Experience with the emergency vascular repair of upper limb arterial transection with concurrent acute compartment syndrome: two case reports
Article information
Abstract
Upper extremity vascular injuries occurring with acute compartment syndrome are very challenging to manage in an emergency context in resource-poor settings. The need to always recognize the likelihood of coexisting compartment syndrome guides surgeons to perform concomitant fasciotomy to ensure a better outcome. We managed three vascular injuries in the upper extremities in two patients with concomitant imminent compartment syndrome observed intraoperatively. The first injury was complete brachial artery disruption following blunt trauma, while the second and third injuries were radial and ulnar artery transection caused by sharp glass cuts. Both patients were treated with vascular repair and fasciotomy. Secondary wound coverage was applied with split-thickness skin grafting, and the outcomes were satisfactory. Concomitant fasciotomy potentially improves the outcomes of vascular repair in emergency vascular surgery and should be considered for all injuries with the potential for acute compartment syndrome.
INTRODUCTION
Injuries to the extremities are a common component of trauma resulting from road traffic accidents. These injuries may occur in isolation or as part of polytrauma. The extent of injury varies depending on the energy of trauma. Injuries involving neurovascular bundles are also very common; these usually occur in high-energy events, and could readily be missed in cases of low-energy blunt injuries [1]. Penetrating injuries are a commoner cause of neurovascular injuries than blunt trauma [2]. Upper extremity vascular trauma constitutes nearly half of all peripheral vascular injuries [3]. It is a limb-threatening and/or a life-threatening event that requires prompt surgical attention. The need for a timely intervention to prevent limb loss is the major responsibility of the trauma and vascular team.
The occurrence of major vascular injury with acute compartment syndrome could be very challenging both to evaluate and treat. The features of acute compartment syndrome could mimic those of vascular injuries, which could also lead to the former [4]. In a setting where the etiopathogenesis of acute compartment syndrome involves both a vascular injury with bleeding into the compartment and direct muscle contusion, the onset of signs common to both conditions is rapid, as well as their progression. The common signs are disproportionate pain, paresthesia, palsy, the absence of a distal pulse, and cold extremities [4].
Acute compartment syndrome occurs very commonly in the forearm, although it is less common than in the leg [5]. The commonest cause is trauma with contusion of the muscles and vascular injury. Prompt presentation and treatment are necessary to ensure limb salvage and prevent or reduce the severity of reperfusion injury. The challenges of late presentation and the unavailability of essential instruments for vascular surgery often affect the outcomes of vascular injuries in rural areas in tropical regions [3]. This leads to unfavorable outcomes, especially limb losses.
CASE REPORTS
The two patients analyzed in this study were managed about a month apart at the Alex Ekwueme Federal Teaching Hospital Abakaliki. The first was a 19-year-old male patient who presented to the unit about 11 hours following a crush injury of the left upper limb. He was behind a reversing sports utility vehicle that collided with him, pressing his upper limb against a wall. The features of acute compartment syndrome were demonstrated preoperatively, and a neurovascular injury was suspected. There was significant bleeding, and the patient presented with a hematocrit of 29%. He was then resuscitated and transfused with 2 units of blood.
The intraoperative findings were avulsion of the roof of the cubital fossa and the bicipital aponeurosis, complete disruption of the brachial artery and its venae comitantes just above the cubital fossa, sparing of the cephalic vein, intact median and ulnar nerves, and acute compartment tension in the anterior compartment of the forearm, which showed grayish and severely contused muscles. The procedure was performed under general endotracheal anesthesia using a tourniquet applied to the proximal third of the arm, observing strict asepsis. The wound was explored and copiously irrigated with dilute hydrogen peroxide and normal saline.
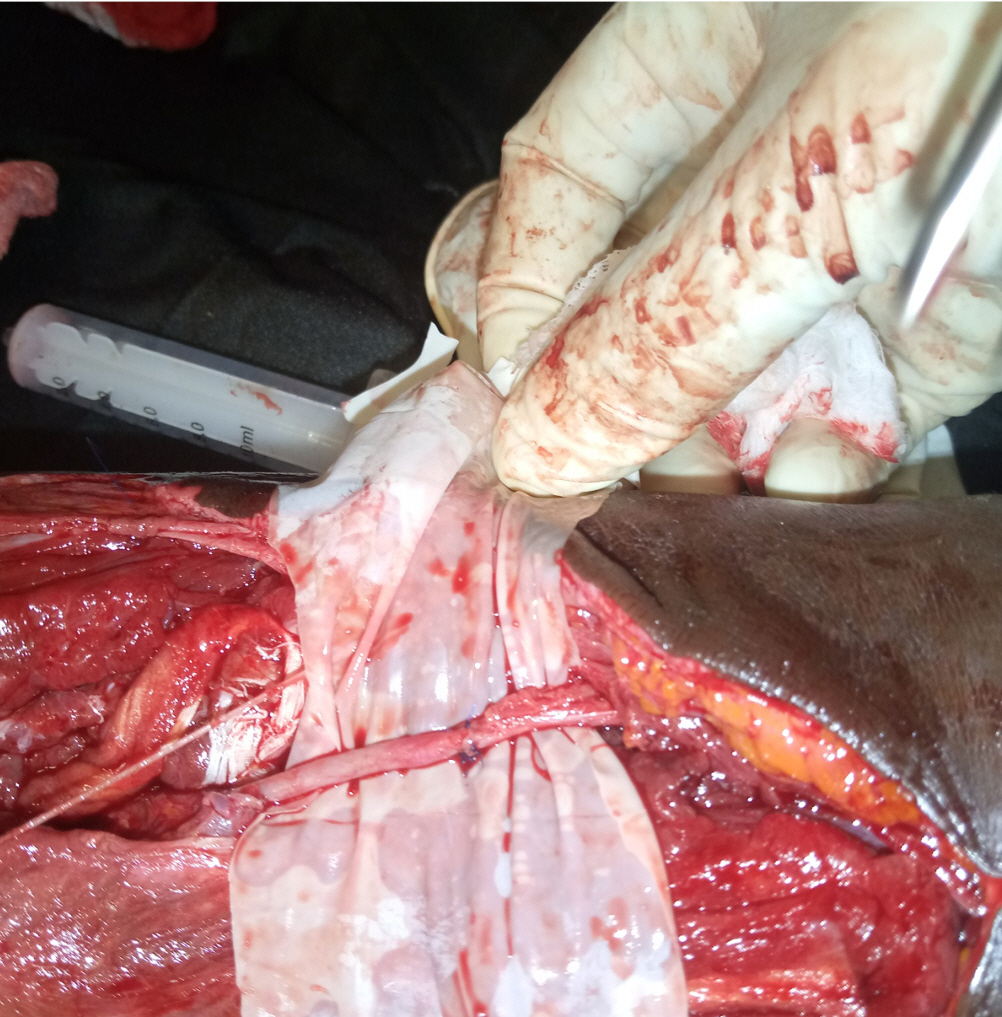
Fasciotomy was performed, the brachial artery was cannulated with a 5F feeding tube, and irrigation with unfractionated heparin was performed. Approximation of the two ends of the brachial artery was achieved with Prolene 5/0, while dilute heparin irrigation and washout continued (Fig. 1). Sutures were applied at eight points and tied gradually upon removal of the feeding tube. Evidence of perfusion was demonstrated with the return of distal pulses, restoration of redness of the muscles, and recovery of normal temperature and partial oxygen pressure between 96% and 100% in the ensuing 24 hours. The wound was loosely dressed, covered with a crepe bandage, and immobilized with a plaster of Paris back slab at 15° flexion. Low-molecular-weight heparin (enoxaparin) was given subcutaneously at 40 mg daily for 1 week before converting to dabigatran tablets (110 mg daily). Presumptive antibiotics, analgesics, and vitamins A, C, and E were continued in the postoperative period. Alternate-day wound dressings were commenced 48 hours after surgery and converted to daily dressings 5 days prior to split-thickness skin grafting. The postoperative period was uneventful, and wound cover was subsequently achieved with split-thickness skin grafting. Healing was complete, and physiotherapy was employed for elbow rehabilitation. The range of movement of the elbow joint was normal on discharge. The donor-site healing of the split-thickness skin graft was excellent. The patient was lost to outpatient follow-up.
The second patient was a 23-year-old male patient, a right-handed truck driver who sustained a glass cut on the midpoint of the right forearm following a motor vehicle crash. He sustained complete transection of both the ulnar and radial arteries at the mid-forearm (Fig. 2). He bled profusely, presented with a hematocrit of 18%, and only provided 2 units of whole blood 12 hours after the injury. This necessitated conducting the operation with a tourniquet to save the limb. The intraoperative findings confirmed complete disruption of the arteries, sparing of the ulnar and median nerves, transection of the muscles of the forearm, and evidence of compartment syndrome. Wound lavage was done with dilute hydrogen peroxide and normal saline. The vessels were cannulated with a size 6 feeding tube and washout was performed with unfractionated heparin (Fig. 3). Vascular coaptation was achieved with Prolene 6/0. Fasciotomy was performed, and the transected muscles were repaired with Vicryl 0 sutures. The wound was loosely dressed with an antibiotic-impregnated petrolatum gel gauze as the contact layer and a gauze absorptive layer was formed by coverage with a crepe bandage. The postoperative management was as in the first case. The outcome was equally gratifying to both the patient and the managing team. Both procedures were performed by the same surgeon. Both patients also gave consent for clinical photographs and the publication thereof.
DISCUSSION
Vascular injuries are often challenging, both to the patient and the managing team, in the tropics due to the lack of both expertise and institutional support in a resource-constrained environment. Patients are often forced to undergo amputation of the extremities. This unfavorable outcome also discourages patients from presenting at tertiary institutions for fear of losing their limbs. The two patients presented herein, in whom three vascular disruptions were managed, were young men and so it was very necessary to salvage the extremities despite all the institutional limitations in the resource-poor setting [6].
Another major challenge is the lack of insurance coverage for most patients in resource-poor settings; coupled with poverty, this reduces the likelihood of patients receiving treatment at the right time [7,8]. As patients apart from government employees pay essentially out of pocket, it takes time to mobilize resources for hospital bills. Furthermore, even with an early presentation, there are certain obligations (e.g., procuring blood) that patients must meet themselves before the procedure is carried out. Both patients in this study bled significantly and needed to be transfused prior to surgery.
Vascular repair was done following the established principles of asepsis and surgical techniques. The coexistence of acute compartment syndrome caused by bleeding into the compartment and/or contusion of the muscles necessitated fasciotomy in all cases, as the ensuing edema could constitute a major obstacle to the success of vascular repair. After fasciotomy, there was evidence of recovery of the muscles intraoperatively. In our setting, where postoperative monitoring is limited to oxygen saturation through pulse oximetry, it is most crucial that every possible mechanical impediment to the flow of blood through the point of coaptation be removed. The wounds were closed secondarily with split-thickness skin grafting. Wound coverage with a split-thickness skin graft was a minor procedure performed after the vascular repair was confirmed to be successful.
The outcome in both patients was excellent at both the donor and the recipient sites, and the patients were discharged within 2 weeks of skin grafting. No significant complications relating to either the vascular repair or the split-thickness skin graft were observed. Both patients were followed up on an outpatient basis. The first patient had an uneventful recovery of function and did not need professional physiotherapy. He regained grossly complete function and continued his educational program. The second patient briefly received physiotherapy to improve power at the wrist joint. He had full recovery of function and returned to his job as a truck driver.
Concurrent fasciotomy with vascular repair in traumatic vascular disruption is an important adjunct to vascular coaptation [9]. Although it requires another session in the operating theater to achieve wound coverage, it is far more rewarding than a single session with attendant failure. Nonetheless, conducting a study with a larger sample would yield more convincing evidence regarding the role of concurrent fasciotomy.
Vascular trauma repair is yet undeveloped in the West African subregion and there are limited publications to that effect. The reason for this is mainly due to poor outcomes, which discourage surgeons in this subregion from embarking on such procedures. Onakpoya et al. [10] recorded a salvage rate of 64.9% and an amputation rate of 25%. However, they did not indicate performing any type of fasciotomy despite its obvious advantages [9,10]. Another published work showed a salvage rate of 80% at a National Cardiothoracic Center of Excellence, but still without any mention of fasciotomy [11]. It is therefore hoped that by sharing this experience, we will motivate surgeons in the West African subregion to use their limited resources to perform limb vascular repair with fasciotomy where indicated, and thereby salvage as many extremities as possible.
In conclusion, emergency vascular repair in the extremities following trauma may have greater success if acute compartment syndrome is addressed and the wound is closed secondarily. It is therefore imperative in every upper extremity neurovascular injury to identify a present or potential acute compartment syndrome before, during, or immediately after neurovascular repair in order to take necessary action for an optimal outcome.
Notes
Ethical statements
Informed consents for publication of the research details and clinical images were obtained from the patients.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: all authors; Methodology: all authors; Project administration: CCM; Writing–original draft: all authors; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Acknowledgements
The authors appreciate the assistance of the ward nurses in the postoperative management of the patients.