Mortality Reduction in Major Trauma Patients after Establishment of a Level I Trauma Center in Korea: A Single-Center Experience
Article information
Abstract
Purpose
Trauma systems have been shown to decrease injury-related mortality. The present study aimed to compare the mortality rates of patients with major trauma (injury severity score >15) treated before and after the establishment of a level I trauma center.
Methods
During this 20-month study, participants were divided into pre-trauma center and trauma center groups, and trauma and injury severity score (TRISS) method was used to compare mortality rates during 10-month periods before and after the establishment of the trauma center (October 2013 to July 2014 vs. October 2014 to July 2015).
Results
Of the 541 total participants, 278 (51.5%) visited after the establishment of the trauma center. The Z and W statistics indicated better outcomes in the trauma center group than in the pre-trauma center group (Z statistic, 2.635 vs. −0.700; W statistic, 4.640). The trauma center group also exhibited meaningful reductions in the time interval from the emergency department (ED) visit to emergency surgery (118.0 minutes vs. 142.5 minutes, p=0.020) and the interval from the ED visit to intensive care unit admission (202.0 minutes vs. 259.0 minutes, p=0.035) relative to the pre-trauma center group.
Conclusions
The TRISS and multivariate analysis revealed significant improvements in survival rates in the trauma center group, compared to the pre-trauma center group.
INTRODUCTION
Traumatic injury, the fifth leading cause of death in the USA, places substantial burdens on society in terms of losses in productivity and increases in disability and the use of health care resources [1]. Accordingly, standards of care for trauma patients have been developed to reduce trauma-related mortality in the USA, and optimal resources have been allocated to designated trauma centers at three levels that account for resources, education, and research commitment [2]. The criteria used to categorize hospitals according to the resources needed to provide different levels of care for patients with traumatic injuries have been published and are increasingly applied to the designation of trauma centers as part of a regionalized approach to trauma care [3]. Several studies have revealed that after the implementation of a designated trauma system, the risk of trauma death decreased significantly among trauma center patients relative to pre- or undesignated trauma center patients. Moreover, comparative studies of multiple trauma center levels reported that patients at level I trauma centers had markedly better survival and functional outcomes, compared to those at level II or undesignated trauma centers [4].
In Korea, trauma injury is the fourth leading cause of death and the leading cause of death among individuals aged ≤40 years [5]. The proportions of preventable deaths among all trauma deaths were 50.4% between 1996 and 1997, 39.6% between 2003 and 2004, and 29.8% between 2009 and 2010 [6]. Despite the decreasing trend, the preventable death rate remain higher in Korea than in other developed countries, indicating the need for improvements in the quality of emergency medical service triage and training, the treatment and training provided by trauma care facilities, and the organization of the trauma system [7].
In Korea, the absence of a trauma team or trauma center represents a significant limitation in the treatment of patients with severe trauma. Most cases of preventable death in Korea (51.9%) can be attributed to events occurring in the emergency department (ED). Specifically, 71.3% of these events involving treatment in the ED represented serious issues with the treatment of severe trauma patients [8].
Accordingly, policymakers began to develop national policies regarding the establishment of a trauma system, and designated several level I trauma centers while taking into account the accessibility and equity of healthcare service delivery in each region. Sixteen hospitals have been designated as level I trauma centers since 2014, and 9 centers are currently in operation, including a level I trauma center established at our institution in October 2014.
Despite the significant investment of medical and human resources into the development of a Korean national trauma system, previous studies have not evaluated the effectiveness of these trauma centers. Accordingly, the present study aimed to comparatively evaluate the mortality rates of patients with major trauma (injury severity score [ISS] >15) treated before and after the establishment of a level I trauma center.
METHODS
Establishment of the trauma center
A trauma center in Korea is a regional medical center with health professionals and specialized resources that allow for the round-the-clock care of victims with critical injuries. These centers employ trauma teams to respond to severely injured patients within 10 minutes of activation and provide integrated and essential injury management. The ability to provide prompt and appropriate medical treatment to serious trauma patients immediately upon arrival, which is conferred by the presence of independent equipment, manpower, and space, is the most important characteristic of a trauma center.
First, a trauma center in Korea is required to dedicate facilities specifically for major trauma patients. These facilities include dedicated emergency resuscitation rooms, 2 operation rooms, a 40-bed ward, and a 20-bed intensive care unit, as well as an intervention room only for severely injured patients. The trauma center also operates exclusive computed tomography and X-ray rooms and is equipped with tools to perform advanced techniques such as ultrasound, continuous renal replacement therapy, and extracorporeal membrane oxygenation. Second, the trauma center must also employ a dedicated medical staff comprising an emergency physician, trauma surgeon, thoracic surgeon, neurosurgeon, orthopedic surgeon, anesthesiologist, and radiologist, as well as 2 nurses tasked with the resuscitation of major trauma patients. These professionals remain on standby 24 hours per day and serve only trauma patients, Third, the medical staff of the trauma center must plan to improve their trauma treatment capabilities through trauma quality management, trauma database construction management, and professional workforce training projects. To meet these requirements, 16 billion won (50% each from the central government and our institution) were spent to equip our facilities for trauma center establishment. Additionally, the annual expenses associated with maintaining a dedicated medical team for trauma patients total 2 billion won.
Patient population
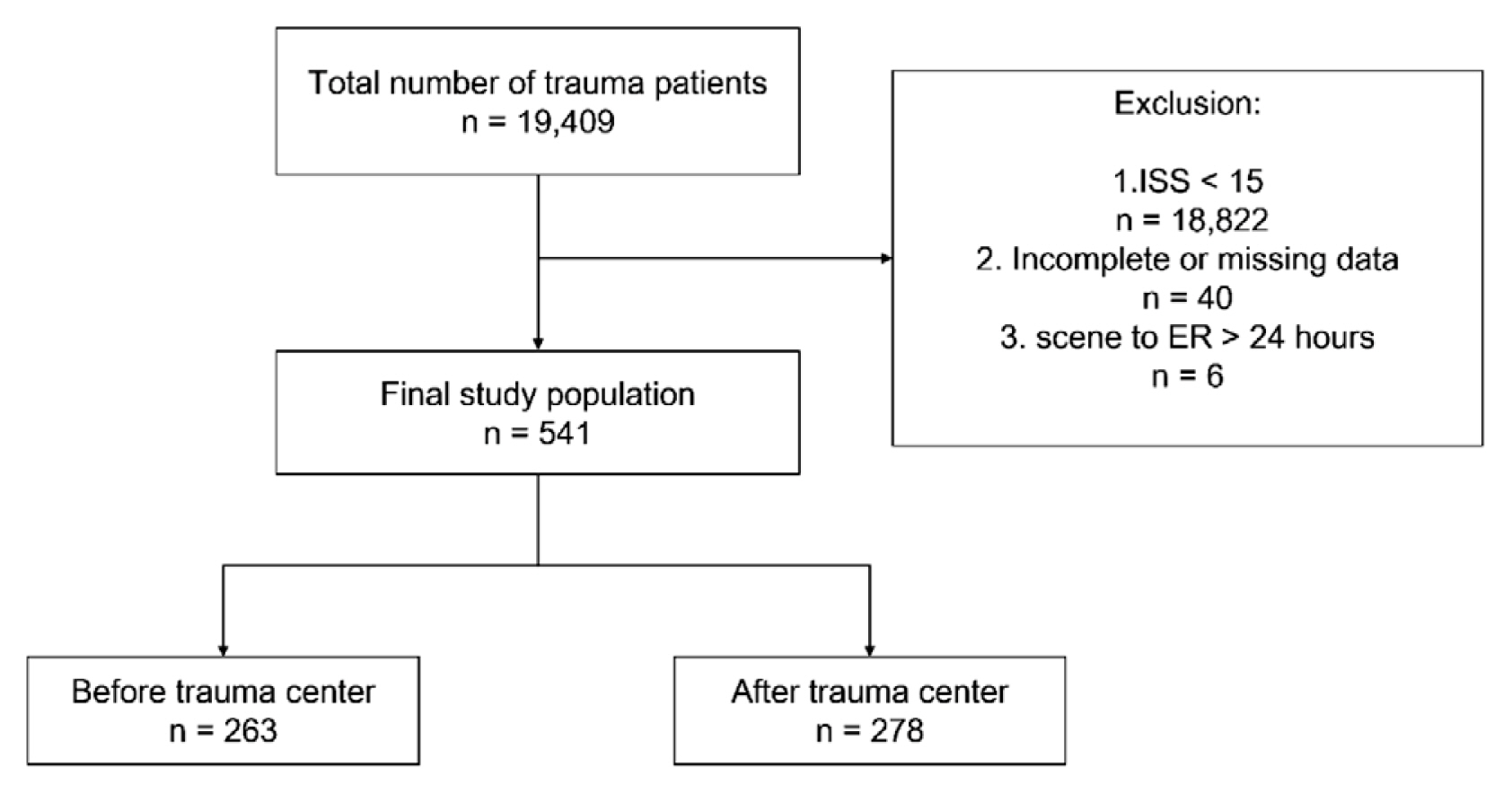
We collected data of patients with major trauma (ISS >15) who were treated at our institution (Supplementary Table 1). Patients were categorized into two groups according to the admission date: the pre-trauma center group comprised patients admitted between October 2013 and July 2014, and the trauma center group comprised patients admitted between October 2014 and July 2015. The following exclusion criteria were applied to the 19,409 trauma patients admitted during the study period: an ISS <15, lack of vital signs on admission and declaration of death within 30 minutes of arrival at the ED (n=18,822), an elapsed time from injury to ED arrival of >24 hours (n=6), and missing or incomplete data (n=40) (Fig. 1). Finally, 541 patients were included in this study. Of these, 263 (48.5%) and 278 (51.5%) patients were included in the pre-trauma center and trauma center groups, respectively.
Study design and data acquisition
This study featured an observational cohort design and prospective data collection. The data were obtained from electronic medical records, the National Emergency Department Information System (NEDIS), and the Korean Trauma Data Bank (KTDB). The NEDIS and KTDB were developed to serve as national data repositories and are managed by the Korean government. Level I trauma centers are required to register with the NEDIS and KTDB. The following data were collected: systolic blood pressure (SBP), diastolic blood pressure, pulse rate, respiratory rate (RR), and Glasgow coma score (GCS) on arrival (measured as part of the initial ED assessment). The following time intervals to outcomes were also measured: time from injury to ED arrival, time from ED visit to emergency surgery, time from ED admission to intensive care unit (ICU) admission, and ICU length of stay (days) or total hospitalization time. We also included variables regarding the injury mechanism, the abbreviated injury scale, and ISS.
Calculation of the trauma and injury severity score (TRISS)
In this study, we applied the TRISS because this method offers a standard approach for tracking and evaluating the outcome of trauma cares, provides an excellent screening tool for case identification in a quality assurance review, and allows the comparison of outcomes among different populations or trauma patients [9]. The TRISS score is calculated from anatomic, physiologic, and age characteristics and used to quantify the probability of survival (Ps) in patients with major trauma. Three factors (ISS, revised trauma scale [RTS], and age) are needed to calculate the TRISS. The RTS can be calculated from the initial vital signs of SBP, RR, and GCS. The Z score and W statistics were also calculated. The Z statistic, first described by Flora, quantifies the difference between the actual number of deaths (or survivors) in a subset (e.g., institution) and the predicted number of deaths (or survivors), according to the baseline [10].
Statistical analyses
Statistical analyses were performed using SPSS version 20 (IBM Corp., Armonk, NY, USA) and SAS software version 9.4 (SAS, Inc., Cary, NC, USA). Continuous data are summarized as proportions, means, and medians with interquartile ranges (IQRs). We compared the patients’ demographic characteristics and outcome variables using a chi-square analysis or independent t-test. Both the predicted and actual patient mortality were compared using Z and W statistics. The Z statistic is to compare the actual number of survivors of the medical institutions under evaluation with the number of expected survival patients based on existing quality standards. Generally, when the number of patients to be surveyed is 150 or more, when the Z-statistic exceeds +1.96 or −1.96, the mortality rate is statistically higher or lower than the existing quality standard. Because the ability to detect statistically significant differences in survival rates by Z statistics is strongly influenced by the number of patients surveyed, the quality of emergency medical institutions cannot be assessed solely by the Z-statistics. W statistic was developed to accurately estimate the magnitude of the difference in survival probability. The W statistic estimates the number of survivors expected using the Major Trauma Outcome Study (MTOS) norm per 100 patients analyzed and allows more accurate comparisons between different institutions or systems [9,11,12]. Additionally, a multiple logistic regression model was used to examine the adjusted associations between trauma center establishment and trauma patient survival.
Ethics statement
This study was approved by our institutional review board (IRB No.: CR317038). The requirement for informed consent was waived by the IRB because of the observational nature of this research.
RESULTS
In a comparison of the pre-trauma center and trauma center groups, we observed no significant differences in sex, median age, level of hypotension on arrival, GCS score, and median ISS value (Table 1). In addition, there were no intergroup differences in the time from injury to ED attendance among patients who visited the hospital directly after injury (44 minutes in the pre-trauma center group vs. 44 minutes in the trauma center group). However, this time interval differed significantly between the groups among cases involving inter-hospital transportation (224 minutes in the trauma center group vs. 183 minutes in the pre-trauma center group; p=0.015) (Table 1). By contrast, the time interval from ED arrival to emergency surgery commencement and ED arrival to intensive care unit admission were significantly shorter in the trauma center group (118.0 minutes vs. 142.5 minutes in the pre-trauma center group, p=0.020 and 202.0 minutes vs. 259.0 minutes in the pre-trauma center group, p=0.035), respectively (Table 2). In both groups, the most common injury mechanism was motor vehicle accident, followed by fall, and this parameter did not differ significantly between the groups. Although no intergroup differences were observed in the mean ISS and RTS values, a sub-group analysis according to survival found that the trauma center group had a lower RTS value than the pre-trauma center group (7.26±1.00 vs. 7.45±0.77, p=0.018), although the differences were insignificant among non-survival patients (Table 3).
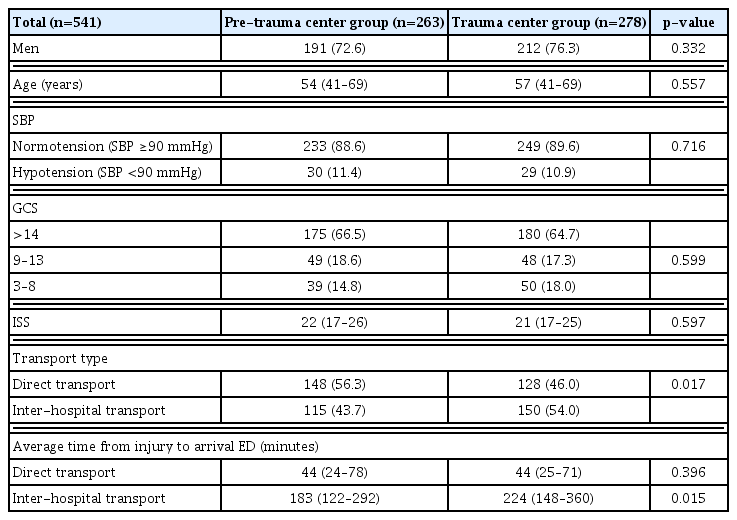
Comparison of general patient characteristics before and after the establishment of the level I trauma center

Comparison of injury mechanisms, ISS, and RTS scores before and after the establishment of the level I trauma center
The predicted and actual survival rates of patients in the pre-trauma center group were 88.3% and 87.1%, respectively, yielding a 1.2% decrease. In the trauma center group, the predicted and actual survival rates were 86.3% and 89.9%, respectively, yielding a 3.6% increase. In an intergroup comparison of Z and W statistics, the trauma center group was revealed a significant mortality reduction with an increase of 4.64 survivors per 100 patients relative to the pre-trauma center group (Z statistics, 2.635 vs. −0.700; W statistics, 4.640) (Table 3). Therefore, the trauma center group exhibited a significant increase in survival, compared to the pre-trauma center group. By contrast, the ICU stays of 4 days (IQR, 1.0–11.8) in the pre-trauma center group and 5 days (IQR, 1.0–12.0) in the trauma center group did not differ significantly. Similarly, the total lengths of hospitalization were similar, with 22 days (IQR, 10.0–41.0) in the pre-trauma center group and 23 days (IQR, 10.0–38.5) in the trauma center group.
To clarify our findings, we used a multiple logistic regression model adjusted for potential confounders (baseline patient and general characteristics and injury severity) to evaluate the association between trauma center establishment and risk-adjusted survival in the study population (Table 4). Accordingly, we found that the trauma center group had an odds ratio for survival of 1.91 (95% confidence interval [CI], 1.03–3.61) relative to the pre-trauma center group. The regression model used in this study exhibited excellent discrimination (C statistic, 0.880).
DICCUSSION
The present study demonstrated a significant increase in the survival rate of patients with severe trauma (ISS >15) after the establishment of the level I trauma center at our institution. The positive Z statistic (z=2.635) calculated in this study indicates that the performance of this center exceeds the national standard (USA) for hospitals that provide trauma care. By including multiple covariates reflective of injury severity (e.g., ISS, physiologic characteristics, and transport type), we further identified more favorable survival outcomes in the trauma center group (Table 4). Furthermore, we demonstrated that this trauma center-related improvement in survival persisted despite the lower RTS scores of trauma center group survivors relative to their pre-trauma center group counterparts (Table 3). As no other changes to the diagnostic or therapeutic procedures applied to trauma patients were made during this period, the reduction in mortality in this study is attributed to the effects of the trauma center. Furthermore, this is the first Korean study to report a reduction in mortality among patients with major trauma treated at a level I trauma center. As the actual effectiveness of a trauma care system can be assessed by its impact on mortality among severely injured patients who would otherwise be expected to die without timely diagnosis and management, this study also evaluated the effect of trauma center care on the outcomes of patients with an ISS of ≥15 and compared these results with the MTOS data from 1987 [12,13].
Numerous studies in developed countries have demonstrated an association between the establishment of level I trauma centers and decreased mortality following major trauma. A TRISS-like analysis of Stewart’s study revealed a significant increase in the Z-score from +1.34 pre-designation to +2.97 post-designation [14]. Champion et al. [15] found that an increased institutional commitment to excellence in trauma care and the establishment of a trauma system in the hospital area were associated with significantly improved outcomes among trauma patients. MacKenzie et al. [3] reported that after adjusting for differences among cases, the in-hospital mortality rate was significantly lower at trauma centers than at pre-trauma centers (7.6% vs. 9.5%; relative risk; 0.80; 95% CI, 0.60–0.95). The effect of treatment at a trauma center varied according to the severity of injury, with evidence suggesting that differences in mortality rates were primarily confined to patients with more severe injuries. Despite a lack of direct comparison between trauma centers and pre-trauma centers, Demetriades et al. [4] reported that patient mortality was significantly lower at level I centers than at other-level trauma centers and undesignated hospitals (25.3% vs. 29.3%). In that study, a multivariate analysis adjusted for age (≤65 and >65 years), mechanism of injury (blunt and penetrating), hypotension on admission (SBP <90 mmHg), and ISS (>25) revealed that the adjusted mortality among patients admitted to level I trauma centers was significantly lower than that of patients admitted to level II trauma centers. The authors also reported that level I centers were associated with significantly better functional outcomes at discharge.
The time to definitive care is very important for severely injured patients, and the immediate availability of an operating facility and personnel may be critical to survival. Treatment failure often occurs in patients with severe injuries who are not prioritized in terms of the use of hospital medical resources and subjected to with needless delays; ultimately, this neglect may result in death due to exsanguination or intracranial hemorrhage [16]. A study by Shackford also found that surgery is one of the most frequently needed early interventions among major trauma patients, thus supporting the use of a dedicated, fully staffed operation room that is available at all times for the care of patients with trauma [17]. Similarly, we observed significant decreases in the ED to operation time and the ED to ICU time in our trauma center group. Although many variables may have affected these improvements in trauma care outcomes during the study period, the above-mentioned reductions in time may be related to the provision of optimal management to injured patients and subsequently reduced mortality among patients treated after the establishment of a trauma center.
After the trauma center was established, we observed a significant increase in the proportion of patients referred by inter-hospital transport from 46% to 54% (p=0.017). We can only speculate the reasons for this increase. Although surrounding hospitals may seek to admit more critically injured patients to the trauma center, we also observed an increased time from injury to ED arrival following inter-hospital transport in the trauma center group. This finding is problematic in light of the postulation that a decreased time between injury and definitive care improves trauma outcomes. The American College of Surgeons recommends that severely injured patients should ideally arrive at the ED within the ‘golden hour’ [18]. A study by Young also found that fewer unexpected deaths occurred among patients transferred directly to the trauma center, compared to those in the inter-hospital transport group. Among patients who survived for >24 hours, the ICU and hospital stay lengths were significantly shorter in the direct transport group [19]. A study of the pre-hospital times of patients with acute traumatic subdural hemorrhage found those who arrived promptly at the designated trauma center from the scene of injury were more likely to survive [20]. This finding supported the concept of the ‘golden hour’ in terms of the outcomes of severely injured patients, particularly those with severe brain injuries. Therefore, we aim to increase the proportion of patients transported directly to the trauma center in our catchment area. Under these circumstances, we anticipate that the survival outcomes will improve among patients with major trauma.
Limitations
This study had several limitations of note. First, seasonal variations in the mechanism of injury among patients with trauma have been well recognized in Korea, which has 4 seasons. However, the observation period used in this study (10 months) did not comprise a full year. To minimize seasonal bias, subjects in both groups were enrolled during the same span of months. Second, although nine level I trauma centers are currently operating in Korea, our study describes only the experiences at a single center. Furthermore, as this study examined survival outcomes of patients at a suburban trauma center, our findings cannot readily be applied to other rural or urban areas in Korea. Therefore, our findings should be generalized with caution. Third, we were unable to obtain comparable data from other medical institutions in our region that treat trauma patients and therefore could not conduct an analysis of differences among the institutions. Fourth, this study relied on data from a registry, NEDIS, and KTDB, which attempt to aggregate a large variety of mechanisms and locations of injury, degrees of physiologic reserve, and causes of death into legitimate analytic categories over time. Furthermore, scoring systems unavoidably introduce biases via their data structures and changes in diagnostic acumen. For example, the ISS is a measure of anatomic injury that limits the maximization of scores in any given anatomic region, thus obscuring the impacts of multiple-organ, single-region injuries [21]. Analysis of the ISS-dependent identification of all injuries and vary with time and the skills of individual trauma registrars. However, the study design is strengthened by the data analysis derived from consecutive patients. Injury descriptions were consistently coded by a limited number of persons selected by the government, who received specific training. In more detail, the registrars in our institution are a dedicated trauma physician on duty and reviewed by trauma coordinator and the dedicated physician again, nevertheless this potential bias cannot be completely excluded [22]. Fifth, this study was limited by the RTS system. In intubated patients admitted to the ED, the number of spontaneously breathing patients may not be accurately determined, leading to the loss of data and exclusion of patients from the study. However, this limitation equally affected the pre-trauma center and the trauma center groups; additionally, incomplete data accounts for <8% of cases, according to the RTS. Accordingly, a countermeasure is needed for intubated patients. Sixth, we used the TRISS method for comparing effectiveness but, the TRISS method has some limitations for measurement of survival rate. TRISS relies on physiological parameters and has several problems such as missing data from data sets and the fact that the use of the GCS score in trauma patients has poor interobserver agreement and requires adjustment of scores for intubated patients. It has been poorly predictive of outcomes in the elderly. It also has significant limitation for comparing outcomes in the Korean population with those in the MTOS population from the 1980s. Despite these limitations, the TRISS is commonly used as the gold standard method for evaluating results in trauma patients. Seventh, this study relied on mortality as an adequate measure of trauma care effectiveness. Outcome measures used to evaluate the effects of a trauma center and trauma system should also incorporate variables such as disability after trauma, rehabilitation, quality of life, and long-term prognosis. Finally, the cost-effectiveness of trauma centers remains unexplored in Korea, and future analyses should include an evaluation of the functional outcomes of survivors of major trauma.
CONCLUSION
Standard TRISS and multivariate analyses of patients admitted before and after the establishment of the level I trauma center revealed that patients in the latter group had an improved survival rate, compared to those in the former group. We attribute this finding to the integration of optimal trauma care, a team-based approach to patient care, and the 24-hour availability of surgery in the trauma center. In conclusion, this study revealed that the survival rate of patients with severe trauma was improved after establishment of a single level I trauma center.