Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Original Article
Epidemiology and outcomes of patients with penetrating trauma in Incheon Metropolitan City, Korea based on National Emergency Department Information System data: a retrsopective cohort study -
Youngmin Kim, MD1
 , Byungchul Yu, MD1,2
, Byungchul Yu, MD1,2 , Se-Beom Jeon, MD1
, Se-Beom Jeon, MD1 , Seung Hwan Lee, MD1
, Seung Hwan Lee, MD1 , Jayun Cho, MD1
, Jayun Cho, MD1 , Jihun Gwak, MD1
, Jihun Gwak, MD1 , Youngeun Park, MD1
, Youngeun Park, MD1 , Kang Kook Choi, MD1,2
, Kang Kook Choi, MD1,2 , Min A Lee, MD1,2
, Min A Lee, MD1,2 , Gil Jae Lee, MD1,2
, Gil Jae Lee, MD1,2 , Jungnam Lee, MD1,2
, Jungnam Lee, MD1,2
-
Journal of Trauma and Injury 2023;36(3):224-230.
DOI: https://doi.org/10.20408/jti.2022.0055
Published online: December 21, 2022
- 1,575 Views
- 47 Download
1Department of Trauma Surgery, Gachon University Gil Medical Center, Incheon, Korea
2Department of Traumatology, Gachon University College of Medicine, Incheon, Korea
- Correspondence to Byungchul Yu, MD Department of Traumatology, Gachon University College of Medicine, 21 Namdong-daero 774beon-gil, Namdong-gu, Incheon 21565, Korea Tel: +82-32-460-3010 E-mail: kane2123@gilhospital.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Patients with penetrating injuries are at a high risk of mortality, and many of them require emergency surgery. Proper triage and transfer of the patient to the emergency department (ED), where immediate definitive treatment is available, is key to improving survival. This study aimed to evaluate the epidemiology and outcomes of patients with penetrating torso injuries in Incheon Metropolitan City.
-
Methods
- Data from trauma patients between 2014 and 2018 (5 years) were extracted from the National Emergency Department Information System. In this study, patients with penetrating injuries to the torso (chest and abdomen) were selected, while those with superficial injuries were excluded.
-
Results
- Of 66,285 patients with penetrating trauma, 752 with injuries to the torso were enrolled in this study. In the study population, 345 patients (45.9%) were admitted to the ward or intensive care unit (ICU), 20 (2.7%) were transferred to other hospitals, and 10 (1.3%) died in the ED. Among the admitted patients, 173 (50.1%) underwent nonoperative management and 172 (49.9%) underwent operative management. There were no deaths in the nonoperative management group, but 10 patients (5.8%) died after operative management. The transferred patients showed a significantly longer time from injury to ED arrival, percentage of ICU admissions, and mortality. There were also significant differences in the percentage of operative management, ICU admissions, ED stay time, and mortality between hospitals.
-
Conclusions
- Proper triage guidelines need to be implemented so that patients with torso penetrating trauma in Incheon can be transferred directly to the regional trauma center for definitive treatment.
- Background
- Trauma is the most common cause of death among young people in Korea, and the preventable death rate ranges from 32.6% to 50.4% [1–3]. Therefore, the Korean government and medical societies agreed to develop a trauma system, including the establishment of regional trauma centers (RTCs) in 2012. In 2014, the first RTC opened, with plans to establish 17 RTCs in Korea by 2021. However, several aspects of the regional trauma system, including governance, low-level trauma centers, and authorized guidelines for injured patient care, have yet to be established.
- The management of penetrating torso injuries is challenging because it requires rapid and accurate assessment and surgical intervention. The rapid prehospital transportation of patients with penetrating injuries to the appropriate facility (i.e., a trauma center) is crucial [4,5]. Rapid transportation and management by experienced trauma surgeons at trauma centers have been shown to improve the survival of patients with major penetrating injuries [6,7]. A study also showed that patients from rural areas had a higher prehospital mortality risk than those from urban areas [8]. Worse outcomes were related to the response time, distance of transport, and limitations in specialized care in rural areas.
- Objectives
- This study aimed to describe the demographics and outcomes of patients with penetrating torso injuries in Incheon Metropolitan City after 2014, when the first RTC opened in Incheon.
INTRODUCTION
- Ethics statement
- This study was approved by the Institutional Review Board of Gachon University Gil Medical Center (No. GCIRB2020-375). The requirement for informed consent from patients was waived due to the retrospective nature of the study.
- Study design and setting
- This retrospective cohort study used data obtained from the National Emergency Department Information System (NEDIS), which is a database operated by the Ministry of Health and Welfare that collects data from all patients visiting 434 emergency departments (EDs) in Korea. The data included patients’ demographics, clinical characteristics, and diagnosis codes at admission. This study did not receive any funding from external sources.
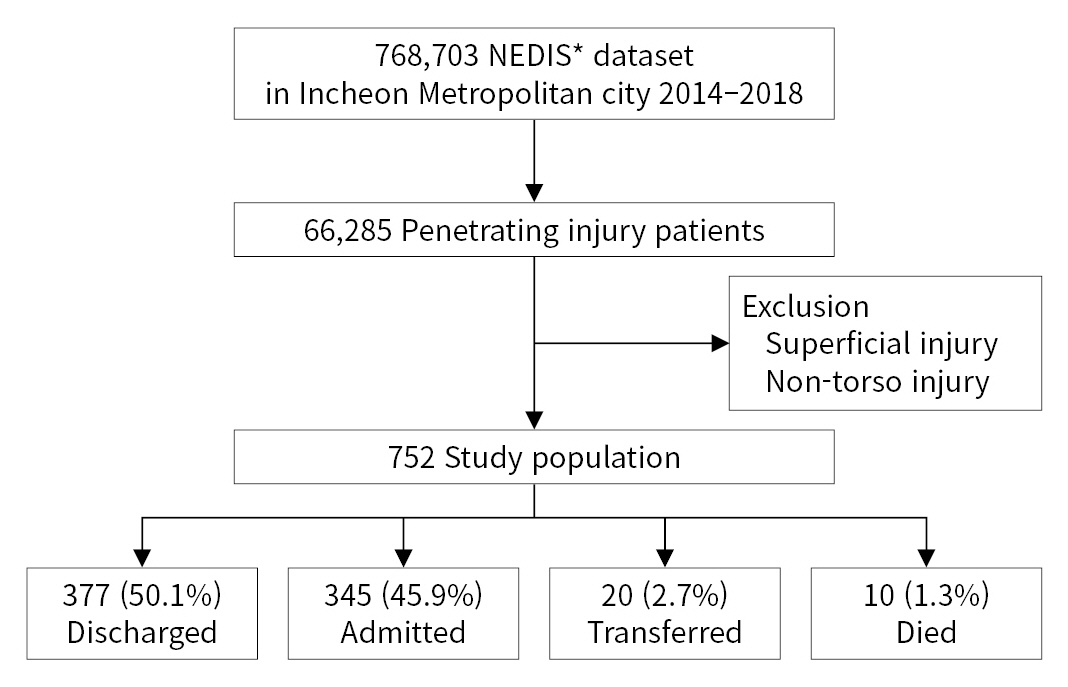
- We extracted the data of all trauma patients who visited EDs in Incheon Metropolitan City from NEDIS between January 2014 and December 2018. Patients with trauma were identified using International Classification of Diseases (ICD) codes. Superficial injuries, drowning, or intoxication cases were not included in the dataset. In this study, we included patients with penetrating injuries to the torso (chest and abdomen) based on ICD codes (Fig. 1).
- Population and trauma care system of Incheon Metropolitan City
- Three million people live in Incheon Metropolitan City, which is surrounded by Seoul and Gyeonggi Province. This region has a population of approximately 20 million. There is one hospital—hereinafter referred to hospital B—in Incheon that has both a regional emergency center (REC) and an RTC. In addition, one REC without an RTC, nine local emergency centers (LECs), and nine local emergency institutions exist in the city. Before the RTC opened in 2014, trauma patients were triaged based on the shortest transport time and distance, such that severely injured patients could be brought to the nearest REC or LEC. After the RTC opened, the standard guidelines for 119 (i.e., emergency) paramedics recommended that severely injured patients be transported to the RTC or an REC; however, this has not been well orchestrated by the trauma governance system.
- Statistical analysis
- The basic demographic variables, types of ED, mechanism of injury, ED presentation route, and other clinical information were analyzed. Age was categorized into the following groups: 0–19, 20–29, 30–39, 40–49, 50–59, 60–69, and ≥70 years. The presentation routes were categorized as either direct or transferred. Medical information included vital signs, mental status at the time of ED arrival, patient’s disposition after ED management, diagnosis on admission, and outcome at the time of discharge. The time variables included estimated injury time, ED arrival time, and discharge time from the ED or admission. Using the time variables, we calculated the time from injury to ED arrival, the ED stay time, and the time from injury to ED disposition.
- All data were analyzed using IBM SPSS ver. 22 (IBM Corp., Armonk, NY, USA). Numerical data are presented as mean±standard deviation or median (interquartile range), and categorical data are presented as percentages. The chi-square test was used to compare proportions for categorical variables, and the Student t-test or Mann-Whitney U-test was used to compare means or medians for continuous variables, as appropriate. Statistical significance was defined as P<0.05.
METHODS
- Of the 768,703 trauma patients who visited EDs in Incheon during the 5-year study period, 752 patients with penetrating torso injuries were included in this study (Fig. 1). Among them, 377 (50.1%) were discharged from the ED, 345 (45.9%) were admitted, 20 (2.7%) were transferred to another hospital, and 10 (1.3%) died in the ED. The most common age group was 40 to 49 years (22.5% of total patients, 24.3% of admitted patients), and more than 70% of the patients were male (Table 1). Approximately half of the patients (42.7%) were transported to RECs, and 90% of patients presented directly to the ED. The admission group showed a significantly lower percentage of patients who presented directly to the ED and had higher Korean Triage and Acuity Scale (KTAS) scores than the nonadmission group. The ED stay time was significantly longer in the admission group.
- We compared the clinical characteristics between patients who received nonoperative management (NOM) and operative management (OM) (Table 2). More patients in the OM group than in the NOM group were managed in RECs (62.8% vs. 44.5%, P=0.001). The OM group showed significantly lower systolic blood pressure and a higher rate of admission to the intensive care unit (ICU). None of the patients died after NOM, whereas 10 patients (5.8%) who received OM died. The transferred patients showed a significantly longer time from injury to ED (43 minutes vs. 101 minutes), higher ICU admission rate (21.3% vs. 43.7%), and higher mortality (2.2% vs. 7.7%) (Table 3).
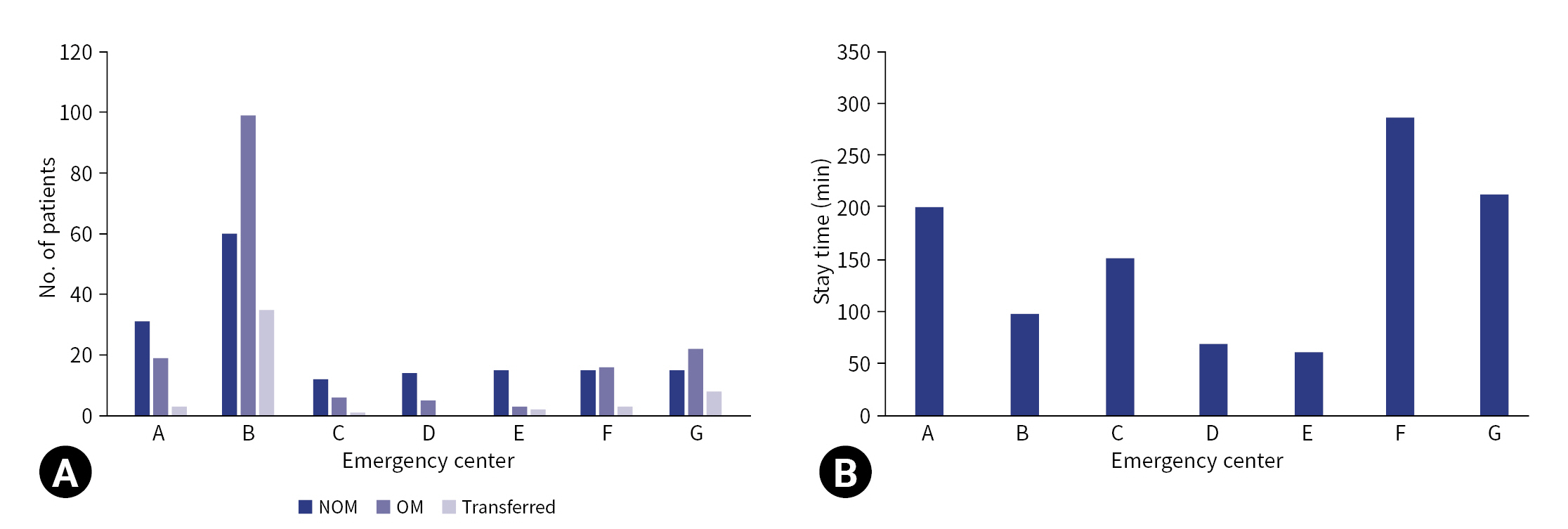
- The number of patients admitted was significantly different among EDs in Incheon (Table 4). Hospital B (both the RTC and REC) had the highest patient volume, managing 46.1% of the total patients and 58.2% of the OM patients. The ICU admission rates varied from 15.8% to 71.7% among hospitals, and hospital B had the largest number of patients admitted to the ICU during the 5-year study period. The shortest ED stay for all admitted patients was 61 minutes, and the longest stay was 286 minutes. In addition, there was a significant variation in the ED stay time of patients who were directly transferred to the operating room (from 48 minutes to 157.5 minutes) (Fig. 2).
RESULTS
- In this study, penetrating torso injuries accounted for 1.1% and 0.1% of all penetrating injuries and all injuries, respectively. Although a direct comparison is difficult due to differences in the clinical characteristics of the study population, this study showed a relatively low incidence of penetrating torso injuries in Incheon over the last 5 years, similar to other industrialized countries [9–11]. Moreover, the incidence and mortality rates of penetrating torso injuries requiring hospitalization were relatively low [12–14]. Unlike in the United States and South Africa, firearms are prohibited in Korea, which may, in part, contribute to the low incidence of penetrating injuries [15,16].
- Most patients were directly transported to the ED for treatment, and the median time from injury to ED arrival was 48 minutes. However, 8.6% of the patients did not receive definitive management in the ED where they initially arrived. Moreover, patients who required hospitalization had a lower rate of direct transportation and longer stays in the ED. This is supported by the opinion that the roles of the RTC and other emergency medical centers are not clearly distinguished, meaning the emergency triage system is not efficient at the prehospital level in Korea [17]. As a result, patients with severe trauma were not concentrated in the RTC.
- The transferred patients had a longer time from injury to the final ED arrival than the other patients. Furthermore, they showed a higher rate of ICU admission and mortality, suggesting that a delayed arrival to the final ED due to transfer could be a risk factor for poor outcomes. Therefore, we need to focus on these transferred cases to improve the outcomes after penetrating injuries.
- Fu et al. [7] reported that trauma centers with a high volume of penetrating trauma patients were associated with good outcomes. In Incheon, only hospital B has an RTC in addition to an REC. This hospital has managed a substantial number of patients in the last 5 years. Our findings showed that the rates of OM and ICU admission were higher in hospital B than in the other REC. Despite this, the ED stay time in hospital B was shorter than that in other hospitals. Of note, patients who were directly transferred to the operating room had a significantly shorter stay in the emergency room in hospital B than in other hospitals. Hoyt et al. [18] reported that direct transport to the operating room for resuscitation was associated with better outcomes in patients with penetrating torso injuries. Meizoso et al. [19] argued that protocols to shorten the ED stay for patients requiring surgery are essential. To improve the clinical outcomes of penetrating torso injuries, it is necessary to establish a trauma governance system that allows direct transfer to the RTC for definitive treatment.
- Limitations
- This study had some limitations. First, as with other retrospective studies with large databases, this study has the potential for selection bias. Second, the NEDIS data lack granular clinical information, such as hemodynamic changes and transfusion requirements. Third, a comparative analysis of data from other regions with similar characteristics would have made it possible to better understand the characteristics of patients with penetrating injuries in Incheon. Despite these limitations, this study is the first to analyze specific injury mechanisms in the metropolitan area of Korea and will be helpful in establishing trauma governance in Incheon.
- Conclusions
- The number of patients with penetrating torso injuries in Incheon Metropolitan City was small enough to be managed at a single definitive treatment facility. Transferring patients to other hospitals is associated with delayed arrival to the final ED, which can cause poor outcomes. To address these factors, appropriate triage guidelines are needed to allow direct transfer to the RTC for patients with penetrating torso trauma in Incheon.
DISCUSSION
-
Author contributions
Conceptualization: BY, JL; Data curation: SBJ, SHL; Formal analysis: YK, JC, JG, YP, JM; Methodology: KKC, MAL, GJL; Visualization: BY, SBJ, SHL, JL; Writing–original draft: YK, JC, JG, YP, KKC, MAL, GJL; Writing–review & editing: all authors.
All authors read and approved the final manuscript.
-
Conflicts of interest
Gil Jae Lee is the Editor-in-Chief, Min A Lee is the Associate Editor, and Seung Hwan Lee, Jayun Cho, and Kang Kook Choi are Editoial Board members of the Journal of Trauma and Injury, but were not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
-
Funding
The authors did not receive any financial support for this study.
-
Data availability
Data of this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION
Comparison between emergency centers in Incheon.
| Variable | Total (n=752) | Admitted (n=345) | Non-admitted (n=407) | P-value |
|---|---|---|---|---|
| Age (yr) | <0.001a) | |||
| 0–19 | 92 (12.2) | 21 (6.1) | 71 (17.4) | |
| 20–29 | 115 (15.3) | 55 (15.9) | 60 (14.7) | |
| 30–39 | 133 (17.7) | 63 (18.3) | 70 (17.2) | |
| 40–49 | 169 (22.5) | 84 (24.3) | 85 (20.9) | |
| 50–59 | 143 (19.0) | 63 (18.3) | 80 (19.7) | |
| 60–69 | 62 (8.2) | 30 (8.7) | 32 (7.9) | |
| ≥70 | 38 (5.1) | 29 (8.4) | 9 (2.2) | |
| Male sex | 537 (71.4) | 255 (73.9) | 282 (69.3) | 0.162 |
| Classification of emergency center | <0.001a) | |||
| Regional emergency center | 321 (42.7) | 185 (53.6) | 136 (33.4) | |
| Local emergency center | 413 (54.9) | 151 (43.8) | 262 (64.4) | |
| Direct transportation | 687 (91.4) | 293 (84.9) | 394 (96.8) | <0.001a) |
| KTASb)score | <0.001a) | |||
| 1 | 9 (1.2) | 2 (0.6) | 7 (1.7) | |
| 2 | 161 (21.4) | 119 (34.5) | 42 (10.3) | |
| 3 | 104 (13.8) | 59 (17.1) | 45 (11.1) | |
| 4 | 159 (21.1) | 23 (6.7) | 136 (33.4) | |
| 5 | 22 (2.9) | 1 (0.3) | 21 (5.2) | |
| Systolic blood pressure (mmHg) | 118.2±43.8 | 124.7±34.5 | 112.6±49.7 | <0.001a) |
| Pulse rate (beats/min) | 82.2±27.5 | 89.4±22.4 | 76.1±29.9 | 0.020a) |
| Respiratory rate (breaths/min) | 18.7±6.2 | 20.0±4.1 | 17.7±7.4 | <0.001a) |
| ED disposition | NA | NA | NA | |
| Discharge | 377 (50.1) | |||
| Transfer out | 20 (2.7) | |||
| Admission to ward or ICU | 345 (45.9) | |||
| Death in ED | 10 (1.3) | |||
| Time from injury to ED (min) | 48 (30–60) | 54 (30–65) | 39 (27–60) | 0.004a) |
| ED stay time (min) | 79 (36–138) | 108 (68–167) | 52 (24–104) | <0.001a) |
| Time from injury to ED disposition (min) | 143 (85–248) | 175 (120–274) | 115 (65–208) | <0.001a) |
| Variable | NOM group (n=173) | OM group (n=172) | P-value |
|---|---|---|---|
| Classification of emergency center | 0.001a) | ||
| Regional emergency center | 77 (44.5) | 108 (62.8) | |
| Local emergency center | 93 (53.8) | 58 (33.7) | |
| Direct transportation | 145 (83.8) | 148 (86.0) | 0.334 |
| Systolic blood pressure (mmHg) | 129.9±30.0 | 119.5±37.8 | 0.005a) |
| Pulse rate (beats/min) | 87.5±21.4 | 91.3±23.3 | 0.117 |
| Respiratory rate (breaths/min) | 19.6±4.0 | 20.1±4.1 | 0.218 |
| Time from injury to ED (min) | 57 (30–79) | 51 (30–60) | 0.750 |
| ED stay time (min) | 173 (88–199) | 87 (52–143) | 0.440 |
| Time from injury to ED disposition (min) | 211 (140–325) | 150 (98–224) | 0.110 |
| Admission to ICU | 53 (30.6) | 122 (70.9) | <0.001a) |
| Discharged to home | 153 (88.4) | 147 (85.5) | 0.028a) |
| Died in hospital | 0 | 10 (5.8) |
| Variable | Direct (n=687) | Transferred (n=65) | P-value |
|---|---|---|---|
| Classification of emergency center | 0.001a) | ||
| Regional emergency center | 279 (40.6) | 42 (64.6) | |
| Local emergency center | 408 (59.4) | 23 (35.4) | |
| Systolic blood pressure (mmHg) | 117.9±43.9 | 120.9±42.6 | 0.605 |
| Pulse rate (beats/min) | 81.6±27.7 | 88.7±24.5 | 0.300 |
| Respiratory rate (breaths/min) | 18.5±6.2 | 20.4±5.5 | 0.100 |
| Time from injury to ED (min) | 43 (30–60) | 101 (60–240) | <0.001a) |
| ED stay time (min) | 76 (34–137) | 92 (55–149) | 0.555 |
| Time from injury to ED disposition (min) | 138 (82–235) | 218 (159–450) | 0.001a) |
| Admission to ICU | 146 (21.3) | 29 (44.6) | <0.001a) |
| Mortality | 15 (2.2) | 5 (7.7) | 0.027a) |
- 1. Jung KY, Kim JS, Kim Y. Problems in trauma care and preventable deaths. J Korean Soc Emerg Med 2001;12:45–56.
- 2. Kim H, Jung KY, Kim SP, et al. Changes in preventable death rates and traumatic care systems in Korea. J Korean Soc Emerg Med 2012;23:189–97.
- 3. Kim Y, Jung KY, Cho KH, et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J Korean Soc Emerg Med 2006;17:385–94.
- 4. Aprahamian C, Thompson BM, Towne JB, Darin JC. The effect of a paramedic system on mortality of major open intra-abdominal vascular trauma. J Trauma 1983;23:687–90. ArticlePubMed
- 5. Ball CG. Current management of penetrating torso trauma: nontherapeutic is not good enough anymore. Can J Surg 2014;57:E36–43. ArticlePubMedPMC
- 6. Davis TP, Feliciano DV, Rozycki GS, et al. Results with abdominal vascular trauma in the modern era. Am Surg 2001;67:565–70. ArticlePubMedPDF
- 7. Fu CY, Bajani F, Tatebe L, et al. Right hospital, right patients: penetrating injury patients treated at high-volume penetrating trauma centers have lower mortality. J Trauma Acute Care Surg 2019;86:961–6. ArticlePubMed
- 8. Kristiansen T, Lossius HM, Rehn M, et al. Epidemiology of trauma: a population-based study of geographical risk factors for injury deaths in the working-age population of Norway. Injury 2014;45:23–30. ArticlePubMed
- 9. Stormann P, Gartner K, Wyen H, Lustenberger T, Marzi I, Wutzler S. Epidemiology and outcome of penetrating injuries in a Western European urban region. Eur J Trauma Emerg Surg 2016;42:663–9. ArticlePubMedPDF
- 10. Bieler D, Kollig E, Hackenberg L, et al. Penetrating injuries in Germany: epidemiology, management and outcome an analysis based on the TraumaRegister DGU. Scand J Trauma Resusc Emerg Med 2021;29:80. ArticlePubMedPMCPDF
- 11. Van Brussel M, Van Hee R. Abdominal stab wounds: a five-year patient review. Eur J Emerg Med 2001;8:83–8. PubMed
- 12. Civil ID, King M, Paice R. Penetrating trauma in Auckland: 12 years on. Aust N Z J Surg 1998;68:261–3. ArticlePubMed
- 13. Mnguni MN, Muckart DJ, Madiba TE. Abdominal trauma in Durban, South Africa: factors influencing outcome. Int Surg 2012;97:161–8. ArticlePubMedPMCPDF
- 14. Zautcke JL, Morris RW, Koenigsberg M, Carmody T, Stein-Spencer L, Erickson TB. Assaults from penetrating trauma in the State of Illinois. Am J Emerg Med 1998;16:553–6. ArticlePubMed
- 15. Exadaktylos A, Stettbacher A, Edul S, Nichols A, Bautz P. Successful management of abdominal stab wounds with clinical evaluation: experiences of an South-African trauma unit with 496 consecutive patients. Unfallchirurg 2003;106:215–9. PubMed
- 16. Crandall C, Olson L, Fullerton L, Sklar D, Zumwalt R. Guns and knives in New Mexico: patterns of penetrating trauma, 1978-1993. Acad Emerg Med 1997;4:263–7. ArticlePubMed
- 17. Park DJ, Park CY, Cho HM, Lee KH, Han HS. Current status and future prospects of trauma centers in Korea. J Korean Med Assoc 2017;60:530–2. ArticlePDF
- 18. Hoyt DB, Shackford SR, McGill T, Mackersie R, Davis J, Hansbrough J. The impact of in-house surgeons and operating room resuscitation on outcome of traumatic injuries. Arch Surg 1989;124:906–9. ArticlePubMed
- 19. Meizoso JP, Ray JJ, Karcutskie CA 4th, et al. Effect of time to operation on mortality for hypotensive patients with gunshot wounds to the torso: the golden 10 minutes. J Trauma Acute Care Surg 2016;81:685–91. PubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite