Internal Iliac Artery Ligation with Pad Packing for Hemodynamic Unstable Open Comminuted Sacral Fracture
Article information
Abstract
A 52-year-old man experienced blunt trauma upon falling from a height of 40 m while trying to repair the elevator. The patient’s systolic blood pressure and hemoglobin levels were 60 mmHg and 7.0 g/dL, respectively, upon admission. A large volume of bloody discharge was observed in the open wound of the perianal area and sacrum. A computed tomography scan revealed an open comminuted sacral fracture with multiple contrast blushes. He underwent emergency laparotomy. Both internal iliac artery ligations were performed to control bleeding from the pelvis. Protective sigmoid loop colostomy was performed because of massive injury to the anal sphincters and pelvis. Pad packing was performed for a sacral open wound and perineal wound at the prone position. After resuscitation of massive transfusion, he underwent the second operation 2 days after the first operation. The pad was removed and the perineal and sacral open wounds were closed. After the damage-control surgery, he recovered safely. In this case, the hemodynamically unstable, open comminuted sacral fracture was treated safely by internal iliac artery ligation with pad packing.
INTRODUCTION
Despite many evolutions in the care of trauma patients, treatment modalities of hemodynamically unstable pelvic fractures have been the biggest challenge for trauma surgeons. Most recently, in a multicenter observational study by the American Association for the Surgery of Trauma (AAST), the mortality rate of patients with pelvic fractures admitted in shock was 32% [1]. To date, there have been several options to control bleeding of severe pelvic bone fractures such as pelvic binding, external fixation, angioembolization, and preperitoneal pad packing (PPP) [2]. However, pelvic fractures can induce massive bleeding, which arises from arterial injury, venous injury, and bone fractures. These various sources of bleeding contribute to the difficulty in controlling bleeding. There are limited reports of surgical ligation of the internal iliac artery [3]. We report a case with a hemodynamically unstable, open comminuted sacral fracture, which was treated by both internal iliac artery ligation and pad packing.
CASE REPORT
A 52-year-old man was transferred to our emergency room (ER) via another hospital after falling from a height of 40 m while trying to repair the elevator. At the previous hospital, he underwent cardiopulmonary resuscitation for several seconds. Upon arrival, his systolic blood pressure was 60 mmHg; heart rate, 110 beats per minute; respiration rate, 28 times per minute; and body temperature, 36°C. He had no history of hypertension, diabetes, or other medical conditions. A large amount of bloody discharge was observed in his perianal area and his perianal wound was packed with gauze to control bleeding. At the time of admission, he received blood transfusion immediately. He received 10 units of packed red blood cells (PRBCs) and 9 units of fresh frozen plasma (FFP) in the ER. After resuscitation by blood and crystalloids, a computed tomography (CT) scan was performed to evaluate the bleeding focus. The CT scan showed multiple contrast extravasation in the pelvis (Fig. 1) and most of the body of the sacrum was comminuted (Fig. 2). An emergency operation was performed to control bleeding of the pelvis. In the lithotomy position, we identified massive hemorrhage in the pelvic cavity and perirectal area. The levator muscle and other sphincter muscles were widely destroyed. We performed both internal iliac artery ligation (Fig. 3) and protective diverting colostomy of the sigmoid colon. We also performed packing in the pelvis via the perianal wound for damage control surgery. After changing to the prone position, we found a large defect in the sacrum (Fig. 4). We also performed pad packing of the sacral avulsion wound. He received 12 units of PRBCs, 4 units of FFP, and 10 units of platelet concentrates (PCs). The patient was admitted to the intensive care unit (ICU) and received massive transfusion 24 hours postoperatively (PRBC 8 units, FFP 11 units, PC 18 units). Two days postoperatively, his vital signs stabilized and the second operation was performed. Additional bleeder ligation was performed and all pads were removed with wound closure. He underwent extubation 3 days postoperatively. He was administrated antibiotics for the treatment of osteomyelitis. He developed a wound infection and underwent several surgical drainage procedures and negative pressure wound therapy (NPWT). After infection control, he underwent internal fixation of the sacrum and symphysis pubis diastasis. He recovered well and was discharged 7 months postoperatively. The anal manometry performed in the outpatient department showed fecal incontinence. Therefore, colostomy repair could not be performed.
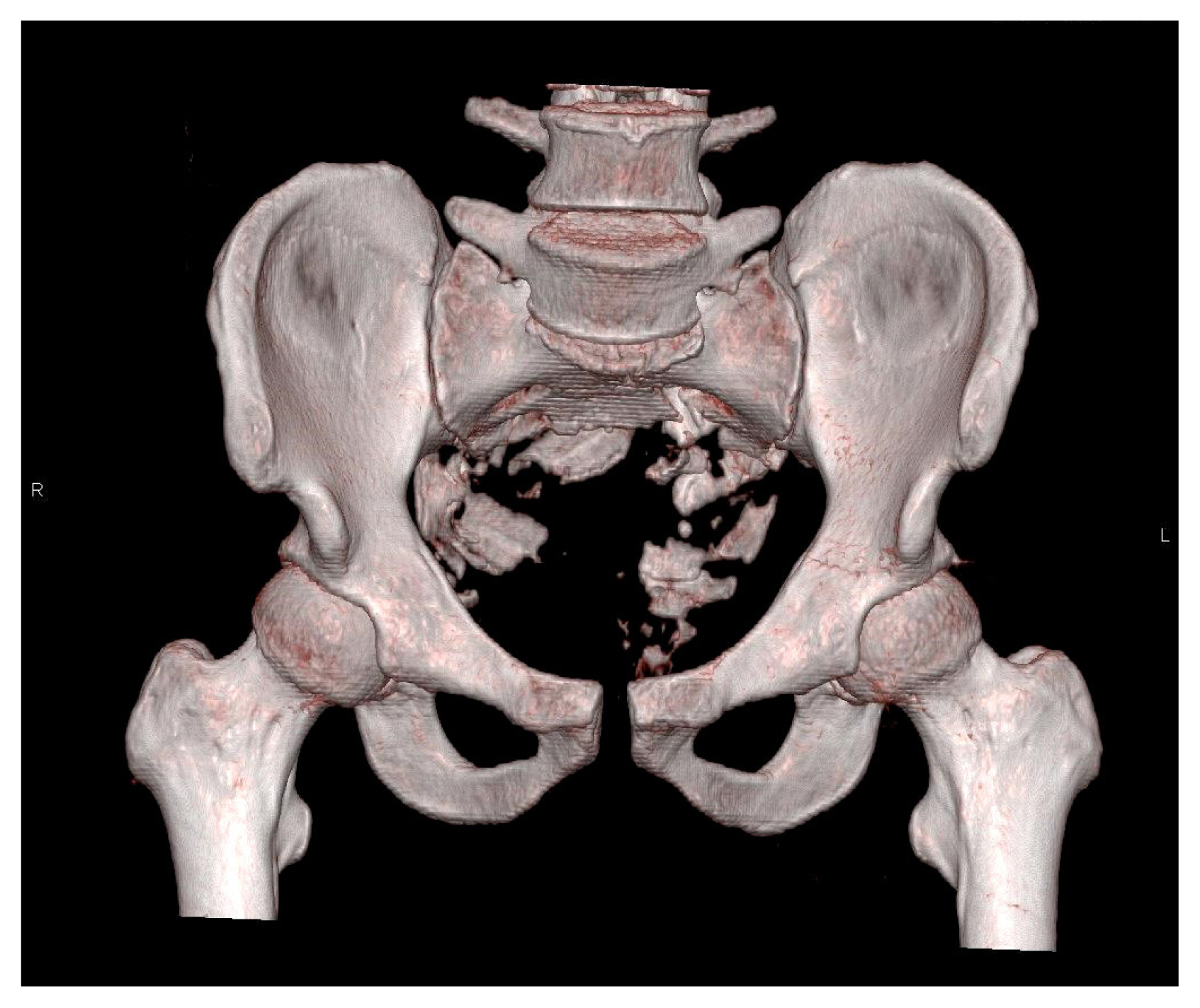
3-dimensional computed tomography of the pelvis (reconstructed image) showing a comminuted sacral fracture.
DISCUSSION
Pelvic exsanguination remains a lethal injury in trauma field. Recently, a new algorithm for management of pelvic fractures with hemodynamic instability was reported by the Western Trauma Association Critical Decisions in Trauma including pelvic stabilization, PPP, angioembolization, and resuscitative endovascular balloon occlusion of the aorta (REBOA) as treatment modalities [2]. However, there is a lack of evidence addressing surgical ligation of the bilateral internal iliac arteries and this issue was not mentioned in the algorithm. Nowadays, pelvic stabilization, angioembolization, and PPP are widely used as treatment modalities for unstable pelvic fractures since the establishment of a regional trauma center in South Korea [4]. However, bilateral internal iliac artery ligation is not popular worldwide or in South Korea. In the present case, bleeding control following pelvic examination was performed successfully and the patient recovered.
Historically, angioembolization was performed in all patients with hemodynamically unstable pelvic fractures. However, PPP was introduced as an alternative option [5]. Pelvic packing was first described 23 years ago in European literature [6]. Recently, PPP has been regarded as a useful option for pelvic hemorrhage in the United States, even though as a standard option, it remains controversial [2]. PPP aims to compress venous and bone bleeding by the tamponade effect [5]. Therefore, the bony structure of the pelvis must be intact to achieve the tamponade effect. In the present case, approximately over 80% of the sacrum was destroyed and successful PPP could not be expected.
Although the increased risk of subsequent ischemic sequelae after internal iliac artery embolization [7,8], no large studies exist. In a series of surgical ligation of the internal iliac artery, DuBose et al. [3] reported no ischemic sequelae during hospitalization. In this study, there was no ischemic complication.
There is limited literature addressing internal iliac artery ligation in hemodynamically unstable pelvic fractures. In a retrospective study of 28 patients with massive bleeding after pelvic fracture who underwent bilateral internal iliac artery ligation accompanying pad packing, DuBose et al. reported 10 survivors and 11 mortalities excluding those who died because of a severe brain injury [3]. The authors suggest that internal iliac artery ligation may be useful when the patient will not survive until angiography. The PPP technique has one limitation, in that it cannot control arterial bleeding sufficiently. Therefore, in general, a patient with ongoing bleeding after pelvic packing necessitates an angiography [5]. Surgical ligation of the internal iliac artery may be a reasonable option for a patient with profound pelvic bleeding. In the present study, because of the large defect of bone and soft tissue with severe hypotension, there is no chance to proceed to the angiography room. Recently, some trauma centers have hybrid rooms for the simultaneous performance of surgery and angiography, and this would help trauma surgeons treat severe pelvic bleeding.
In conclusion, massive pelvic bleeding with a large defect in the sacrum was treated safely by surgical ligation of the bilateral internal iliac arteries. Bilateral internal iliac artery ligation may be an alternative option if PPP or angioembolization is not available.


