Articles
- Page Path
- HOME > J Trauma Inj > Volume 30(4); 2017 > Article
-
Case Report
Proximal Tibia Fracture after Proximal Tibia Autograft Harvest - Jin-Kak Kim, M.D.1, Jong-Hyeop Song, M.D.1, Kyungbum Lee, M.D.2, Jae-Woo Cho, M.D.1, Ki-Ho Moon, M.D.1, Do-Hyun Yeo, M.D.1, Beom-Soo Kim, M.D.1, Jong-Keon Oh, M.D., Ph.D.1
-
Journal of Trauma and Injury 2017;30(4):247-252.
DOI: https://doi.org/10.20408/jti.2017.30.4.247
Published online: December 30, 2017
- 5,917 Views
- 57 Download
- 1 Crossref
1Department of Orthopaedic Surgery, Guro Hospital, Korea University College of Medicine, Seoul, Korea
2Department of General Surgery, Guro Hospital, Korea University College of Medicine, Seoul, Korea
- Correspondence to: Jong-Keon Oh, M.D., Ph.D., Department of Orthopaedic Surgery, Guro Hospital, Korea University College of Medicine, 148 Gurodong-ro, Guro-gu, Seoul 08308, Korea, Tel: +82-2-2626-3088, Fax: +82-2-851-3111, E-mail: jkoh@korea.ac.kr
• Received: August 29, 2017 • Revised: October 18, 2017 • Accepted: October 22, 2017
Copyright © 2017 The Korean Society of Trauma
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Bone-grafting procedures are common in orthopedic trauma surgeries. There are only few reports on the morbidity after proximal tibia harvesting. Here, we report an experience of complication after proximal tibia harvesting while treating subtrochanteric femoral osteomyelitis.
- Bone-grafting procedures are common in orthopedic surgeries for bone defects following trauma, arthrodesis, and nonunion of fractures. Autologous bone graft has biologic advantages over heterogeneous or synthetic bone substitutes because of a combination of osteogenic, osteoinductive, and osteoconductive properties. These properties have not yet been achieved in heterogeneous or synthetic bone substitutes. Several donor sites have been described for harvesting autologous cancellous bone such as the iliac crest, distal femur, proximal tibia, distal tibia, proximal humerus, olecranon, and distal radius [1]. There are some reports on donor site morbidity after iliac bone graft harvesting but only very few after proximal tibia harvesting [2,3]. Here, we report an experience of complication after proximal tibia harvesting while treating subtrochanteric femoral osteomyelitis.
INTRODUCTION
- A 55-year-old female visited our institute for the treatment of infected nonunion of subtrochanteric femoral fracture. The patient did not have any other comorbidity, except for obesity. Her body mass index was 38.14 kg/m2.
- She underwent multiple surgeries for the subtrochanteric femoral fracture at a local hospital, which resulted in non-union of the fracture. Furthermore, intraoperative samples for bacterial cultures were positive for methicillin-resistant staphylococcus aureus (Fig. 1)
- We removed the previously placed broken plate and debrided the infected tissue. Then, we placed a plate for temporary fixation and inserted a cement rod with cement spacer loaded with antibiotics. The 3.5 plate is not enough to maintain the fracture deformity when used alone; however, the intramedullary cement rod and spacer added stability until the next surgery (Fig. 2). Vancomycin was injected via intravenous for six weeks consulting to department of infectious disease. We set concentration to target for therapeutic drug monitoring of vancomycin.
- After three weeks from 1st surgery, we converted the temporary fixative to definite femoral nail (Fig. 3). During each of the procedures, we performed microbiological culture investigations during debridement and post-debridement. The post-debridement culture negative results let know us that the debridement was adequate.
- During six months of follow up in the outpatient department, her levels of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were not normalized, even though the intraoperative cultures were negative. Usually, we use bone grafts three months postoperatively after ESR and CRP have normalized, however, we could not do so in this case. There were no signs of infection such as fever, local warmth, redness, or tenderness. Additionally, we consulted the department of infectious diseases to identify the focus, which they could not. Therefore, we decided to perform debridement again. At that time, we changed all internal fixatives and inserted cement spacer with antibiotics. The tissue cultures were negative again.
- Six months later, we performed bone grafting even though ESR/CRP had not fully normalized. We could not wait for longer because she had been walking with a crutch and partial weight bearing for almost four years. Fortunately, a rheumatologist gave a diagnosis for her seropositive rheumatoid arthritis, which affect level of ESR and CRP. The total size of the bone defect was 91 mm in the subtrochanteric area. For this huge defect, we had to harvest the cancellous bones from the anterior superior iliac spine (ASIS) and bilateral proximal tibia. The other parts of ASIS were already used before. We had a choice of bilateral posterior superior iliac spine, but we thought it was not enough amounts for defects. We could add allograft bone chips or bone substitutes. But we wanted to avoid the chance of infection again even though it is rare. By creating a window at Gerdy’s tubercle, we obtained the cancellous bones with curettes from the metaphysis of the proximal tibias. The curettage was performed parallel to inferiorly but did not violate the medial cortex. The defect after harvesting did not require additional grafts. We obtained 44 g of cancellous bone from the right proximal tibia, and 31 g from the left proximal tibia. We also obtained 20 g from the left ASIS. Bone grafting was performed in the subtrochanteric femoral defect (Fig. 4). Postoperatively, the patient was placed in bilateral lower extremity splints and instructed to not bear weight till postoperative 6 weeks. For her left leg, we planned to permit her tolerable partial weight bearing from 6 weeks. And for her right leg, we planned to permit after 3 months because of grafted site used to consolidate from 3 months.
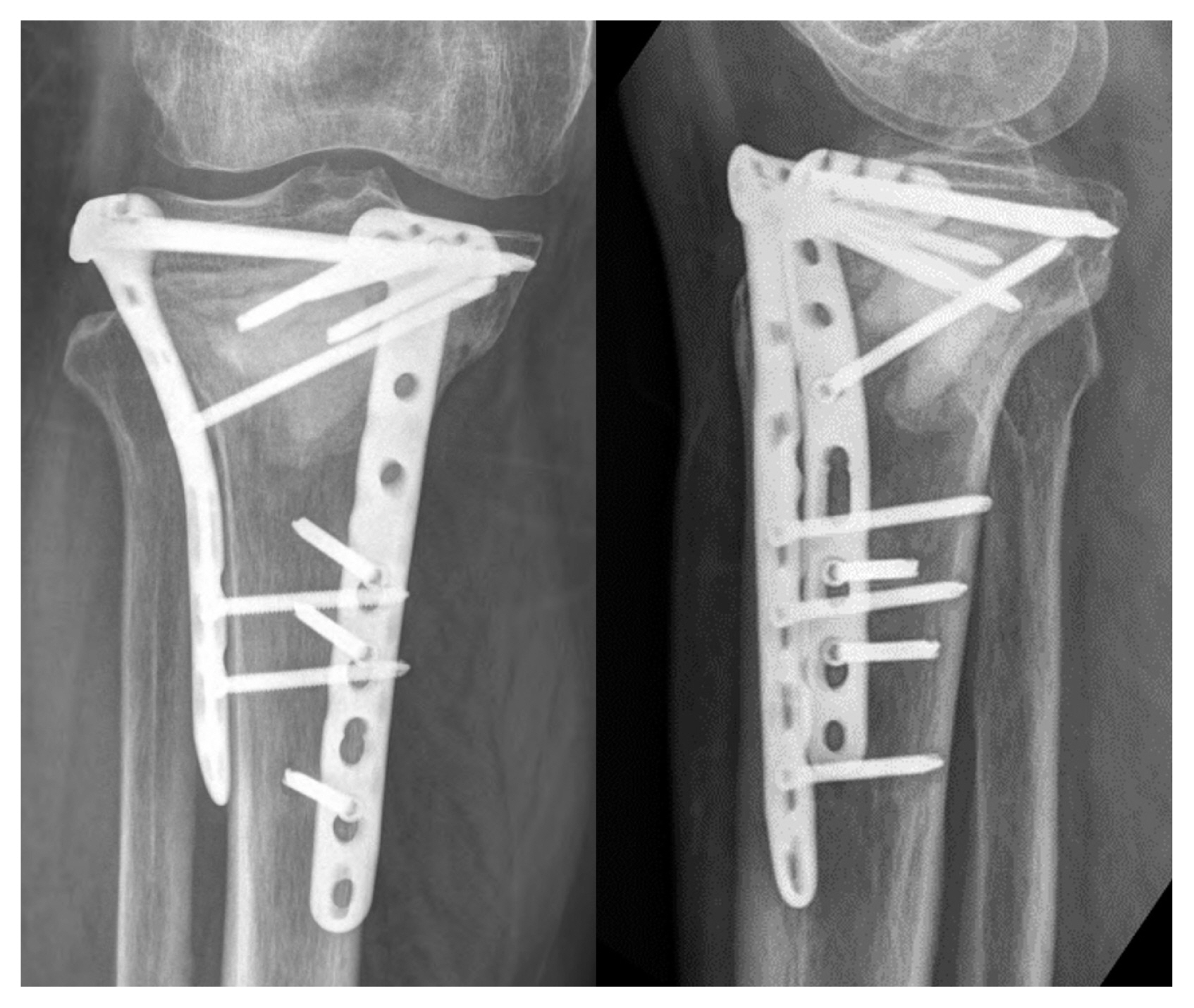
- On outpatient follow up two weeks later, her thigh pain was negligible but she complained of severe right knee pain. The radiographs showed cortical disruption from the medial to the lateral proximal metaphysis. However, there were no intra articular extensions noted on computed tomography (Fig. 5). Although the time of the new fracture was unclear, it happened postoperatively because there was no fracture line in the immediate radiographs. She did not bear weight but her pain aggravated since three days after the surgery.
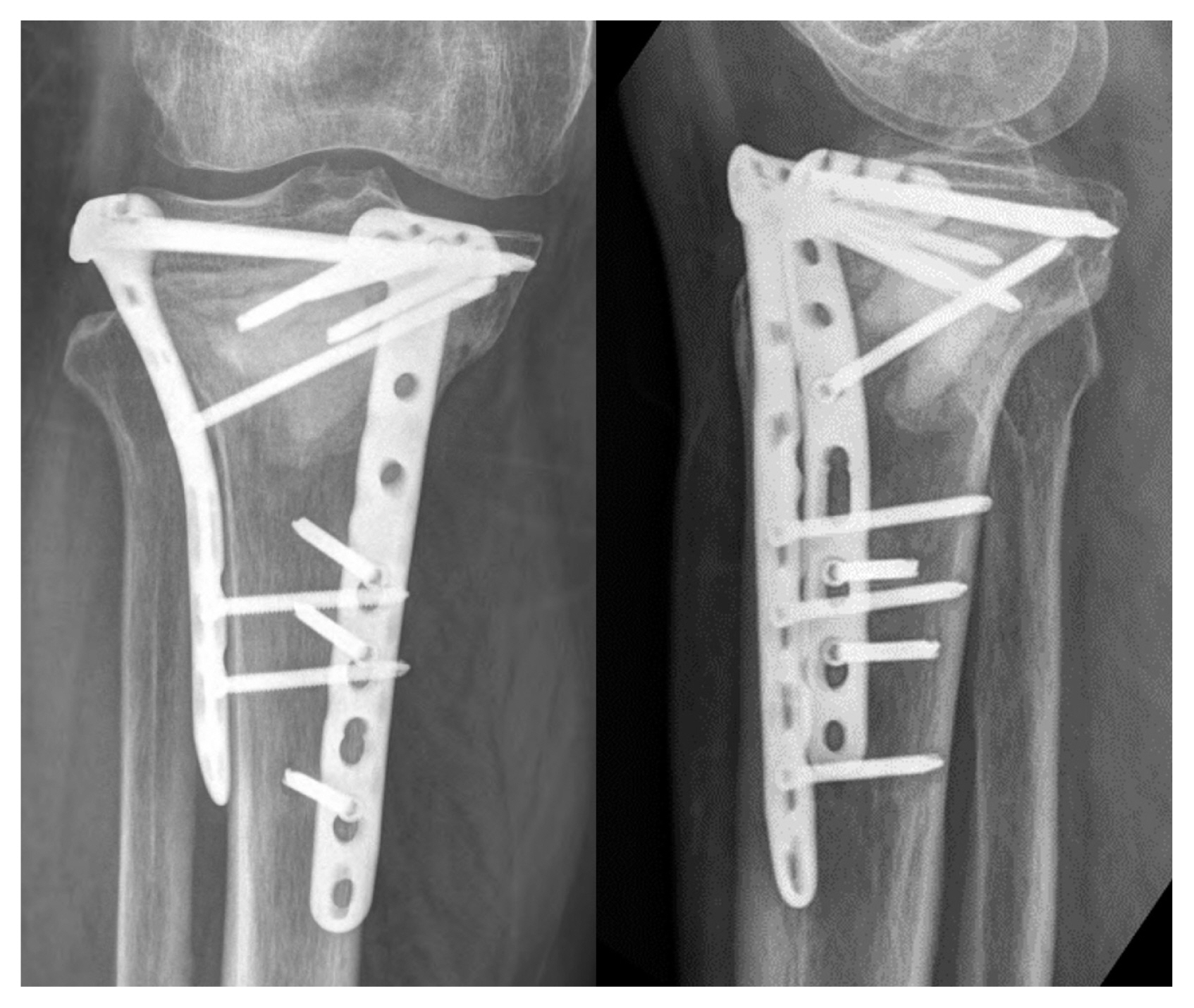
- Open reduction and internal fixation was performed using a 3.5 lateral proximal tibia plate and an additional medial plate was used. The bone graft substitute PRO-DENS™ (combination of calcium sulfate with calcium phosphate, WRIGHT Medical Technology, Inc., Arlington, TN, USA) was used to fill the defects (Fig. 6). After 9 months fracture was united well.
CASE REPORT
- Autologous cancellous bone graft has many benefits over allograft such as lower risk of immunologic complications and a combination of biologic properties. Anterior iliac crest is one of the standard harvest sites of autologous cancellous bone. However, donor site morbidity following harvesting of bone graft from the ilium has been reported. Many studies have reported that the iliac crest is associated with a relatively high morbidity. The rate of major complications that resolve with intervention, including neurologic injury, vascular injury, deep infection, large hematoma, bowel herniation, ureteral injury, and fracture and pelvic instability are reported to range from 2.5% to 39%. The rate of minor complications that resolve without intervention such as persistent donor site pain, seromas, cosmetic defects, and temporary paresthesia range from 10 to 40% [4–6].
- Due to the relatively high rate of complications with iliac crest bone grafts, other harvesting sites have gained popularity such as distal femur, proximal tibia, distal tibia, and local surgical site grafts. Of these, proximal tibia is relatively preferred over others because proximal tibia harvest site is near the surgical site within the same sterile drape usually and it can be under controlled with a tourniquet. Therefore, a graft may be obtained from the ipsilateral limb without re-draping. Additionally, a similar amount of bone graft may be obtained compared to the iliac crest. The reported volume of harvested graft from the proximal tibia is up to 30 cm3 [7].
- Most complications of harvesting proximal tibia are minor. Geideman et al. [7] reported only four minor complications in 155 patients who underwent a foot and ankle procedure utilizing the ipsilateral proximal tibia as the donor site for autologous bone grafts. There was one postoperative hematoma that resolved over time and three were transient complaints of pain at the donor site greater than those at the operative site. Their patients were maintained as non-weight bearing for at least six weeks. The complication rate was only 2.5%. O’Keeffe et al. [8] reported a complication rate of 1.3% in 206 patients with 230 proximal tibial bone graft harvests (3 of 230). Patients were non-weight bearing for a minimum of six weeks. The complications were hematoma, tibial eminence fracture, and superficial surgical site infections. Tibial eminence fractures were not insufficiency fractures extending the tibia plateau. Alt et al. [9] reported that in 54 patients who underwent proximal tibial bone grafting with immediate weight bearing that the complication rate was 1.9%. Only one patient of 54 patients developed a hematoma which resolved with evacuation.
- Fractures at the donor site are rare and have been reported by craniomaxillofacial surgeons predominantly. Kim et al. [10] reported four tibial bone fractures in 105 patients. Additionally, in two case series by Van Damme and Merkx [11], two of nine patients experienced fractures while playing tennis in one and running one week postoperatively in the other. Hughes and colleagues reported two fractures in 75 patients during exercising [12]. They have something in common with bone-harvesting technique. They made a bony window for harvesting just below the tibial tuberosity or just inferolateral to the tibial tuberosity, which is the level of upper diaphysis consisting of cortical bone and included higher stress [13]. Therefore, fracture had occurred during active exercising since excessive loads were permitted. To the best of our knowledge, only one case is similar to this case. Michael et al. [14] reported one case of proximal tibial fracture with proximal tibia graft due to foot and ankle surgery.
- We tried to understand the reasons underlying a fracture. The patient in this case was obese and she had walked with crutches with partial weight bearing for almost four years. That could have led to disuse osteoporosis, which can lead to easy fractures by low energy trauma. We thought when she make an only sitting position, fracture has occur. The amount of bone graft harvesting is also an important factor. It is still unclear how much amount of cancellous bone is safe to be removed. Additionally, the management of the defect after harvesting, such as backfilling with bone graft substitute is unclear. Alt et al. [15] showed that decancellated proximal tibia was no more likely to fracture than intact tibia by loading stress in eight cadavers. Further mechanical studies would helpful in solving this problem.
- Proximal tibia offers sufficient quantities of good quality cancellous bone. Even though morbidity after proximal tibia bone graft harvest is relatively rare, there is a chance of proximal tibia fractures. This case shows that the patient factors are very important. We recommend more cautious protection to minimize the risk of fractures in a high-risk patient.
DISCUSSION
Fig. 1(A) Initial radiograph showed subtrochanteric femoral fracture. It was an atypical femoral fracture. (B) Primary treatment was open reduction and nailing with cerclage wiring. A big incision (white arrow) was required. Biology of fracture site might be broken then. (C) Failure of implant 11 months postoperatively. There was no callus formation; however, progression of varus deformity of the proximal fragment was seen. (D) Revision treatment was plating. (E) However, after five months she underwent removal surgery again, because of infection. (F) Internal fixation with angled blade was tried but (G) failed again.
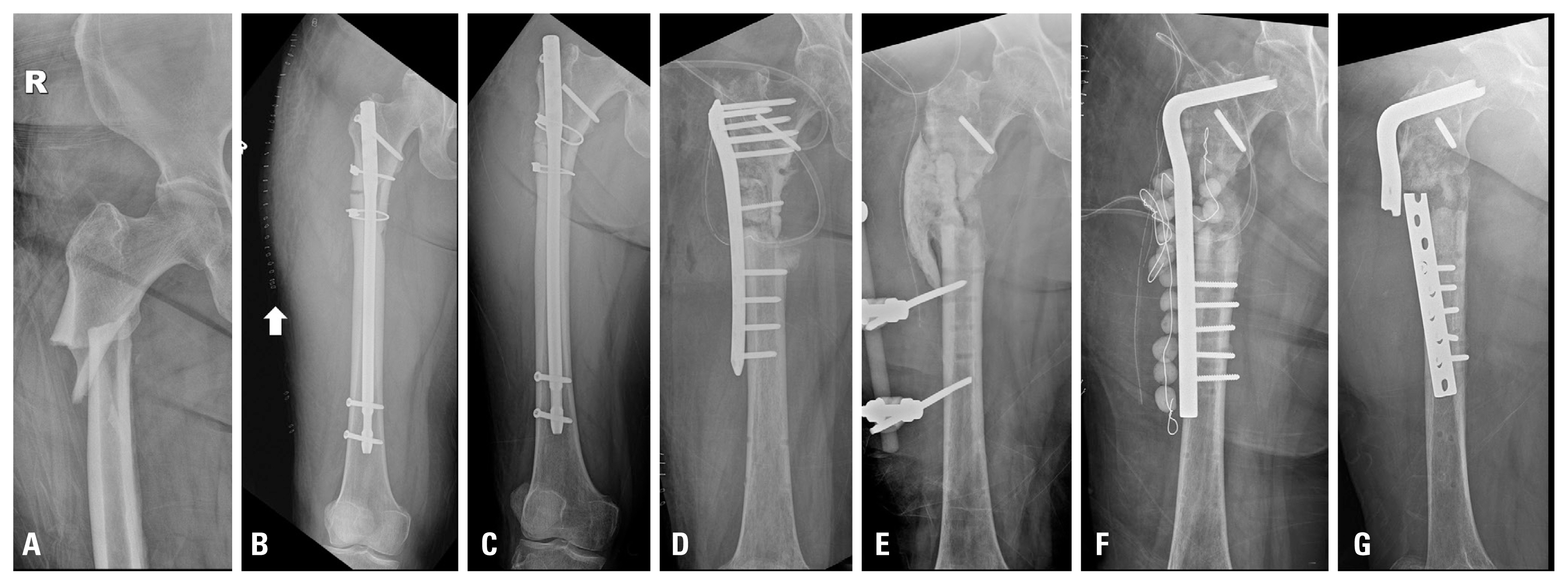
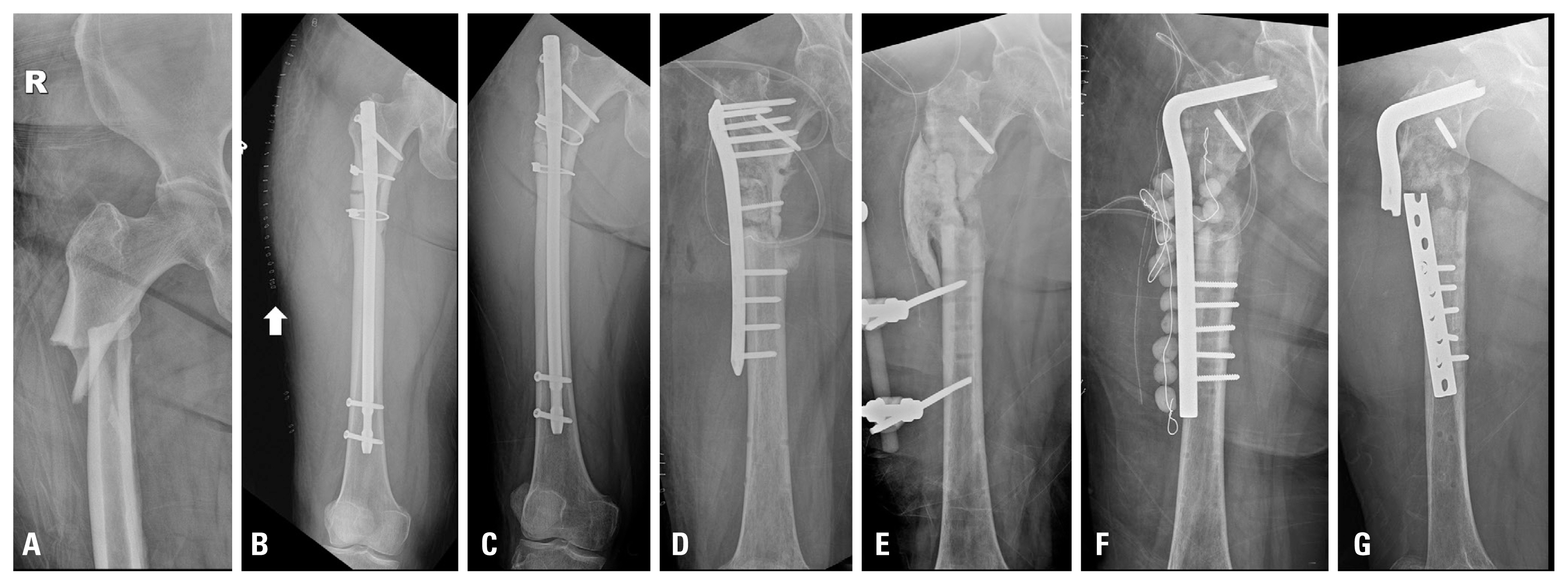
Fig. 2(A) We debrided the infected tissue including bone and soft tissues. (B) Two antibiotics-loaded cement rods were used. They were connected by a hinge. (C) Immediate post-operative radiograph was taken. We used plate for temporary fixation.


Fig. 3Conversion to definite fixation. We changed the previous plate for a new one in view of the infection.
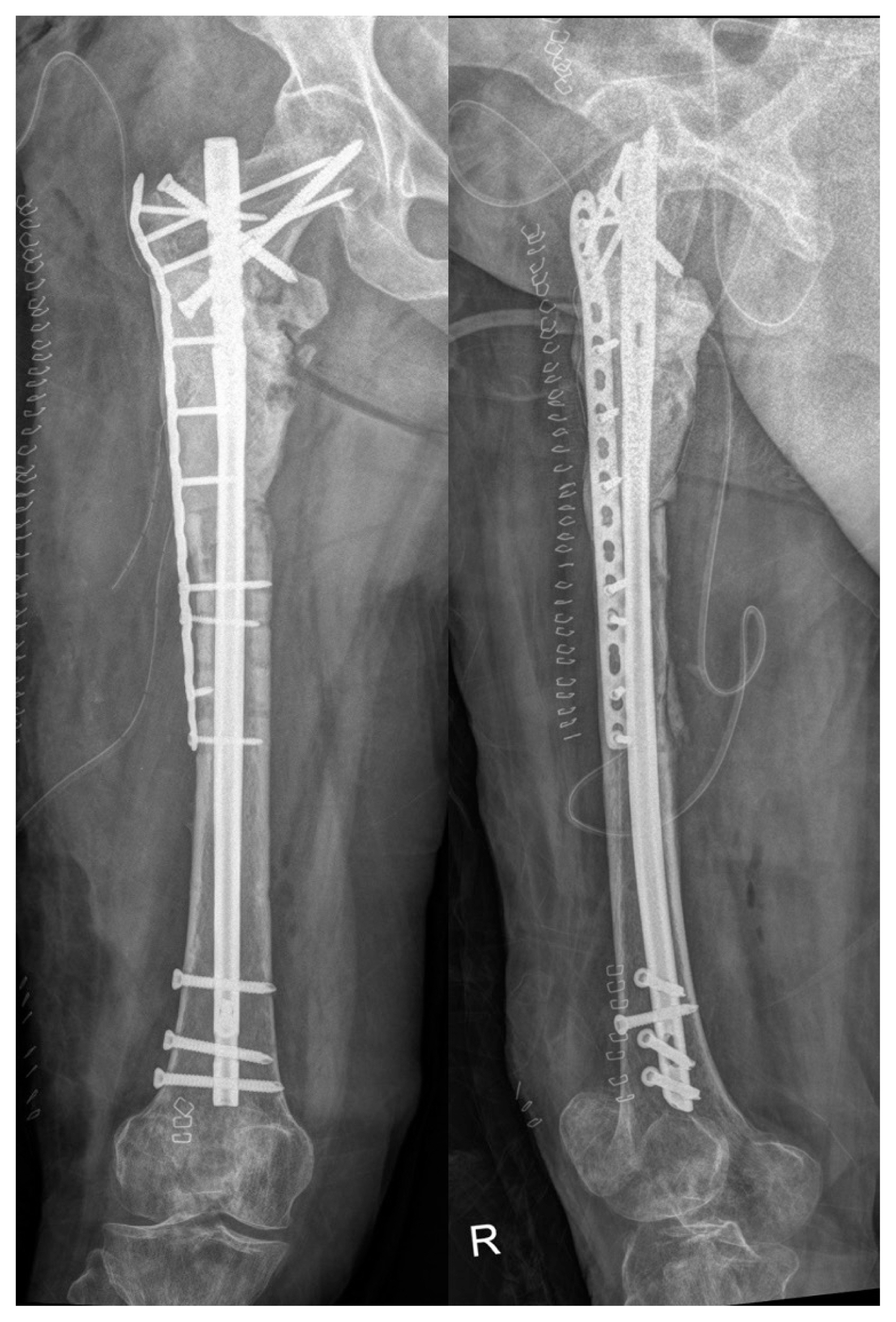
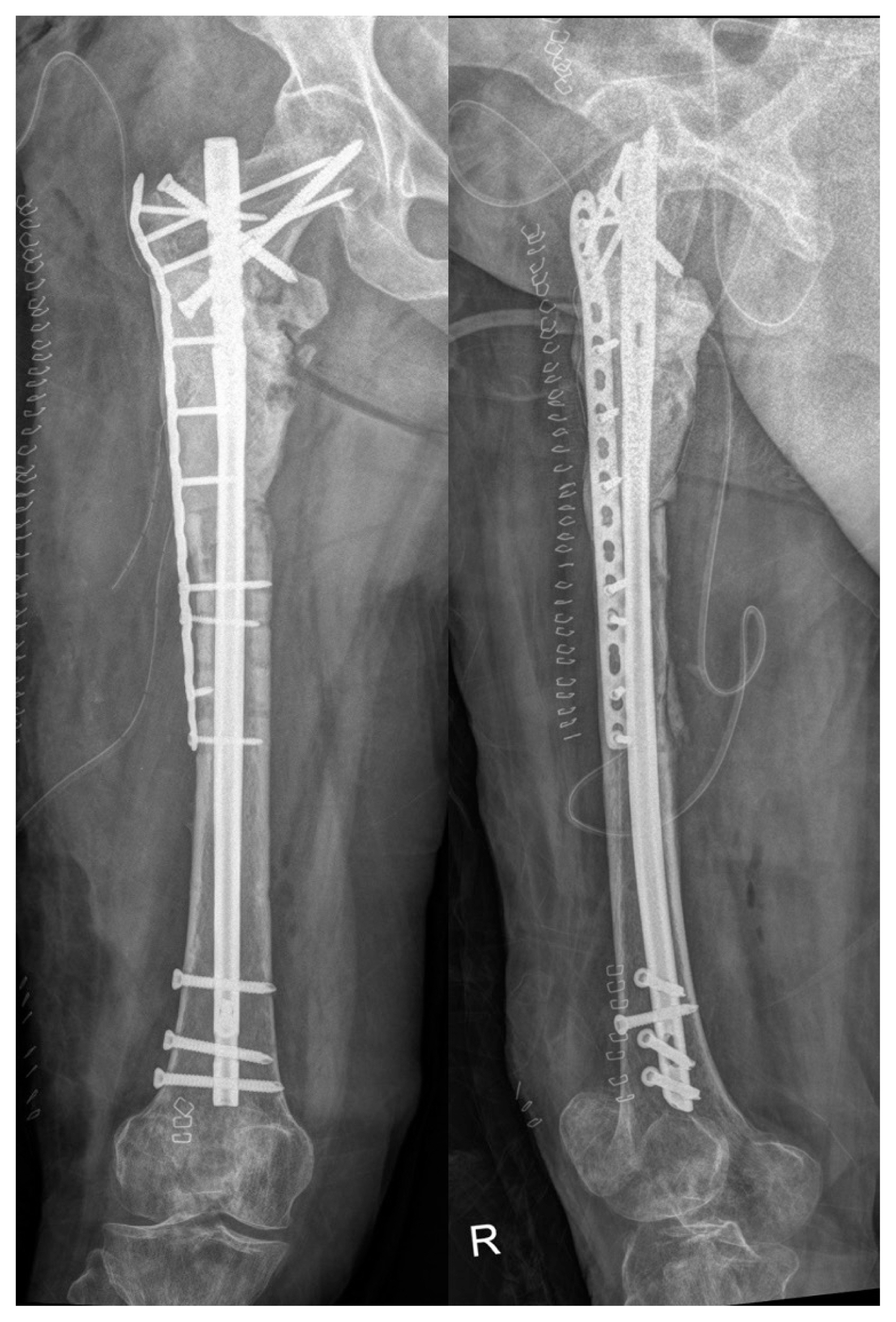
Fig. 4For a huge defect in the subtrochanteric area, we had to harvest from anterior superior iliac supine and bilateral proximal tibia.


Fig. 5At the outpatient follow-up two weeks later, she complained of right knee pain. Anteroposterior (A) and lateral (B) radiographs showed transverse cortical disruption of proximal tibia metaphysis. Additionally, coronal (C) and sagittal (D) cuts of computed tomography (CT) showed an extra-articular fracture. CT images show a huge vacant defect.


- 1. Egol KA, Nauth A, Lee M, Pape HC, Watson JT, Borrelli J Jr. Bone grafting: sourcing, timing, strategies, and alternatives. J Orthop Trauma 2015;29:Suppl 12S10–4.Article
- 2. Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma 1989;3:192–5.ArticlePubMed
- 3. Baumhauer J, Pinzur MS, Donahue R, Beasley W, DiGiovanni C. Site selection and pain outcome after autologous bone graft harvest. Foot Ankle Int 2014;35:104–7.ArticlePubMed
- 4. Russell JL, Block JE. Surgical harvesting of bone graft from the ilium: point of view. Med Hypotheses 2000;55:474–9.ArticlePubMed
- 5. Seiler JG 3rd, Johnson J. Iliac crest autogenous bone grafting: donor site complications. J South Orthop Assoc 2000;9:91–7.PubMed
- 6. Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury 2011;42:Suppl 2S3–15.Article
- 7. Geideman W, Early JS, Brodsky J. Clinical results of harvesting autogenous cancellous graft from the ipsilateral proximal tibia for use in foot and ankle surgery. Foot Ankle Int 2004;25:451–5.ArticlePubMed
- 8. O’Keeffe RM Jr, Riemer BL, Butterfield SL. Harvesting of autogenous cancellous bone graft from the proximal tibial metaphysis. A review of 230 cases. J Orthop Trauma 1991;5:469–74.ArticlePubMed
- 9. Alt V, Nawab A, Seligson D. Bone grafting from the proximal tibia. J Trauma 1999;47:555–7.ArticlePubMed
- 10. Kim IK, Cho HY, Pae SP, Jung BS, Cho HW, Seo JH. Tibial bone fractures occurring after medioproximal tibial bone grafts for oral and maxillofacial reconstruction. J Korean Assoc Oral Maxillofac Surg 2013;39:257–62.ArticlePubMedPMC
- 11. Van Damme P, Merkx MA. Fracture of the tibia after the modified tibial bone-graft-harvesting technique: a report of two cases. J Craniomaxillofac Surg 1988;26(Suppl 1):197.
- 12. Hughes CW, Revington PJ. The proximal tibia donor site in cleft alveolar bone grafting: experience of 75 consecutive cases. J Craniomaxillofac Surg 2002;30:12–6; discussion 17, ArticlePubMed
- 13. Xu C, Silder A, Zhang J, Reifman J, Unnikrishnan G. A cross-sectional study of the effects of load carriage on running characteristics and tibial mechanical stress: implications for stress-fracture injuries in women. BMC Musculoskelet Disord 2017;18:125, ArticlePubMedPMCPDF
- 14. Michael RJ, Ellis SJ, Roberts MM. Tibial plateau fracture following proximal tibia autograft harvest: case report. Foot Ankle Int 2012;33:1001–5.ArticlePubMed
- 15. Alt V, Meeder PJ, Seligson D, Schad A, Atienza C Jr. The proximal tibia metaphysis: a reliable donor site for bone grafting? Clin Orthop Relat Res 2003;(414):315–21.Article
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Novel Vacuum-Assisted Method for Harvesting Autologous Cancellous Bone Graft and Bone Marrow From the Proximal Tibial Metaphysis
Adam M. Lukasiewicz, Paul S. Bagi, Kristin E. Yu, Vineet Tyagi, Raymond J. Walls
Foot & Ankle Orthopaedics.2021; 6(1): 247301142098190. CrossRef
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite