Analysis of Errors on Death Certificate for Trauma Related Death
Article information
Abstract
Purpose
This study was to investigate errors of death certificate (DC) issued for patients with trauma.
Methods
A retrospective review for DC issued after death related to trauma at a training hospital trauma center was conducted. Errors on DC were classified into major and minor errors depending on their influence on the process of selecting the cause of death (COD). All errors were compared depending on the place of issue of DC, medical doctors who wrote the DC, and the number of lines filled up for COD of DC.
Results
Of a total 140 DCs, average numbers of major and minor errors per DC were 0.8 and 3.7, respectively. There were a total of 2.8 errors for DCs issued at the emergency department (ED) and 5.4 errors for DCs issued beyond ED. The most common major error was more than one COD on a single line for DCs issued at the ED and incompatible casual relation between CODs for DCs issued beyond ED. The number of major errors was 0.5 for emergency physician and 0.8 for trauma surgeon and neurosurgeon. Total errors by the number of lines filled up for COD were the smallest (3.1) for two lines and the largest (6.0) for four lines.
Conclusions
Numbers of total errors and major errors on DCs related to trauma only were 4 and 0.8, respectively. As more CODs were written, more errors were found.
INTRODUCTION
The main function of a death certificate (DC) is to prove an individual’s death. It provides the cause of death (COD) and serves as evidence when facing legal problems for one person’s death [1]. In addition, if medical doctors write the DC as professionals who treat the patient, a well written DC would be the best consideration for the patient and the bereaved family. The DC of farmer Baek Nam-Gi who died in September 2016 after being water cannon shot by police during a protest in November 2015 has become a hot topic in South Korea. The manner of death for that DC was changed from disease related death to trauma related death after much social debate. The importance of DC has been highlighted once again [2].
Previous studies have determined general characteristics of errors of DCs and the effectiveness of education in reducing errors [1,3–12]. However, no study has reported errors of DC related to trauma only. Thus, the objective of this study was to investigate errors of DC issued for patients with trauma.
METHODS
Data of DC issued after death related to trauma at a training hospital designated as the regional trauma center from September 2015 located in a southeastern coast area of South Korea were analyzed retrospectively from September 2015 to August 2017. This study was approved by the relevant Institutional Review Board.
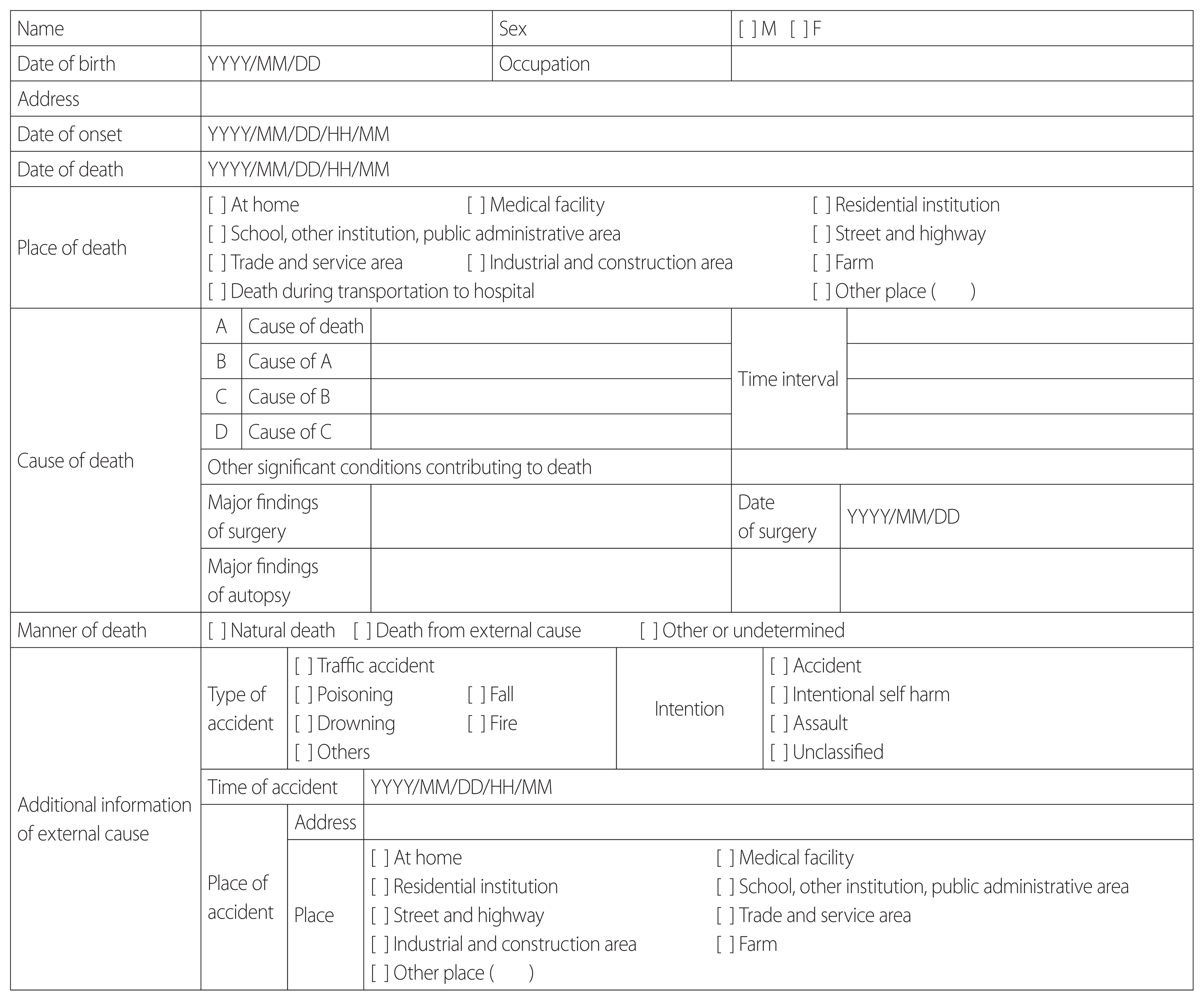
There has been no specific educational program for how to write DC in South Korea. It is possible for several CODs for one situation in the DC and even the some CODs are vaguely documented in the DC guidelines. Therefore, the knowledge and experience for the DC are important to judge the error of that. Two emergency physicians who have been well aware of guideline for DC of World Health Organization, Korea Medical Association and had experience in research on DC, judged errors of DC [7]. Also, they knew well about statistical production process associated with DC in Statistics Korea and participated in workshop for DC organized by the Statistics Korea. Although the emergency physicians did not well know the details of the surgical findings, however there was no problem to judge the error of the DC since it is critical to determine whether the surgical findings depending on the medical records were recorded appropriately in the DC. Each emergency physician judged errors of DCs respectively by referring to DC and medical records. If they had different opinions in determining errors, final errors were determined based on discussion and consensus. If it was hard to determine whether the manner of death was due to external cause or natural death based on their medical record, the case was excluded from this study. Evaluation for errors of DC was based on guidelines of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) [13,14]. Using the form of DC commonly used in South Korea (Fig. 1), assessment of errors was divided into three parts. Part I evaluated COD and the manner of death. Part II evaluated the time interval from onset to event or death, other significant conditions not associated with the COD, major findings of surgery, and date of surgery. Part III evaluated type of accident, intention, time of accident, and place of accident (Table 1).
Definition of errors
Errors on DC were classified into major and minor errors depending on their influence on the process of selecting the COD [6,8,10,11,15]. Major errors were those related to Part I of the DC: 1) mode of dying as the underlying COD (UCOD) such as cardiac arrest, heart failure, respiratory failure; 2) secondary conditions as the UCOD without an antecedent COD such as pulmonary embolism, sepsis; 3) ill-defined conditions as the UCOD such as senility, symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified corresponding to ICD-10 codes for R00–R94 and R96–R99; 4) improper sequence of time between CODs; 5) incompatible causal relationship such as two or more unrelated CODs; 6) listed more than one COD on a single line in Part I; 7) blank line between CODs or duplicated the same COD; 8) incorrect manner of death; and 9) unacceptable COD with evidence of an illogical decision (Table 1). Minor errors were those related to Part II, Part III, and some of Part I of the DC: 1) mode of dying as the COD with appropriate UCOD; 2) no cause of injury as UCOD; 3) no result of injury as COD; 4) unclear COD with clear cause of injury as UCOD; 5) incorrect time interval; 6) incorrect other significant conditions; 7) incorrect operating findings even after surgery; 8) incorrect date of surgery even after surgery; 9) incorrect type of accident; 10) incorrect intention of external cause; 11) incorrect time of accident; and 12) incorrect place of accident (Table 1).
As a general characteristic of DC, the place of issue of DC was classified into emergency department (ED) or beyond ED including intensive care unit and surgery room. The medical doctor who wrote the DC was classified as board certified emergency physician, board certified trauma surgeon, neurosurgeon, and other residents. Based on medical records, whether the patient underwent surgery between trauma onset and death was investigated. How many lines among four lines of Part I for COD (Fig. 1) were entered were also investigated. All major and minor errors were investigated.
All errors were compared depending on the place of issue of DC, medical doctors who wrote the DC, and the number of lines filled up for COD of DC. Chi-square test and student’s t-test were used for comparing errors depending on the place of issue of DC. Errors depending on the specialty of medical doctors and the number of lines filled up for COD of DC were compared using analysis of variance (ANOVA) with Scheffe post hoc test, chi-square test, and Fisher’s exact test. IBM SPSS version 24.0 (IBM, Armonk, NY, USA) was used for all statistical analyses. Statistical significance was defined at p<0.05.
RESULTS
A total 140 DCs out of 142 DCs were analyzed during the study period except two cases for which COD could not be determined. Regarding the place of issue of DC, 38% were ED and 62% were others. Regarding medical doctors who wrote the DC, 35% were board certified trauma surgeon, 31% were board certified emergency physician, 27% were neurosurgeon, and 7% were others under medical residency. An average of 2.4 lines for COD were recorded. The most common cases were recorded in two lines (34%) or three lines (29%) for COD. Average numbers of major and minor errors per DC were 0.8 and 3.7, respectively. In particular, 5.4 minor errors were found in 45 cases that had surgery while 2.8 minor errors were found in 95 cases that had no surgery (Table 2).
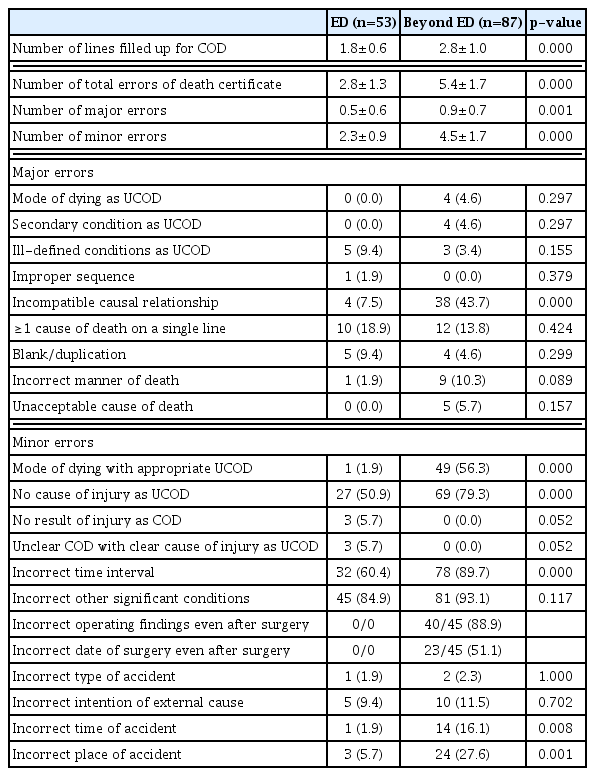
DCs issued at the ED were filled up with 1.8 lines for COD. For DCs issued beyond ED, they were filled with 2.8 lines. There were a total of 2.8 errors for DCs issued at the ED and 5.4 errors for DCs issued beyond ED. The most common major error was more than one COD on a single line for DCs issued at the ED and incompatible casual relation between CODs for DCs issued beyond ED. Minor error with mode of dying followed by a legitimate COD was 2% for DCs issued at the ED and 56% for DCs issued beyond ED. Minor error with no cause of injury as the UCOD was 51% for DCs issued at the ED and 79% for DCs issued beyond ED (Table 3).
The number of lines filled up for COD was 3.4 for neurosurgeon, 2.4 for trauma surgeon, and 1.9 for emergency physician. The number of major errors was 0.5 for emergency physician and 0.8 for trauma surgeon and neurosurgeon. Major error with incompatible causal relationship was the most common in neurosurgeon (63%). More than one COD on a single line was the most common in trauma surgeon (29%). Major error with incorrect manner of death was common in other medical doctors under medical residency (50%). Minor error with mode of dying followed by a legitimate COD was common in neurosurgeon (68%). No operating finding even after surgery was 72%. It was 100% for both trauma surgeon and neurosurgeon (Table 4).
Total errors by the number of lines filled up for COD were the smallest (3.1) for two lines and the largest (6.0) for four lines. Major error with only mode of dying as UCOD was 14% for one line. Incompatible casual relationship was 35% for three lines and 92% for four lines. Minor error with mode of dying followed by a legitimate COD was 13% for two lines and 88% for four lines (Table 5).
DISCUSSION
Of a total of 140 DCs included in the study, only one DC had no major or minor error. This is similar to previous studies showing that major errors are found in more than 50% of issued DCs or minor errors are found in most DCs, with DCs having no errors account for only 1% [3,5,6,16]. Cases with no cause of injury as the UCOD accounted for 69% (96/140) in this study. This result reflects that in many cases, principles for writing DCs related to trauma are not well understood or adhered to. In order to reduce these errors, efforts are needed to improve the quality of a DC through a feedback system which evaluates the adequacy of a DC in the institution where the DC is issued [10,17]. Continuous education is also required for individuals authorized to write the DC [4,7,8,11,18].
A previous study has found that the lower the age of the issuer and the lower the level of the issuing hospital, the greater the number of errors of DC [9]. Total number of errors was the smallest in board certified emergency physicians while the number of major errors was the largest in others under medical residency in this study. This may be related to the experience for writing DC. Emergency physician would have experienced relatively many cases of death in the ED and in issuing DC. However, the understanding for DC and the experience for issuing DC of residents would be poor. Moreover, more errors for incorrect manner of death were found in case of the patient being transferred to other specialty especially internal medicine because of complication after admitted to trauma team first.
In this study, the higher the number of lines for COD, the higher the number of errors, especially minor errors. Common minor errors were missing time interval or other significant conditions in previous studies [3,6,10,11]. Even if four lines for COD were recorded in this study, 88% were missing time interval and 96% were missing other significant conditions. Although the specific characteristics of medical doctors who filled up a lot of lines for COD of DC were not investigated in this study, this might reflect a misconception of them that if more or all lines for COD of DC were recorded, the more accurate the DC would be. A poor knowledge and misconception for writing the DC might result in more lines filled up for COD, thus leading to more errors.
In a previous study, among 307 cases of DCs with 162 cases of natural death, 50 cases of external cause, 95 cases of undetermined or unknown cause, and 17 cases (5.5%) of the total DCs were found to have errors for incorrect manner of death with 10 cases being issued as undetermined or unknown cause instead of external cause and seven cases being issued as natural death instead of external cause [12]. Errors for the manner of death in this study that included only DCs related to trauma accounted for 7.1% (10/140). These results reflect that it is unlikely that natural death would be wrongly issued as the death from external cause. However, there is a high possibility that the death from external cause would be wrongly issued as natural death. In particular, the longer the time from an accident to death, the greater the confusion about the direct COD and its relevance to trauma, and the more likely it will lead to errors in determining the manner of death.
In case of trauma related death, it is likely that the subject of responsibility for the cause of trauma is more controversial than in natural death. If there is a conflict between parties concerned about the outcome of death, the DC would be an important document to resolve the dispute. It is not easy to issue a DC correctly with limited clinical information without any findings from an autopsy. However, the issuer of the DC is responsible for issuing it as accurately as possible according to medical knowledge and guidelines for writing the DC, although they might only have limited clinical information.
The result of this study cannot be generalized because only DCs issued by a training hospital were included. In addition, although we examined errors according to medical doctors, the experience or educational status for writing the DC of doctors were not investigated.
CONCLUSION
Numbers of total errors and major errors on DCs related to trauma only were 4 and 0.8, respectively. As more CODs were written, more errors were found. Thus, Education and steady quality control are needed to improve the quality of DC.