Articles
- Page Path
- HOME > J Trauma Inj > Volume 35(4); 2022 > Article
-
Original Article
An analysis of missed injuries in patients with severe trauma -
EunGyu Ju, RN1
 , Sun Young Baek, MD2
, Sun Young Baek, MD2 , Sung Soo Hong, MD2
, Sung Soo Hong, MD2 , Younghwan Kim, MD2
, Younghwan Kim, MD2 , Seok Hwa Youn, MD2
, Seok Hwa Youn, MD2
-
Journal of Trauma and Injury 2022;35(4):248-254.
DOI: https://doi.org/10.20408/jti.2022.0017
Published online: September 14, 2022
- 1,995 Views
- 72 Download
- 1 Crossref
1National Trauma Center, National Medical Center, Seoul, Korea
2Department of Surgery, National Trauma Center, National Medical Center, Seoul, Korea
- Corresponding to Seok Hwa Youn, MD Department of Surgery, National Trauma Center, National Medical Center, 245 Eulji-ro, Jung-gu, Seoul 04564, Korea Tel: +82-2-2260-7114 E-mail: iguasufalls@daum.net
Copyright © 2022 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- To analyze the data of trauma patients with undetected injuries at the time of initial resuscitation during the primary and secondary surveys.
-
Methods
- We retrospectively reviewed the medical records of 807 patients who were hospitalized at the National Trauma Center, Seoul, Korea from June 1, 2019 to June 30, 2021.
-
Results
- In trauma patients with an Injury Severity Score ≥16 accounted for 27.5% in the non-missed injury group (non-MIG), but this rate was considerably higher at 71.2% in MIG. The mean hospitalization longer in MIG (50.90±39.56) than in non-MIG (24.74±26.11). The proportion of patients with missed injuries detected through tertiary trauma survey (TTS) was 28 patients (23.5%) within 24 hours, 90 patients (75.6%) after 24 hours to before discharge. The majority of missed injuries were fractures (82.4%) and ligament tears (8.4%), which required consultation with the orthopedic department. The final diagnoses of missed injuries were confirmed by computed tomography (44.5%), magnetic resonance imaging (19.3%), X-ray (19.3%), bone scan (11.8%), and physical examination (5.0%).
-
Conclusions
- TTS is considered a useful process for detecting missed injuries that were not identified at the time of initial resuscitation in the primary and secondary surveys. In the future, to detect missed injuries quickly, it is necessary to develop a suitable TTS program for each trauma center. In addition, further research is needed to verify the effectiveness of the protocolized TTS and survey chart to improve the effectiveness of TTS.
- In modern society, various industries have developed economically and technologically. Consequently, the number of patients with trauma caused by industrial accidents, such as falls, slips, hits, stuck in machines, stabs, and traffic accidents, is increasing. In Korea, out of 295,110 deaths in 2019, 27,282 (9.24%) were caused by trauma [1].
- Trauma deaths occur frequently in economically active populations under the age of 44 years. This constitutes a significant social burden [2]. According to a 2006 study, the cost of productivity loss due to injury related premature deaths were approximately ₩8.6 trillion [3].
- The number of patients with severe trauma and Injury Severity Score (ISS) ≥16 increased from 8,803 in 2018 to 9,115 in 2019. As of 2019, 5,004 traffic accidents (54.9%) and 3,416 falls (37.5%) accounted for the majority. Of these, only 4,357 patients (47.8%) survived. Among them, the incidence of severe and moderate disabilities was 2,594 (59.5%), which was higher than that of 1,676 normal recoveries (38.5%) [4].
- Severe trauma poses an immediate threat to a patient’s life if timely management is not provided [5]. However, if initial resuscitation of the patient is prioritized and identified injuries are belatedly discovered, it may affect the relationship of trust with patients and extend hospital days for long-term treatment and rehabilitation. Therefore, this is expected to be a significant burden on both patient’s individual finances and social insurance fund [2].
- Accordingly, the Ministry of Health and Welfare in Korea selected five regional trauma centers in 2012 under the “2010–2012 Emergency Medical Advancement Plan,” and as of 2021, 15 regional trauma centers are in operation. As a result, the preventable trauma mortality rate, which was high at 30.5% in 2015, decreased to 19.9% in 2017, demonstrating a significant improvement [6].
- As a new regional trauma center is planned to open, we investigated missed injuries during the initial resuscitation through a tertiary trauma survey (TTS). In Korea, regional trauma centers individually discuss and conduct TTS; however, this has not yet been published. Therefore, this study aimed to provide basic data for the development of a protocol for effective TTS to diagnose and treat missed injuries by retrospectively analyzing the types and frequencies of injuries identified.
INTRODUCTION
- This study was approved by the Institutional Review Board of the National Medical Center (No. NMC-2021-10-122). The written informed consent was waived due to the retrospective nature of this study. This study was conducted on 807 patients with trauma who were hospitalized at the National Trauma Center, Seoul, Korea from June 1, 2019 to June 30, 2021. Among the patients, 734 patients who did not find missed injury were classified into the non-missed injury group (non-MIG) and 73 patients in 119 injury sites who found missed injury into MIG. Frequency analysis and paired-sample t-test were performed using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA).
METHODS
- In non-MIG and MIG, male patients accounted for 64.7% and 78.1% of the population, respectively. The average age in non-MIG and MIG was 62.9 and 50.7 years, respectively. In particular, the mean ISS was 11.76±8.84 in non-MIG and 22.03±11.76 in MIG, thereby showing a higher score in MIG. The proportion of patients with severe trauma and ISS ≥16 in non-MIG accounted for 27.5% but was considerably higher at 71.2% in MIG. The mean hospital day for non-MIG was 24.74 days and 50.90 days for MIG, which was approximately 2.06 times higher (Table 1).
- Missed injuries were classified into the following three types: type I, not diagnosed in the initial survey conducted immediately after admission but confirmed through a tertiary survey within 24 hours of hospitalization; type II, confirmed from 24 hours after hospitalization to before discharge from the hospital after the tertiary survey; and type III, confirmed after discharge from the hospital (Table 2) [7].
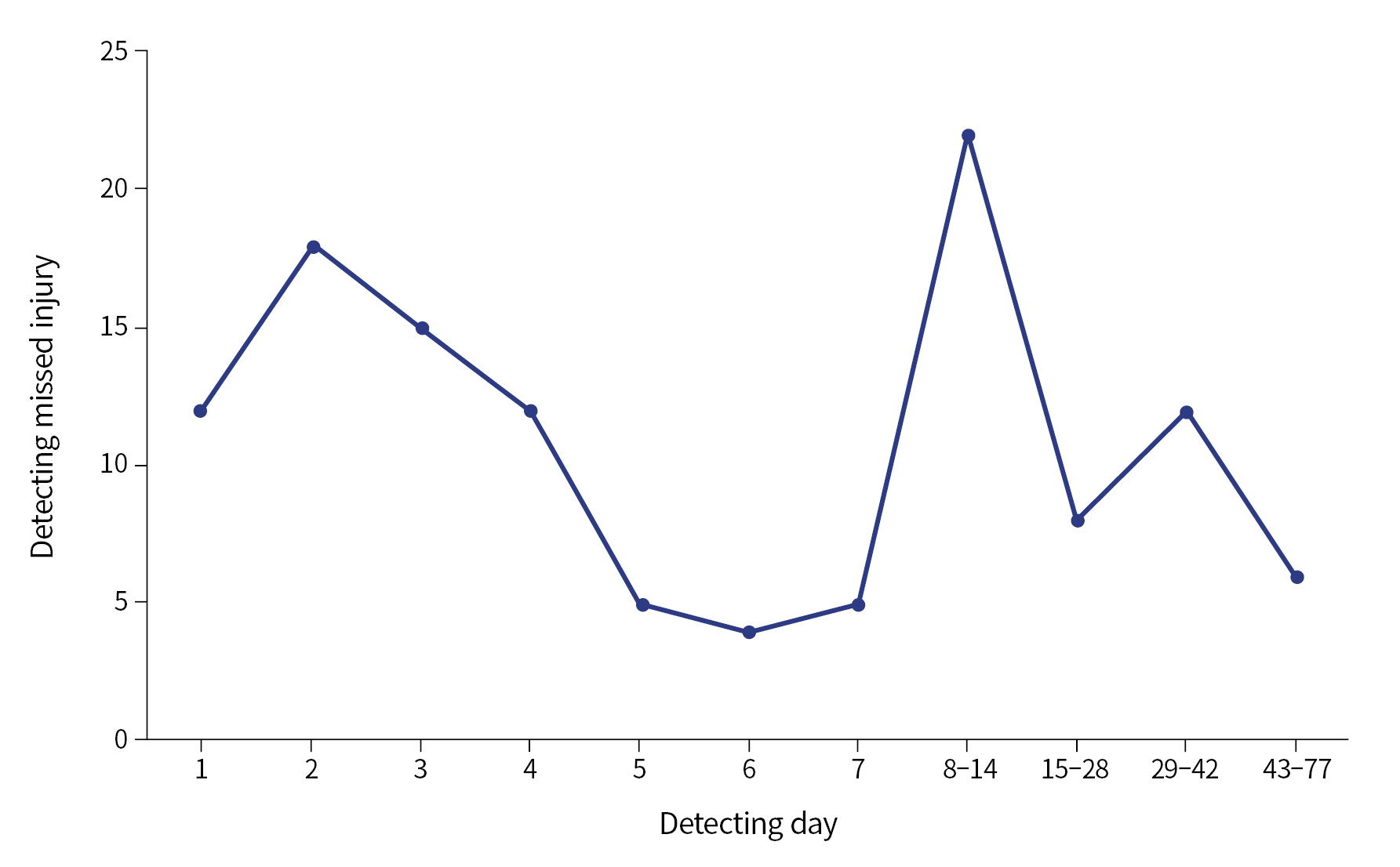
- The characteristics of analysis of the missed injuries are summarized in Table 3. On investigating, 28 cases of injury (23.5%) were type I, 90 cases (75.6%) were type II, and one case (0.8%) was type III. Seventy-one cases (59.7%) were found within the 1st week and 22 cases (18.5%) were found in the 2nd week of hospitalization (Fig. 1).
- On analyzing the kinds of injuries, fractures accounted for the majority with 98 cases (82.4%), followed by ligament tears in 10 cases (8.4%), hemorrhage in five cases (4.2%), skin laceration in two cases (1.7%), nerve palsy in two cases (1.7%), contusion in one case (0.8%), and organ injury in one case (0.8%).
- The identified missed injury area was classified based on the Abbreviated Injury Scale 2015 dictionary [8]. However, pelvic injuries were further analyzed in this study because they affect mortality as many as lower-extremity injuries [9]. As the results show, there were 34 cases (28.6%) of injury in the upper extremities, 27 cases (22.7%) in the chest, 26 cases (21.8%) in the lower extremities, 13 cases (10.9%) in the facial region, eight cases (6.7%) in the head, seven cases (5.9%) in the abdomen, and four cases (3.4%) in the pelvis.
- Regarding the diagnostic tools used to detect the missed injuries, 53 cases of injury (44.5%) were diagnosed by computed tomography (CT), 23 cases (19.3%) each were diagnosed by magnetic resonance imaging and X-ray. Fourteen cases (11.8) were confirmed through bone scan and six cases (5.0%) were confirmed through physical examination alone.
RESULTS
- In this study, patients with ISS ≥16 accounted for 27.5% of patients in non-MIG, and the proportion of MIG was considerably higher at 71.2%. The mean ISS was 11.76±8.84 in non-MIG, whereas it was 22.03±11.76 in MIG, which was 10.27 higher than that of non-MIG. This result suggests that because injury control and resuscitation management are prioritized, and such cases are immediate transferred to the operating room or radiological intervention room, it is difficult to detect all injuries during the initial management. Furthermore, the ability to conduct a thorough TTS is limited on account of the patients being administered opioids and sedatives or having an altered mental state due to brain injury or shock. Therefore, to detect missed injuries, medical staff at trauma centers should repeatedly evaluate physical examination and review radiologic images during the patient’s hospitalization.
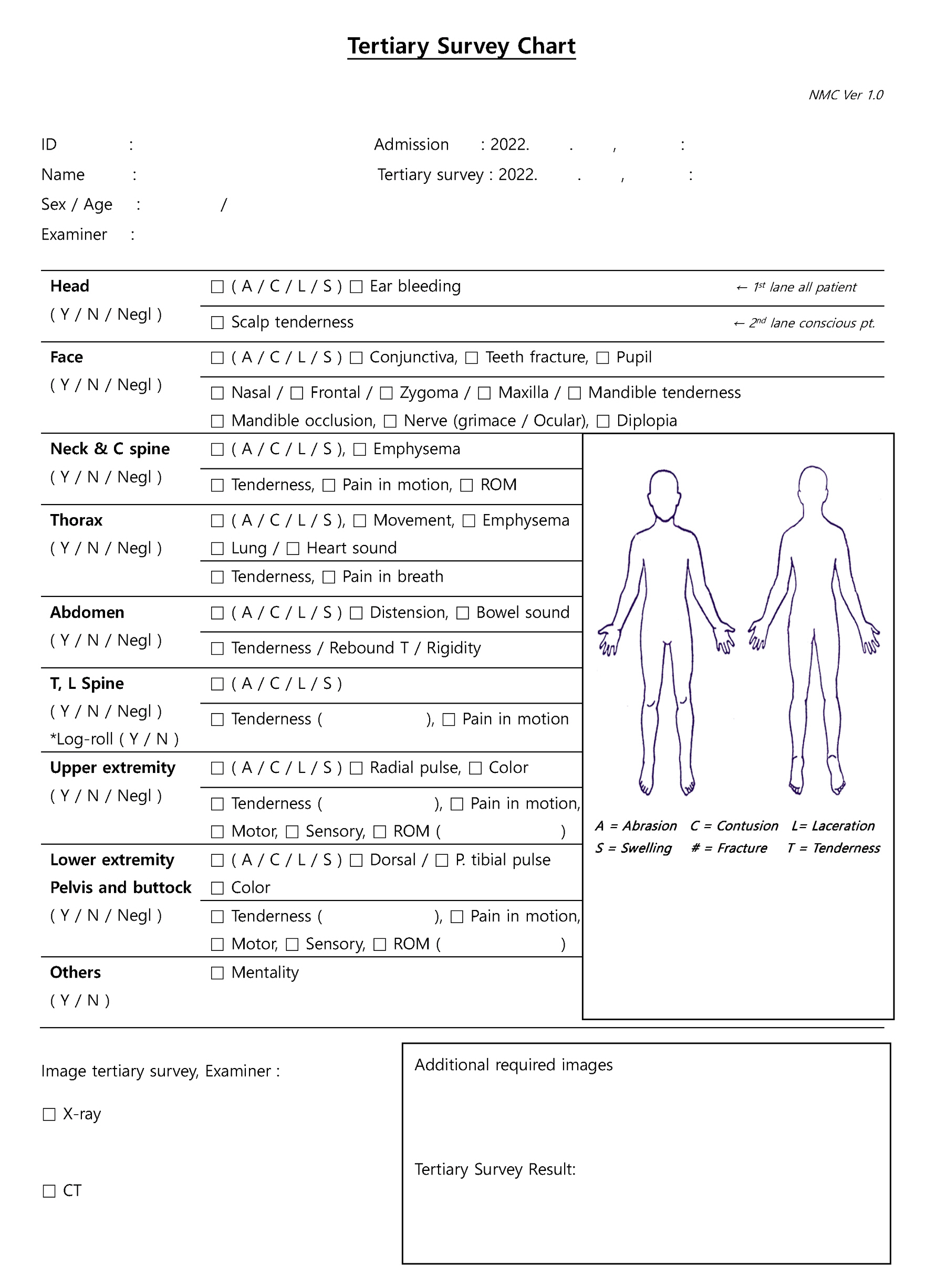
- In addition, a standardized tertiary investigation tool will enable rapid identification of missed injuries and improve prognosis [10,11]. Thus, we recently developed a protocol for TTS with a survey chart and designated the person in charge to systematically detect missed injuries. The chart was configured in a two-way investigation, depending on the patient’s level of consciousness. If the patient is unconscious due to sedatives, shock, or brain injury, TTS is conducted only by limited examinations, such as inspection (e.g., for abrasion, contusion, laceration, swelling, fracture, tenderness, skin color, and chest movement), auscultation (e.g., heart, lung, and bowl sounds), palpation (e.g., pulse, emphysema), and percussion located in the first lane in the chart with review of radiography. After the patient’s consciousness is recovered, TTS is completed by assessing complaints of pain or response to physical examinations in the second lane (Fig. 2).
- The types of missed injuries identified in this study were type I (23.5%), type II (75.6%), and type III (0.8%), showing trends similar to those in the previous study (23%, 59%, and 0.1 %, respectively) [12]. Although it has not been long since the domestic severe trauma treatment system was established, it is remarkable that it is in line with previous studies conducted overseas. Perhaps, it is because patients are intensively evaluated in early hospital days at resuscitation stage or missed injuries are found in the process of reestablishing the treatment plan in the 1st week when the patient’s vital sign is stabilizing. However, further research is needed to clarify the trend that found missed injuries in 1 to 4 days of hospitalization and peaked at 8 to 14 days.
- The injuries most frequently identified were fractures (82.4%) and ligament tears (8.4%), requiring consultation with the orthopedic department. Moreover, the injured areas comprised the upper extremities (28.6%), chest (22.7%), and lower extremities (21.8%). In most patients with severe trauma, opioids and sedatives are often administered for pain control and ventilator care after management such as surgical treatment and initial resuscitation [13]. Therefore, it could be difficult for the patient to clearly identify pain in the injured area. Accordingly, injuries that cannot be identified based on appearance, such as dislocations and open wounds, are thought to be recognized in the process of performing physical and radiologic examination once the patient’s vital signs are stabilized.
- Regarding the tools that finally diagnosed the missed injuries, 53 cases (44.5%) by CT, 23 cases (19.3%) each by magnetic resonance imaging and X-ray, 14 cases (11.8%) by bone scanning, and six cases (5.0%) by physical examination. In many cases, it is difficult to identify the exact mechanism of injury because patients with severe trauma have unstable vital signs and are unconscious or confused. Therefore, to shorten the time spent in the CT and emergency rooms, we conducted a protocol that included a noncontrast scan of the brain and neck and a contrast-enhanced scan of the chest, abdomen, and pelvis, unless there were limitations such as hemodynamic instability. Through this process, major trauma areas were identified and treated by surgery or radiological intervention. It is believed that missed injuries were confirmed when CT or X-ray studies were reviewed by the medical staff within 24 hours [7,14,15].
- A bone scan visualizes the activity of osteoblasts. If there are complaints of pain and traces of trauma, a bone scan can be used to evaluate the suspected area for a fracture. Therefore, unless there was a limitation, we performed a bone scan 5 days after admission or immediately after transfer to the general ward. In this study, 14 patients (11.8%) were diagnosed using bone scans. This is consistent with the claim that bone scanning is effective in diagnosing fractures that were missed during the initial resuscitation process [16].
- However, in this study, two cases of facial nerve palsy were confirmed only by physical examination alone. It is necessary to conduct physical examination and early examination of the neurological system when nerve damage is suspected to avoid sequelae in the recovery process.
- This study has several limitations. First, it was performed at a single trauma center and the number of cases was small. Second, the study is retrospective in nature, and data confirmation, such as the patient’s initial level of consciousness or administration of sedatives, was limited. Therefore, the scope of the study was limited, and the results cannot be generalized. Nevertheless, we suggest additional research to overcome the difficulty of performing TTS and improve patient’s prognosis, including patient’s data like amount or duration of administered sedatives and length of ventilator care.
- In conclusion, TTS is considered a useful process for identifying areas of injury that were missed at the time of initial resuscitation [7]. But the ability to conduct a thorough TTS is limited on account of the status of patients or the environment of each trauma center. Therefore, it is necessary to develop a suitable program for each trauma center that protocolized the TTS and a chart to assist in documenting insufficient parts of performing TTS. Further investigation is needed to verify the effectiveness of the protocolized TTS and chart through multi-institutional joint research to investigate the diagnostic method, type of missed injury, and treatment method.
DISCUSSION
-
Ethical statements
This study was approved by the Institutional Review Board of the National Medical Center (No. NMC-2021-10-122). The written informed consent was waived due to the retrospective nature of this study.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: SHY; Data curation: all authors; Formal analysis: EGJ; Methodology: EGJ, YK, SHY; Project administration: SHY; Resources: SYB, SSH, YK, SHY; Visualization: EGJ; Writing–original draft: EGJ; Writing–review & editing: all authors.
All authors read and approved the final manuscript.
ARTICLE INFORMATION
| Characteristic | Non-MIG (n=734) | MIG (n=73) | t | P-value* |
|---|---|---|---|---|
| Age (yr) | - | - | ||
| Range (min–max) | 20–112 | 21–86 | ||
| Mean±SD | 62.9±18.1 | 50.7±17.1 | ||
| Hospital day | ||||
| Range (min–max) | 1–228 | 2–205 | - | - |
| Median (IQR) | 18 (8.0–31.0) | 39 (21.5–72.5) | - | - |
| Mean±SD | 24.74±26.11 | 50.90±39.56 | 3.200 | 0.002 |
| Injury Severity Score | ||||
| Range (min–max) | 1–75 | 1–48 | - | - |
| Mean±SD | 11.76±8.84 | 22.03±11.76 | 7.271 | <0.001 |
| ≥16a) | 202 (27.5) | 52 (71.2) | 5.143 | <0.001 |
| Sex | - | - | ||
| Male | 475 (64.7) | 57 (78.1) | ||
| Female | 259 (35.3) | 16 (21.9) |
| Characteristic | No. (%) |
|---|---|
| Missed injury type | |
| I (within 24 hr) | 28 (23.5) |
| II (after 24 hr) | 90 (75.6) |
| III (after discharge) | 1 (0.8) |
| Detected time (day of hospitalization) | |
| 1 | 12 (10.1) |
| 2 | 18 (15.1) |
| 3 | 15 (12.6) |
| 4 | 12 (10.1) |
| 5 | 5 (4.2) |
| 6 | 4 (3.4) |
| 7 | 5 (4.2) |
| 8–14 | 22 (18.5) |
| 15–28 | 8 (6.7) |
| 29–42 | 12 (10.1) |
| 43–77 | 6 (5.0) |
| Injury type | |
| Fracture | 98 (82.4) |
| Ligament tear | 10 (8.4) |
| Hemorrhage | 5 (4.2) |
| Skin laceration | 2 (1.7) |
| Palsy | 2 (1.7) |
| Contusion | 1 (0.8) |
| Organ injury | 1 (0.8) |
| Injury area | |
| Head and necka) | 8 (6.7) |
| Face | 13 (10.9) |
| Thoraxb) | 27 (22.7) |
| Abdomenc) | 7 (5.9) |
| Pelvisd) | 4 (3.4) |
| Upper extremity | 34 (28.6) |
| Lower extremity | 26 (21.8) |
| Detector | |
| Computed tomography | 53 (44.5) |
| Magnetic resonance imaging | 23 (19.3) |
| X-ray | 23 (19.3) |
| Bone scan | 14 (11.8) |
| Physical examination | 6 (5.0) |
- 1. Statistics Korea. Statistical yearbook of causes of death in 2020 [Internet]. Daejeon: Statistics Korea; 2021 [cited 2021 Oct 18]. Available from: https://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board?bmode=read&bSeq=&aSeq=403046.
- 2. Ha JW, Han GT, Kim DW, Im HS, Choi JG, Yuk TM. A study on the burden of medical expenses for patients with severe trauma (report no. 2017-20-033). Goyang: National Health Insurance Service Ilsan Hospital; 2017.
- 3. Yu BC, Chung M, Lee GJ, et al. Analysis of KTDB registered trauma patients from a single trauma center in Korea. J Trauma Inj 2015;28:123–8. Article
- 4. Jo JY, Hwang YS, Kweon SH. A community-based study of severe trauma, death and disability, 2019. Cheongju: Korea Disease Control and Prevention Agency; 2021.
- 5. Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med Cent) 2010;23:349–54. ArticlePubMedPMC
- 6. Ministry of Health and Welfare. Assessment of preventable trauma mortality rate and activation of trauma center operation. Sejong: Ministry of Health and Welfare; 2017.
- 7. Zamboni C, Yonamine AM, Faria CE, Filho MA, Christian RW, Mercadante MT. Tertiary survey in trauma patients: avoiding neglected injuries. Injury 2014;45 Suppl 5:S14–7. ArticlePubMed
- 8. Association for the Advancement of Automotive Medicine (AAAM). Abbreviated Injury Scale 2015 released. Chicago: AAAM; 2016
- 9. Sathy AK, Starr AJ, Smith WR, et al. The effect of pelvic fracture on mortality after trauma: an analysis of 63,000 trauma patients. J Bone Joint Surg Am 2009;91:2803–10. ArticlePubMed
- 10. Houshian S, Larsen MS, Holm C. Missed injuries in a level I trauma center. J Trauma 2002;52:715–9. ArticlePubMed
- 11. Pfeifer R, Pape HC. Missed injuries in trauma patients: a literature review. Patient Saf Surg 2008;2:20. ArticlePubMedPMCPDF
- 12. Tammelin E, Handolin L, Soderlund T. Missed injuries in polytrauma patients after trauma tertiary survey in trauma intensive care unit. Scand J Surg 2016;105:241–7. ArticlePubMedPDF
- 13. Joseph A. Sedation of the trauma patient in the intensive care unit. J Emerg Crit Care Med 2018;2:8. Article
- 14. Thomson CB, Greaves I. Missed injury and the tertiary trauma survey. Injury 2008;39:107–14. ArticlePubMed
- 15. Gordic S, Alkadhi H, Hodel S, et al. Whole-body CT-based imaging algorithm for multiple trauma patients: radiation dose and time to diagnosis. Br J Radiol 2015;88:20140616. ArticlePubMedPMC
- 16. Lee KJ, Jung K, Kim J, Kwon J. Bone scan as a screening test for missed fractures in severely injured patients. Orthop Traumatol Surg Res 2014;100:953–7. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Tertiary Trauma Survey on Emergency Department Observational Units: A Systematic Literature Review
Tamkeen Pervez, Mehreen Malik
Cureus.2024;[Epub] CrossRef
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite



