Successful treatment of fungal central thrombophlebitis by surgical thrombectomy in Korea: a case report
Article information
Abstract
Fungal thrombophlebitis of the central vein is a rare, life-threatening disease associated with significant morbidity and mortality. It requires immediate central venous catheter removal and intravenous antifungal therapy, combined in some cases with either anticoagulation or aggressive surgical debridement. A 70-year-old male patient injured by a falling object weighing 1,000 kg was transferred to our hospital. A contained rupture of the abdominal aorta with retroperitoneal hematoma was treated with primary aortic repair, and a small bowel perforation with mesenteric laceration was treated with resection and anastomosis. After a computed tomography scan, the patient was diagnosed with thrombophlebitis of the left internal jugular vein and brachiocephalic vein. Despite antifungal treatment, fever and candidemia persisted. Therefore, emergency debridement and thrombectomy were performed. After the operation, the patient was treated with an oral antifungal agent and direct oral anticoagulants. During a 1-year follow-up, no signs of candidemia relapse were observed. There is no optimal timing of surgical treatment for relapsed fungal central thrombophlebitis. Surgical treatment should be considered for early recovery.
INTRODUCTION
Fungal thrombophlebitis of the central vein is a rare, life-threatening disease associated with significant morbidity and mortality. It requires immediate central venous catheter (CVC) removal and intravenous antifungal therapy, combined in some cases with either anticoagulation or aggressive surgical debridement [1–3]. Below we describe a patient who developed candidal thrombophlebitis of the jugular and brachiocephalic veins after major trauma and recovered dramatically after surgery.
CASE REPORT
A 70-year-old male patient injured by a falling object weighing 1,000 kg was transferred to Ulsan University Hospital. At the previous hospital, he was intubated, and a right subclavian CVC was inserted. Because a focused assessment with sonography for trauma exam showed hemodynamic instability and evidence of free intraperitoneal fluid, an emergency operation was undertaken. A multilumen access catheter (MAC) was inserted in the right internal jugular vein (IJV) for rapid administration of blood and fluid. A contained rupture of the abdominal aorta with retroperitoneal hematoma was treated with primary repair, and a small bowel perforation with mesenteric laceration was treated with resection and anastomosis. During postoperative care in the intensive care unit, invasive mechanical ventilation was applied to achieve positive pressure. The patient received total parenteral nutrition, and tazobactam/piperacillin was administered intravenously (4.5 g every 8 hours). Previous medical records of the patient indicated hypertension and diabetes mellitus, and diabetes mellitus had been treated with insulin therapy for many years.
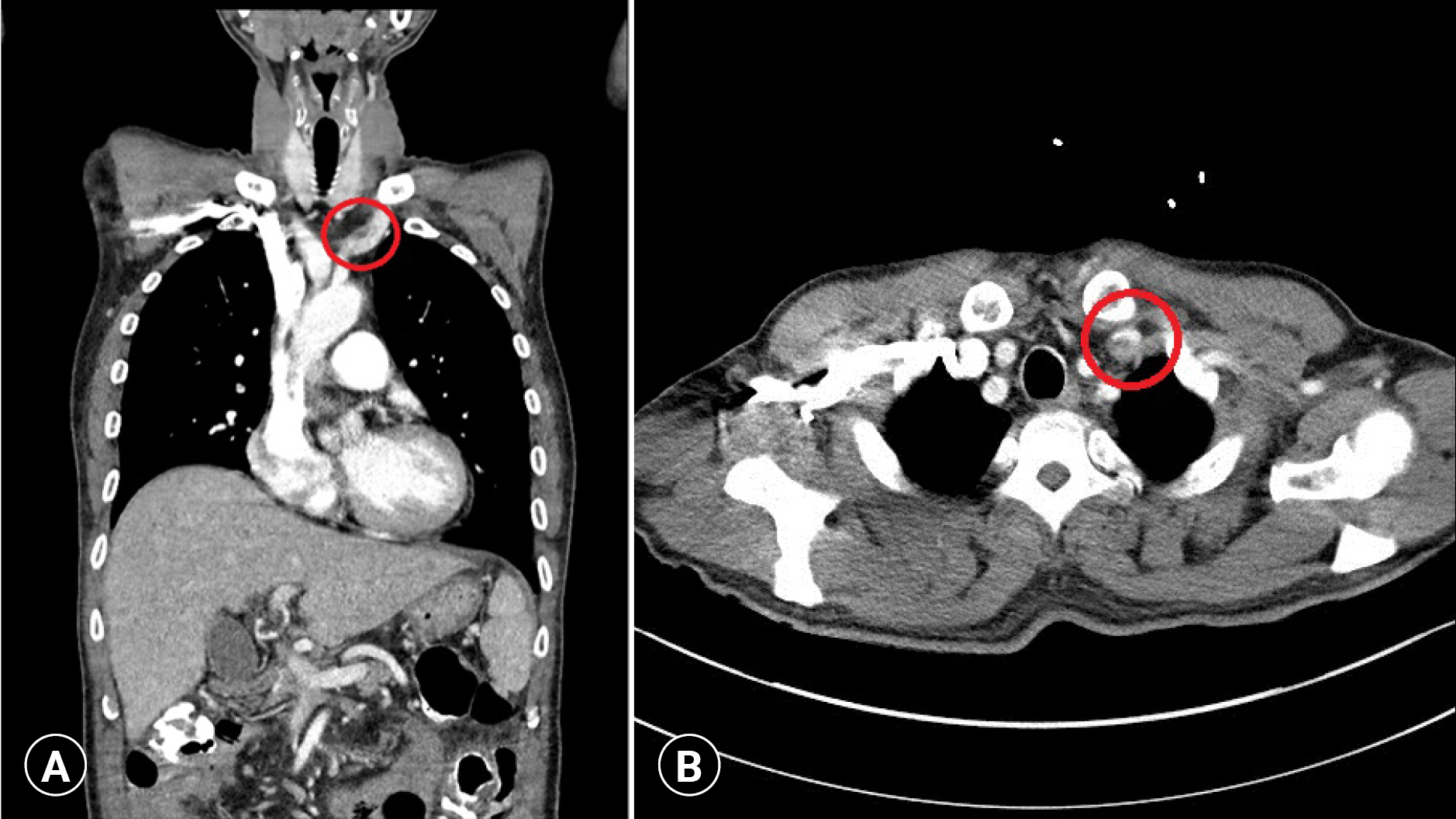
On hospital day (HD) 3, the patient developed a sustained fever. The right IJV MAC and right subclavian CVC were removed and cultured. A CVC was inserted in the left IJV. After extubation on HD 5, the patient was moved to the general ward. Right IJV MAC and right subclavian CVC tip cultures revealed no growth. Administration of antibiotics was stopped on HD 15. On HD 17, the patient became febrile again, and as a result, the left IJV CVC was removed and cultured. Administration of levofloxacin (750 mg/day) was started for empiric antibiotic therapy. Laboratory findings showed a white blood cell (WBC) count of 6,340/μL and a C-reactive protein (CRP) level of 0.53 mg/dL. On HD 18, a computed tomography (CT) scan with contrast was performed on the abdomen and chest to identify the source of fever, but there was no specific finding. Tazobactam/piperacillin (4.5 g every 8 hours) was administered. A spiking fever persisted on HD 19, and the laboratory findings indicated inflammation (WBC count of 8,210/μL, CRP level of 8.80 mg/dL, procalcitonin level of 0.37 μg/L). On HD 21, Candida tropicalis was isolated from the previous left IJV CVC tip (HD 17) and in blood cultures. Micafungin (100 mg/day) was administered immediately, and levofloxacin was stopped. Two sets of peripheral blood cultures were performed. Despite treatment with intravenous micafungin, high fever persisted on HD 22, and laboratory values indicated increasing inflammation (WBC count of 14,510/μL, CRP level of 8.37 mg/dL). The patient was transferred to the intensive care unit. Continuous electrocardiography monitoring detected frequent ventricular premature contractions. When echocardiography was performed, there was no evidence of vegetation. Because the left IJV CVC tip culture finding indicated candidal infection, bedside neck duplex ultrasonography was performed, and a left IJV thrombus was detected. To identify the extent of thrombus formation, a chest CT scan with contrast was performed. A filling defect was identified from the left IJV to the left brachiocephalic vein (Fig. 1). Emergency debridement and thrombectomy of the left IJV and brachiocephalic vein were performed on the same day (Fig. 2). The intraoperative findings were poorly organized, with thrombi and pus in the affected veins. Histological examination confirmed that the thrombus cultures contained C. tropicalis.
After the operation, the patient’s fever subsided immediately. Postoperative blood culture revealed negative results and no isolated C. tropicalis. Laboratory findings indicated resolution of inflammation after postoperative day (POD) 4 (WBC count of 9,210/μL, CRP level of 7.88 mg/dL, procalcitonin level of 0.28 μg/L). Enoxaparin (40 mg/day) was started for anticoagulation on POD 2, then changed to direct oral anticoagulants (apixaban, 5 mg/12 hr) on POD 5. On POD 6, a chest CT scan with contrast showed an obliterated left IJV and brachiocephalic vein due to a newly developed thrombus (Fig. 3). On POD 6, laboratory findings showed no evidence of recurrence (WBC count of 7,450/μL, CRP level of 5.24 mg/dL). The patient was treated with an antifungal agent (oral fluconazole, 150 mg/8 hr) for 4 weeks. Candidemia never recurred. No signs or symptoms of candidemia relapse were observed upon a 1-year follow-up, when a chest CT scan again showed an obliterated left IJV and brachiocephalic vein.
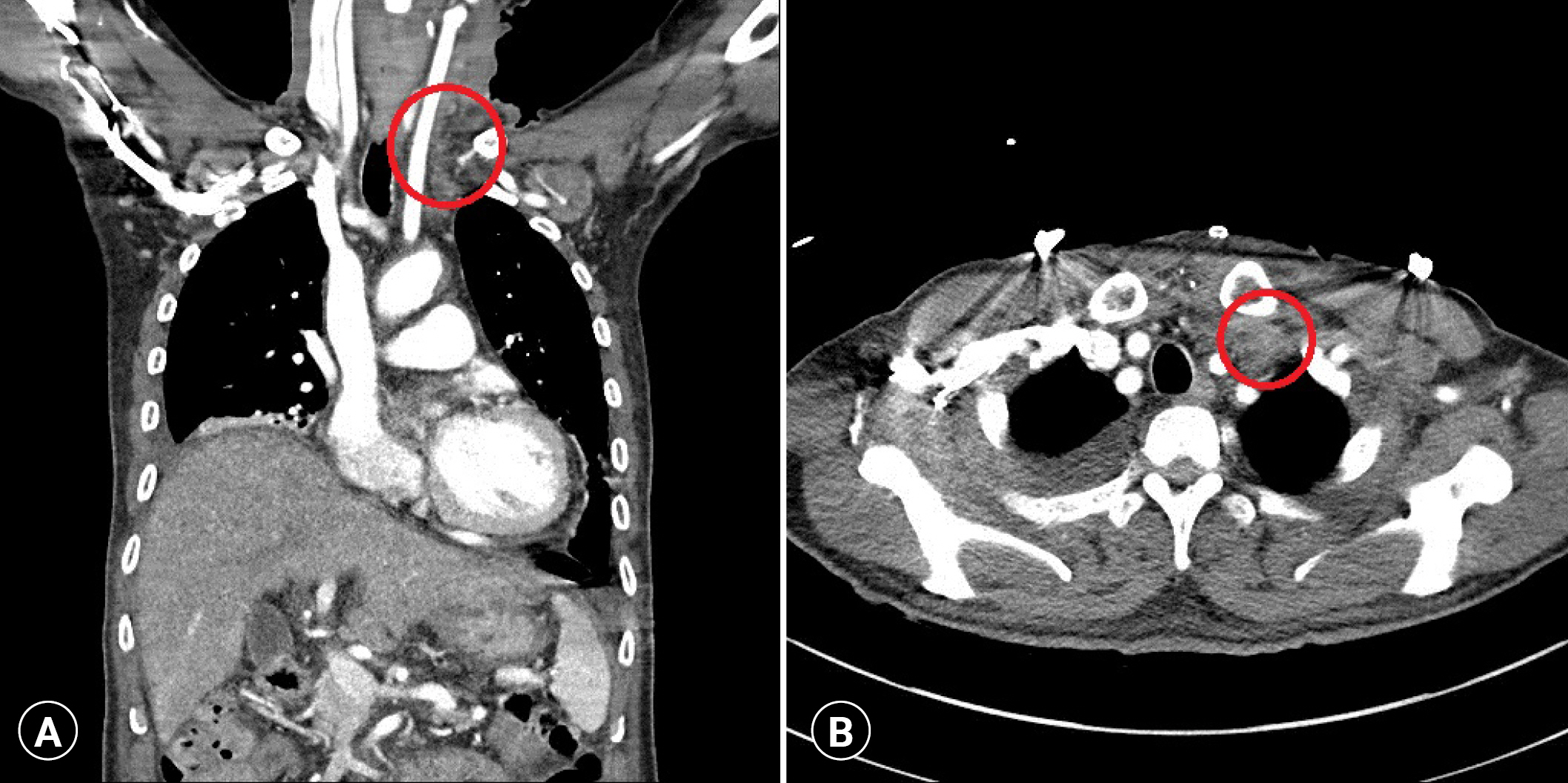
Obliterated left internal jugular vein and brachiocephalic vein (circles) due to newly developed thrombus. (A) Coronal and (B) axial view.
Ethics statement
This study was approved by the Institutional Review Board of Ulsan University Hospital (No. 2022-10-015). The patient provided informed consent for publication of the research details and clinical images.
DISCUSSION
A CVC provides useful vascular access for intravenous therapy, transfusion, and hemodynamic monitoring. However, CVC use may lead to venous thrombus formation, with critical complications such as catheter-associated septic thrombophlebitis. Conservative treatment to remove the infection’s source is usually sufficient, including peripheral or central intravenous catheters, broad-spectrum intravenous antibiotic administration, and possibly anticoagulation. Sometimes this conservative management fails, and surgical approaches such as resection, ligation of the involved veins, or thrombectomy may be supplemented [4].
The incidence of candidiasis has increased gradually in recent decades. Its pathogenesis is not well-known. For candidal suppurative thrombophlebitis, guidelines recommend catheter removal incision and drainage or resection of the vein with administration of an intravenous antifungal agent [5]. An antifungal treatment, such as lipid formulation amphotericin B, fluconazole, or echinocandin, is recommended for at least 2 weeks. Step-down therapy to fluconazole should be considered subsequently for a stable patient who has a fluconazole-susceptible isolate. There are a few surgical treatment methods, including radical excision of the affected vein or thrombectomy. Surgical excision of the vein plays an important role in the treatment of peripheral vein candidal thrombophlebitis.
Candidal thrombophlebitis in CVC is a rare condition that tends to be underdiagnosed. Unlike peripheral vein candidal thrombophlebitis, when a central vein is involved, surgery is usually not available and radical excision is considered controversial [6]. Instead, systemic anticoagulation or thrombolytic treatment has been tried as adjunctive therapy, with insufficient data regarding effectiveness [7].
Treating recurrent patients or patients unresponsive to conservative treatment remains challenging because no definite therapeutic strategy has been established for central candidal thrombophlebitis. In contrast to one report of successful treatment of recurrent candidemia due to central candidal thrombophlebitis with a combination of micafungin and fosfluconazole [8], there has been a report of surgical thrombectomy of the brachiocephalic vein, which effectively removed the source of Candida sepsis and maintained patency of a major vein but resulted in the patient’s death from multiple pulmonary emboli [9]. There has also been a successful report of vena caval thrombectomy and ligation, and the authors of that report suggested surgical intervention when septic pulmonary emboli, extensive thrombophlebitis, or refractory sepsis occur despite optimal therapy [6]. Venous thrombectomy can be a lifesaving treatment for failed conservative management in septic deep venous thrombosis, whether bacterial or candidal [10].
Herein, we performed thrombectomy with debridement without complete excision of the central vein. We decided upon an emergency operation because the patient’s high fever persisted despite antifungal therapy and extension of thrombus. After thrombectomy, the vein was repaired with a Prolene suture without venoplasty. This method may be an option for thrombophlebitis with clear intima after thrombectomy. Though the remaining affected vein could be a source of recurrence, considering the risk, we chose to leave the vein in place unless it became inflamed. After surgery, anticoagulation was started on POD 2, and the patient showed early signs of recovery. At the 1-year follow-up, there was no evidence or symptom of candidemia.
Fungal central thrombophlebitis is a rare and probably underdiagnosed infectious complication of critically ill patients. Recurrent or persistent candidemia after removal of a contaminated CVC should prompt further investigation, and surgical treatment should be considered in the disease’s early phases for timely recovery and prevention of fatal complications.
Notes
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
The authors did not receive any financial support for this study.
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
Author contributions
Conceptualization: JTK; Data curation: JTK; Investigation: EJL; Visualization: EJL; Writing–original draft: EJL; Writing–review & editing: all authors. All authors read and approved the final manuscript.