy or thoracoscopy) in cases with isolated chest injuries and a late diagnosis [3,5].
The main objective of surgery is to reduce the organs, drain the pleural fluid, and repair the defect with nonabsorbable sutures with or without the placement of mesh [11]. However, there are some cases presented in the literature in which the surgeons preferred using only nonabsorbable sutures without mesh placement due to the elevated risk of infection [12].
In summary, right diaphragmatic rupture is an uncommon condition. A multimodal investigation combined with a high degree of clinical suspicion is indicated for a proper diagnosis. Treatment is surgical and depends on the patient’s status and the presence of other injuries.
Notes
Ethical statements
Written informed consent for publication of the research details and clinical images was obtained from the patient.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: all authors; Formal analysis: all authors; Investigation: all authors; Writing–original draft: FA, SG; Writing–review & editing: all authors. All authors read and approved the final manuscript.