Types of injuries caused by isolated electric scooter accidents
Article information
Abstract
Purpose
The recent increase in electric scooter (e-scooter) use has been accompanied by an increase in injuries from e-scooter–related accidents. Studies have reported that most such injuries are minor, and physicians may therefore underestimate the severity of such injuries. This study investigated the types and severity of injuries caused by isolated e-scooter accidents (i.e., those that did not involve colliding with other cars or falling from heights).
Methods
This prospective observational study was conducted from May to December 2021 at Dankook University Hospital tertiary medical center. The demographic data of patients injured in isolated e-scooter–related accidents were collected. All injuries were categorized by body part.
Results
Fifty eligible patients visited our emergency department during the study period. Of these, 76% were categorized as nonemergency, and 62% were discharged after initial evaluation and treatment at the emergency department. Another 10% were admitted to the intensive care unit (ICU) and 18% to the ward, with nine patients receiving at least one operation. The average hospital stays were 2.4 days in the ICU and 9 days in the ward. One death occurred due to traumatic brain injury (overall mortality rate, 2%). Multiple fractures of the left third through ninth ribs combined with lung laceration and fractures of T12 and L4 were noted.
Conclusions
Various types and severities of injuries can occur in isolated e-scooter accidents. While most such injuries are minor, some will require ICU admission or surgery, and deaths can occur. Physicians should not underestimate the severity of such injuries.
INTRODUCTION
There are various types of electric-powered personal transport devices, including unicycles, bicycles, hoverboards, scooters, and Segways. Interest in personal transport devices has been rising recently, in part due to limitations on social activities and other personal behavior changes related to the coronavirus disease 2019 pandemic. In Korea, for example, the use of electric scooters (e-scooters) has been increasing (Fig. 1). This growth has been driven by several factors, including personal enjoyment, the environmental friendliness of such low carbon-emitting vehicles, and the public availability of e-scooter service mobile applications. With this growth has come an increase in injuries related to personal mobility-related accidents [1–6]. In a multicenter study conducted in Korea, the frequency of e-scooter injuries increased from 3.1 injuries per 100,000 population in 2014 to 100.3 per 100,000 population in 2018 [2]. According to another study, the number of e-scooter injury patients more than tripled in 2017 compared to 2016 [7]. Since 2018, most papers published worldwide that have reported on e-scooter injuries have dealt with personal mobility-related accidents more generally. [8]. Articles looking specifically at isolated e-scooter injuries have been scarce, and research specific to Korea is apparently nonexistent. Generally, physicians approach and evaluate patients injured riding e-scooters with an eye to major trauma if they have had high energy accidents, such as colliding with another vehicle or falling from a significant height. It is possible, however, that physicians may be underestimating the severity of some e-scooter–related injuries, in part because studies show that most injuries from e-scooter–related accidents are minor [8–11], but also because e-scooters are generally used for leisure activities, short distances, and at relatively low velocities (20–40 km/hr), This study, therefore, investigated the types and severity of injuries caused by isolated e-scooter accidents, which are often considered minor.
METHODS
Study design
This is a retrospective observational study on prospective data collected from May to December 2021. It was conducted at the regional emergency center and level I trauma center affiliated with Dankook University Hospital, which is an academic tertiary medical center. Approximately 40,000 to 45,000 patients visit our emergency department (ED) each year. During the study period, we collected the data on patients injured in isolated e-scooter–related accidents. Patients who had fallen from their scooter, collided with walking or standing people, or collided with a stationary building, pillar, or column were included. Those who had collided with other vehicles or fallen from a significant height while riding their e-scooter were excluded, as were those who had been riding manual scooters. Data recorded included age, sex, accident location, injury mechanism, protective devices, operations needed, and hospital stay length. As drivers in Korea often use e-scooters to travel to their offices or other places of work, their occupations were also recorded. After initial evaluation and treatment, the patients’ injuries were categorized by body part. Head, face, and tooth injuries were categorized as “head and neck.” Chest, abdomen, pelvis, and clavicle injuries were categorized as “chest and abdomen.” Other injuries were categorized as “upper extremity,” “lower extremity,” or “spine.” Institutional Review Board approval and informed consent were not required as no other personally identifying information besides age and sex was gathered.
Statistics
Categorical data were expressed as number (%), whereas numerical data were represented as mean±standard deviation. IBM SPSS ver. 26.0 (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Frequencies were compared using the Fisher exact test. A P-value below 0.05 was considered to indicate statistical significance.
RESULTS
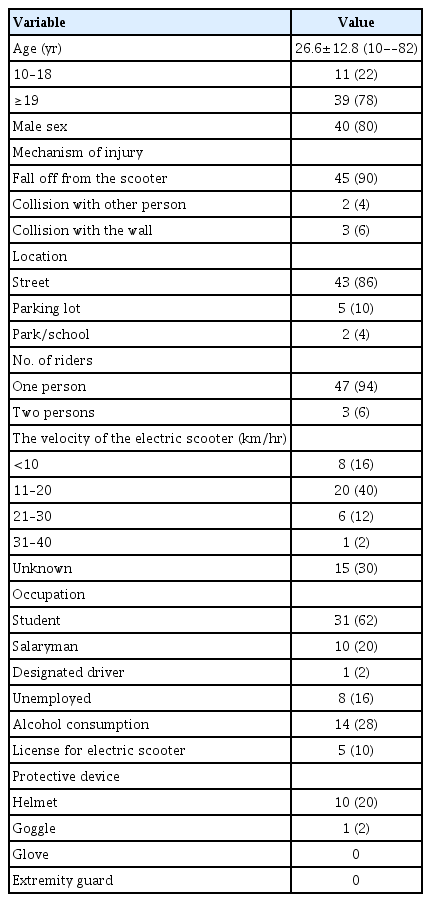
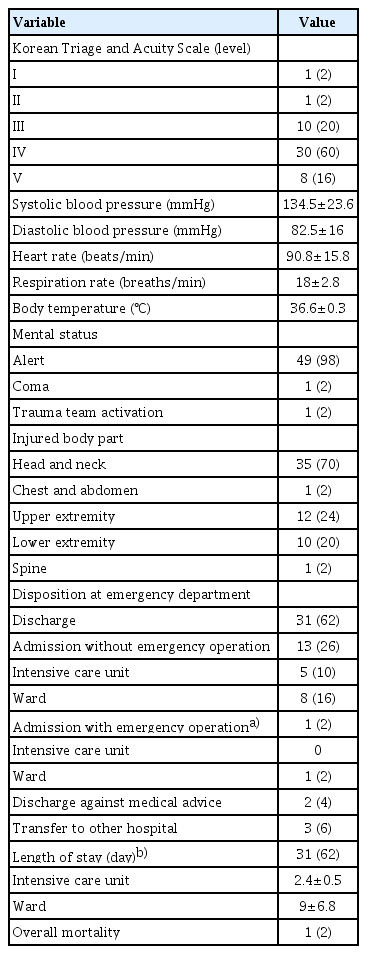
During the study period, 50 patients injured by isolated e-scooter accidents visited our ED, 40 (80%) of whom were male. The mean age of these patients was 26.6 years (range, 10–82 years) (Table 1). Of the 50 patients, 45 (90%) had fallen off their e-scooter due to a simple loss of balance, while the others were injured due to collisions. Most of the accidents (43 cases, 86%) took place in the street. Three accidents (6%) occurred while two riders were on board. In eight cases (16%), the e-scooter velocity at the time of the accident was below 10 km/hr, while in 20 cases (40%) it was 11 to 20 km/hr, and in seven cases (14%) above 20 km/hr. Fourteen patients (28%) had high blood alcohol levels at the time of their accident, and five (10%) had licenses. Ten (20%) wore helmets and one of them also wore goggles. None of the patients wore other protective devices such as gloves or extremity guards. Two patients (4%) were designated as Korean Triage and Acuity Scale (KTAS) level I or II, 10 (20%) as level III, 30 (60%) as level IV, and eight (16%) as level V. Overall, 38 patients (76%) were categorized as nonemergency (KTAS levels IV, V) (Table 2). One patient was in a coma; the others were alert. Thirty-one patients (62%) were discharged after initial evaluation and treatment at the ED, five (10%) were admitted to the intensive care unit (ICU), and nine (18%) to the ward. Nine patients were operated on (one emergency operation and eight elective operations). The average hospital stay was 2.4 days in the ICU and 9 days in the ward. The overall mortality rate was 2% (one patient from a traumatic brain injury).
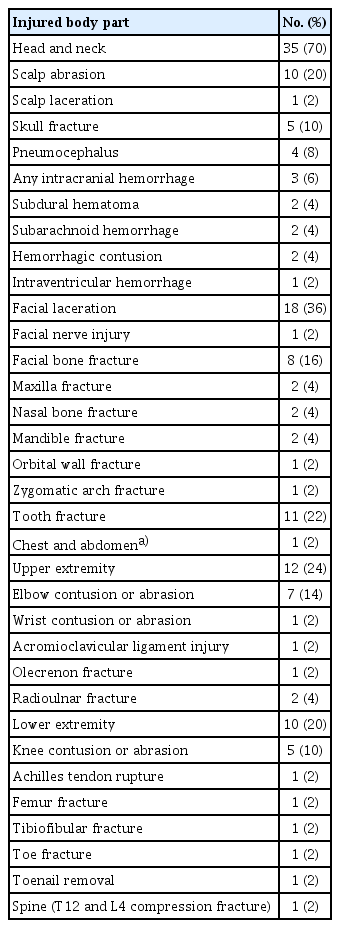
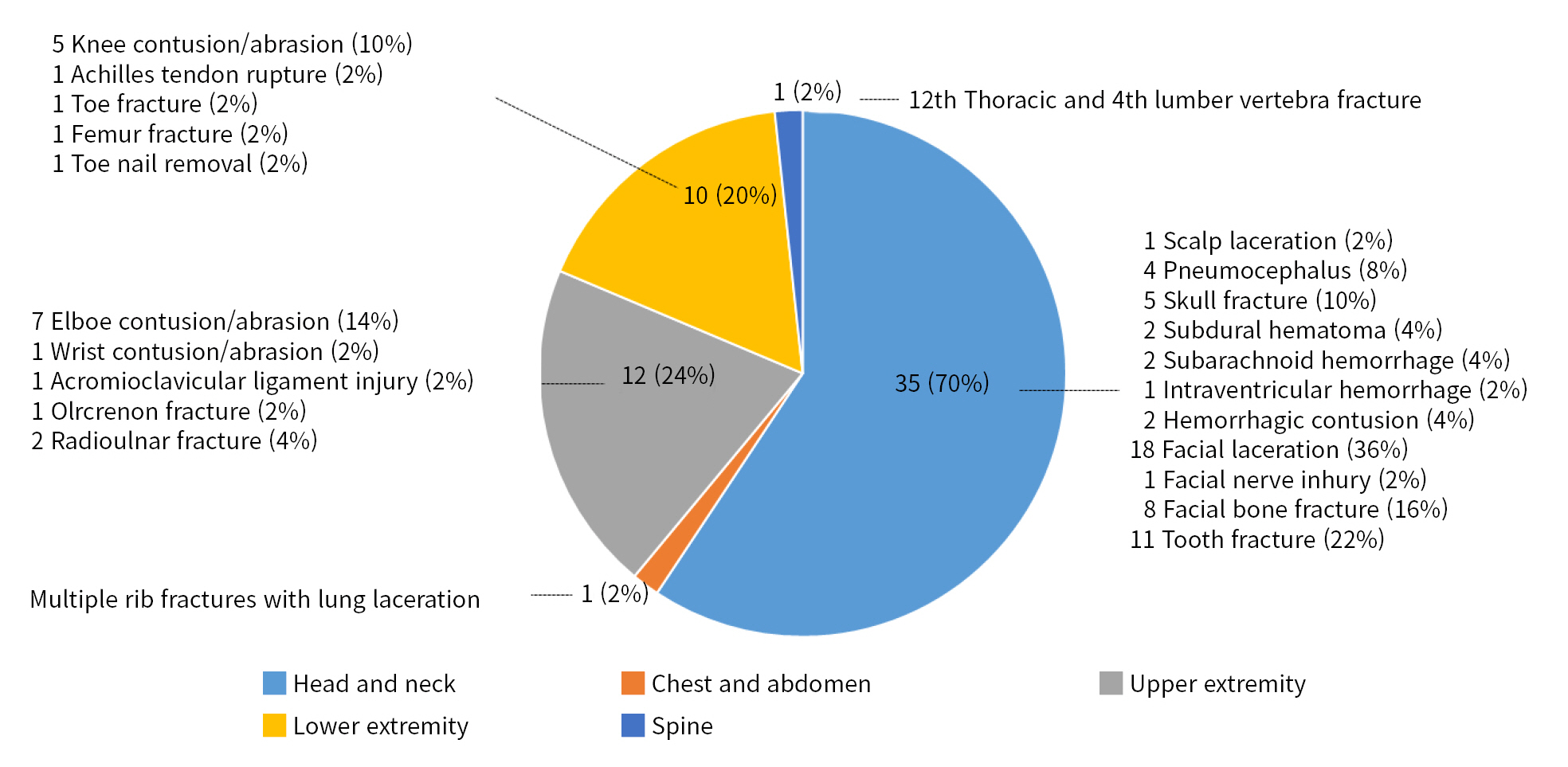
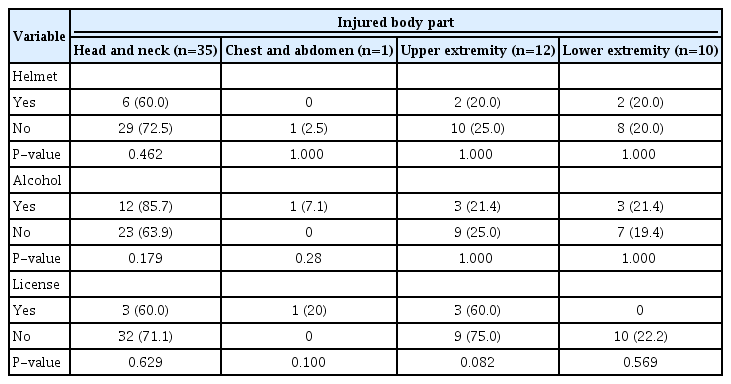
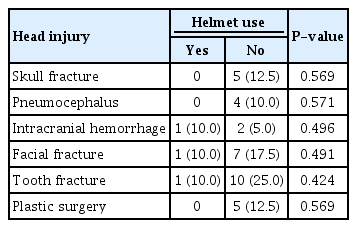
The most common injury categories were head and neck (35 patients, 70%), upper extremities (12 patients, 24%), and lower extremities (10 patients, 20%). Chest and spine injuries were noted in one patient each. Of the head and neck injuries, facial laceration was the most common with 18 cases, and tooth injury second with 11 cases (Table 3, Fig. 2). Skull fracture, pneumocephalus, and intracranial hemorrhage (3 cases, 6%) were noted. Multiple fractures of the left third through ninth ribs combined with lung laceration were noted in one patient (Fig. 3). Elbow abrasion or contusion was the most common upper extremity injury. Ligament injuries and fractures were observed in four cases (8%). Abrasion or contusion of the knee was the most common lower extremity injury. Fractures of the femur, toe, and tibia/fibula were also noted in one patient each. Toenail removal and rupture of the Achilles tendon also occurred in one patient each. A fracture of T12 and L4 vertebrae was noted.
Images of the chest computed tomography of the patient with multiple rib fractures. (A, B) Multiple rib fractures (white arrows) and lung laceration (black arrow) were seen.
No patient received a neurosurgical intervention. Plastic surgery for facial bone fractures was performed in five patients. Two upper extremity and two lower extremity operations (Achilles tendon rupture, femur fracture) were performed. No statistically significant correlations were found between the location of injuries in terms of body part and helmet use, alcohol consumption, or e-scooter license status (Table 4). Likewise, skull fracture, pneumocephalus, intracranial hemorrhage, facial fracture, tooth injury, and plastic surgery incidence did not show statistically significant relationships based on helmet use (Table 5).
DISCUSSION
In isolated e-scooter accidents, the severity of riders’ injuries may be disproportionately overlooked because many reports suggest that these injuries are minor and occur at a relatively low speed of travel [8]. This study, therefore, was conducted to obtain more definitive information about injuries caused by isolated e-scooter accidents.
In our study, the youngest patient was 10 years old, but most of the children who presented to our ED were excluded because the study was limited to e-scooters. Children mainly ride manual scooters, whereas teenagers and adults mostly use e-scooters. Most of the patients (90%) lost their balance and fell off their scooters. The other 10% were two cases of colliding with another person and three cases of colliding with a wall. Ten patients (20%) wore helmets, with only one of them also wearing goggles, and none of them used limb protection or any other protective devices. The rate of helmet use was only 20%, despite the fact that in Korea, protective devices and licenses have been mandatory when riding an e-scooter since May 2021, and this study took place after that. The rate of helmet use seemed to have increased slightly compared to the 3% reported in previous domestic studies [2,7], but it was still low. Legal regulations need to be strengthened.
When they arrived at the ED, 76% of patients were designated nonemergency (KTAS levels IV, V), and 98% were alert. After ED treatment, 62% were discharged on the same day. In other words, most patients with isolated e-scooter accidents had minor injuries. The other 28% of patients were hospitalized, however, and 10% were treated in the ICU. Surgery was performed in 18% of cases (five plastic surgery, four orthopedic surgery), and the overall mortality rate was 2% (one patient). Head and neck injuries were the most common, followed by upper extremity injuries. This is consistent with other studies [7,8,12]
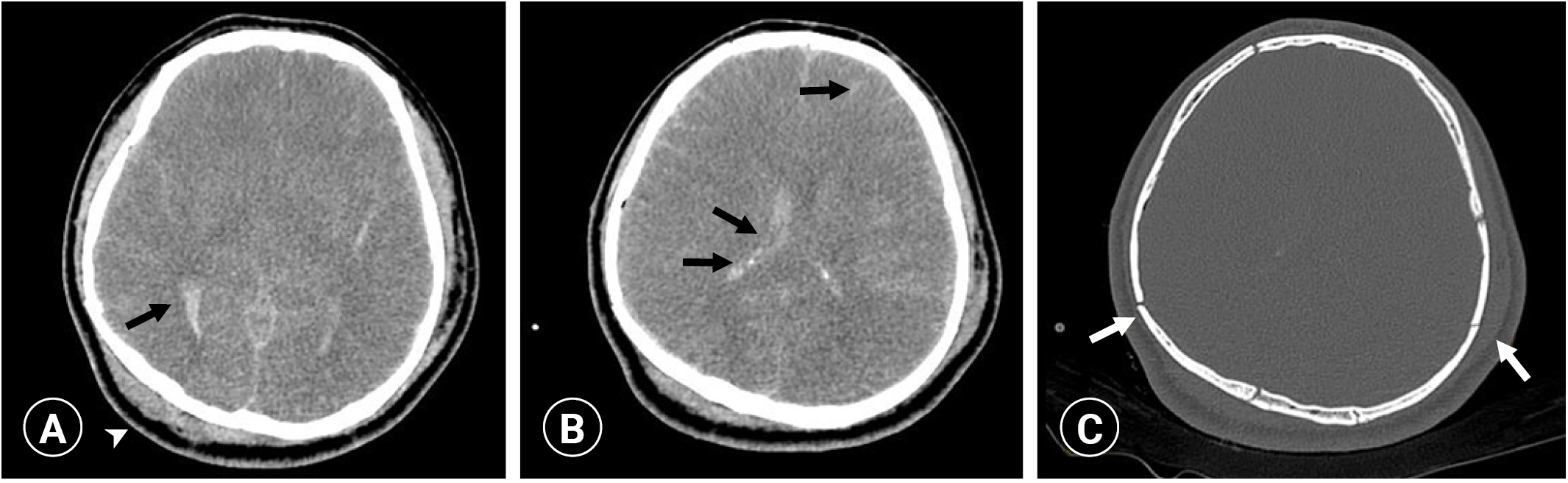
In the 70% of patients with head and neck injuries, there were mostly minor injuries such as facial lacerations, tooth injuries, and scalp abrasions, with some intracranial bleeding (three cases). No patients received neurosurgical intervention. Two cases were managed conservatively, and one case had severe cerebral edema with a low chance of being resuscitated or regaining consciousness, making surgery impossible (Fig. 4). This 27-year-old male patient, who had not been wearing the helmet, died 3 days later. His accident was captured by a nearby closed-circuit television camera, which showed him hitting his head on the ground while falling alone on the road. so it was confirmed that the accident met the study criteria for classification as “isolated.” When brought to the ED, this patient was in a coma and had nasal fractures. Deaths have rarely been reported in other scooter-related reports. One domestic personal mobility study mentioned death but gave no details of a specific injury mechanism or site [2]. In this study, one additional case had a facial fracture with a facial nerve injury; this patient was treated with an emergency operation (open reduction and internal fixation with neurorrhaphy).

Images of the brain computed tomography of the comatose patient. (A, B) Severe brain edema and subarachnoid hemorrhage (black arrows), and scalp swelling (arrowhead) were observed. (C) Multiple skull fractures (white arrows) were also noted.
Helmet use made no statistically significant difference in the incidence of skull fracture, pneumocephalus, intracranial bleeding, facial fracture, tooth injury, or plastic surgery. However, caution is needed in interpreting this finding. First, it is possible that victims wearing helmets were less likely to visit the hospital because their injuries tended to be more minor. Second, the finding of no statistically significant difference may have only been because of the small sample size. In our study, skull fracture, pneumocephalus, and plastic surgery did not occur at all in the helmet-wearing group. Moreover, there are many reports that using helmets reduces the risk of damage [2,13–15], so it cannot be concluded that wearing helmets is meaningless because this study did not show statistical significance.
Multiple fractures of the left third through ninth ribs combined with lung laceration and zygomatic arch fracture were observed in one case. This 39-year-old female patient who fell alone was discharged after 14 days of hospitalization without surgery. Her injuries were likely specific to her isolated e-scooter injury, as she was a relatively young patient without any underlying diseases such as osteoporosis. Despite their rarity, attention needs to be paid to complications such as cerebral air embolism caused by lung laceration or pneumothorax [16,17].
The most common extremity injury was simple abrasion or contusion, but fractures and Achilles tendon ruptures that required surgery also occurred. There were six cases of extremity fractures in our study, and three (50%) were operated on. This was consistent with an article by Coelho et al. [18] reporting the need for surgery in more than 50% of extremity fractures in e-scooter accidents.
This study has few limitations. First, it was a single-institution study, so it cannot be assumed to apply nationally. A multicenter study is needed to further investigate detailed diagnoses and treatments. Furthermore, the sample size was small, so the frequency of severe injuries and mortality could be overestimated.
As e-scooter use increases, so do accompanying accidents. Various types of injury can occur even in isolated e-scooter accidents. Most of these injuries are minor enough to allow patients to be discharged on the same day; however, some patients need admission to ICU or surgery, and deaths may occur. Physicians, therefore, should not underestimate the severity of injuries from such accidents.
Notes
Ethical statements
Institutional Review Board approval and informed consent were not required as no other personally identifying information besides age and sex was gathered.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: HIK; Formal analysis: HIK; Methodology: KY; Writing–original draft: KY; Writing–review & editing: HIK.
All authors read and approved the final manuscript.