Clinical Effects of Intra-Abdominal Pressure in Critically Ill Trauma Patients
Article information
Abstract
Purpose
There is increasing interest in intra-abdominal pressure (IAP) and intra-abdominal hypertension (IAH) in critically ill patients. This study investigated the effects and outcomes of elevated IAP in a trauma intensive care unit (ICU) population.
Methods
Eleven consecutive critically ill patients admitted to the trauma ICU at Pusan National University Hospital Regional Trauma Center were included in this study. IAP was measured every 8–12 hours (intermittently) for 72 hours. IAP was registered as mean and maximal values per day throughout the study period. IAH was defined as IAP ≥12 mmHg. Abdominal compartment syndrome was defined as IAP ≥20 mmHg plus ≥1 new organ failure. The main outcome measure was in-hospital mortality.
Results
According to maximal and mean IAP values, 10 (90.9%) of the patients developed IAH during the study period. The Sequential Organ Failure Assessment (SOFA) score was significantly higher in patients with IAP ≥20 mmHg than in those with IAP <20 mmHg (16 vs. 5, p=0.049). The hospital mortality rate was 27.3%. Patients with a maximum IAP ≥20 mmHg exhibited significantly higher hospital mortality rates (p=0.006). Non-survivors had higher maximum and mean IAP values.
Conclusions
Our results suggest that an elevated IAP may be associated with a poor prognosis in critically ill trauma patients.
INTRODUCTION
Increases in intra-abdominal pressure (IAP) affect the functions of organs both within and outside of the abdominal cavity, resulting in various clinical problems [1]. Therefore, there is a great deal of interest in the relationships between the multiple pathophysiological changes that occur in patients in the intensive care unit (ICU) and increases in IAP.
A continuous increase in IAP decreases the flow of blood supplied to the nervous system [2], circulatory organs [3], respiratory organs [4], gastrointestinal system [5], liver [6], and kidneys [7], and induces long-term functional deterioration. Intra-abdominal hypertension (IAH) and abdominal compartment syndrome (ACS), in which IAP increases, have been reported to increase patient mortality during ICU treatment, which may be related to severe organ damage [8,9].
However, few studies have addressed elevated IAP, such as high pressure in the abdominal cavity and ACS associated with intensive care treatment. This study investigated the clinical associations of elevated IAP and prognosis in patients admitted to trauma ICUs.
METHODS
Study population
From May 1 to December 31, 2017, a total of 1,452 patients were admitted to the emergency room of Pusan National University Hospital Regional Trauma Center due to traffic accidents, falls, and so forth. Of these, 951 patients were excluded because they were admitted to general wards, and 490 were excluded because intra-abdominal pressure (IAP) was not measured. Eleven subjects in whom IAP was measured were included in the study (Fig. 1). IAP was measured intermittently 2–3 times daily at 8–12 hours intervals from the first to the third day of hospitalization in the intensive care unit (ICU). In addition to assessing the effects of IAP, we also performed a retrospective chart review (using electronic records) for all patients. We collected demographic information, medical histories, clinical courses, acute physiology and chronic health evaluation (APACHE)-II scores, sequential organ failure assessment (SOFA) scores, and lengths of hospital and ICU stays. The shock index and injury severity scale (ISS) scores were calculated based on admission histories.
Measurement of IAP
IAP was measured using a modification of a method reported by Cheatham and Safcsac [10] using a urethral catheter in most patients and a commercial monitoring device (AbViser™; Contavec, Oklahoma City, OK, USA) in some patients. Measurement of IAP was performed by perfusing the urethral canal with physiological saline, adjusting the zero point at the position of the symphysis pubis, and then moving the urine drainage passage to the supine position. After locking and injecting 50 mL normal saline into the bladder, the pressure was measured while opening the urine drainage passage. IAP was measured intermittently 2–3 times per day, and the mean and maximum IAP values were recorded.
High IAP and ACS were diagnosed according to the definition of the World Society of Abdominal Compartment Syndrome [11], i.e., continuous or repetitive increase in IAP to ≥12 mmHg, and classified as grade I (12–15 mmHg), grade II (16–20 mmHg), grade III (21–25 mmHg), or grade IV (≥25 mmHg). ACS was defined as IAP ≥20 mmHg accompanied by multiple organ dysfunction. Patients with IAP ≥20 mmHg but no organ failure were classified as having high IAP, but not ACS, based on the above definition.
Our Institutional Review Board waived the need for informed patient consent because we used only existing materials and documents. Data were collected and processed anonymously; patients were entitled to refuse to participate at any time without any adverse consequences.
Statistical analyses
Statistical analyses were performed using SPSS ver. 18.0 for Windows (SPSS Inc., Chicago, IL, USA) and STATA ver. 14.1 (Stata Corp., College Station, TX, USA). Continuous variables were analyzed using the Mann-Whitney U test and Fisher’s exact test, and are expressed as the median (interquartile range). In all analyses, p<0.05 was taken to indicate statistical significance.
RESULTS
Patient characteristics
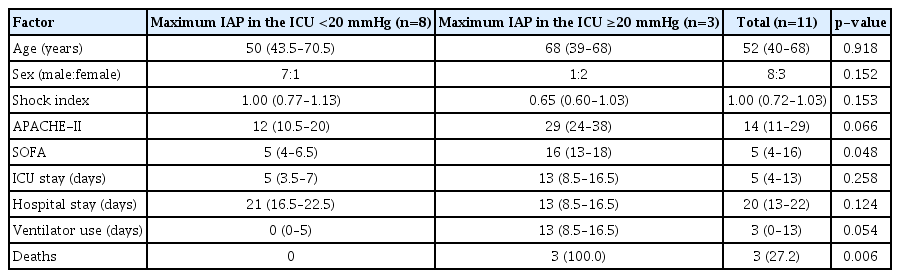
Table 1 lists the clinical features of the patients. The study population of 11 patients consisted of eight men and three women. The median age and ISS score were 52 years (40–68) and 25 (16–32), respectively. Five patients (45.5%) suffered a car accident, two (18.2%) a fall, two (18.2%) a pedestrian injury, one (9%) a motorcycle accident, and one (9%) an agricultural injury. The most commonly injured intra-abdominal organ was the liver (45.5%) (Table 1). Other abdominal injuries included liver contusions, small bowel and/or colonic injuries, and kidney and spleen injuries (Table 1). Five patients underwent abdominal surgery (Table 1). The APACHE-II score at the time of admission was 14 points (11–29), and the SOFA score was 5 points (4–16). The mean ICU stay was 5 days (4–13), and the mean total hospital stay was 20 days (13–22).
IAP and clinical course
The mean and maximum IAP values at admission were 14.4 mmHg (11.3–17.8) and 17 mmHg (13–20), respectively. The respective values in the ICU were 14.5 mmHg (13.5–19.5) and 18 mmHg (15–24) mmHg (Table 1). Based on both the maximum and mean IAP, 10 patients exhibited IAH (90.9%). Two patients (18.2%) had severely high IAP of grade III or higher (using the mean IAP as the reference). Three patients (27.3%) exhibited IAH of grade III or higher when the maximum IAP served as the reference (Table 1). Three patients died (27.3%): one of hemorrhagic shock, one of multi-organ failure, and one of severe sepsis (Table 1).
Relationship between the maximum IAP and clinical factors
Three patients (27.3%) exhibited a maximum ICU IAP ≥20 mmHg (grade III or higher). The median age was 68 years in those with IAP of grade III or higher and 50 years in those with IAP of less that grade III, but the difference was not statistically significant (p=0.918). The shock index (0.65 vs. 1.00, p=0.153), APACHE-II score (29 vs. 12, p=0.066), and total length of hospital stay (13 days vs. 21 days, p=0.124) were not significantly different between the groups. The ICU stay was longer (by 8 days) in the group with IAP of grade III or higher than in the IAP of less than grade III group, but the difference was not statistically significant (p=0.258) (Table 2).
However, the SOFA score was significantly higher in the group with IAP ≥20 mmHg than in the group with IAP <20 mmHg (16 vs. 5, p=0.049). High-grade IAP was significantly associated with more in-hospital mortality rates (p=0.006) (Table 2). In addition, the mean IAP measured in the ICU was higher in the group that died than survived (24 vs. 14 mmHg, p=0.006), and the maximum IAP exhibited a similar tendency (27 vs. 16.5 mmHg, p=0.014) (Fig. 2).
DISCUSSION
High pressure in the abdominal cavity has attracted a great deal of attention as a potential causative factor of several complications in both surgical and internal medicine ICUs. The types of high pressure within the abdominal cavity and ACS are primary IAH/ACS, which occur in connection with abdominal or pelvic injury or surgery; secondary IAH/ACS, which is caused by sepsis, capillary leakage, burn injuries, and so forth; and recurrent IAH/ACS that occur recurrently despite surgical intervention and other treatments [11]. In this study, all 11 patients in whom IAH occurred had primary IAH following trauma.
In 2004, Malbrain et al. [12] reported that the mean IAP in the ICU was 9.8±4.7 mmHg, and that high IAP and ACS had prevalence rates of 50.5% and 8.2%, respectively. In a follow-up survey conducted in 2005, the mean pressure in the abdominal cavity was 10.0±4.8 mmHg, and the prevalence rates of high IAP and ACS were 32.1% and 4.2%, respectively [9]. In the present study, both the mean and maximum IAP values were higher than in previous reports, and the prevalence rate of high IAP was also higher than in previous studies. These differences were thought to have been due to differences in the study populations between studies. The subjects in the present study were trauma patients who were hospitalized in the ICU, and therefore it was likely that they would show high IAP. In addition, we cannot exclude the possible effects of differences in precision and reproducibility of surgical techniques for measuring abdominal pressure between studies [13]. In this study, stress was measured using multiple testers during the study period, and measurement errors occurred between testers. These factors were likely at least partially responsible for the higher mean IAP compared with previous investigations.
A significant association between high IAP and mortality in the ICU was previously reported [9], and our results confirmed this tendency. High pressure in the abdominal cavity was significantly associated with prognosis, with higher pressure associated with poorer prognosis (Table 2).
In this study, the mean IAP at the time of hospitalization and on admission to the ICU were 14.4 mmHg (11.3–17.8) and 14.5 mmHg (13.5–19.5), respectively. The maximum IAP on hospitalization and admission to the ICU were 17 mmHg (13–20) and 18 mmHg (15–24), respectively. Although there is no consensus regarding whether the mean or maximum IAP should be used for diagnosing high pressure in the abdominal cavity, the prevalence of peritoneal hypertension was 90.9% in our study regardless of whether the mean or maximum IAP was used to this end. However, when the maximum IAP was used as the reference, high-grade maximal IAP (≥20 mmHg) was significantly associated with a higher in-hospital mortality rate (Table 2). Therefore, from a clinical perspective, we suggest that it may be useful to employ the maximum IAP to diagnose IAH or ACS.
Some researchers have suggested that abdominal perfusion pressure (APP) is a superior predictor of patient survival than is IAP [14]. Particularly in patients who undergo mechanical ventilation, the decrease in peritoneal perfusion pressure is significantly related to mortality rate, as the cardiac output decreases due to the increase in airway pressure as a result of mechanical ventilation, and under such conditions, peritoneal perfusion pressure is thought to cause perfusion injury of several intraperitoneal organs such as the gastrointestinal tract, kidneys, and liver [13,15,16]. On the other hand, it has also been reported that there is no relationship between peritoneal perfusion pressure and prognosis [11]. In the present study, we could not determine the relationship between APP and mortality as we did not measure APP.
Although our results indicate a close relation between IAP and prognosis, our study had limitations due to the small study population and the retrospective nature of the research. Further prospective studies in larger populations are required to clarify the clinical significance of IAP.
CONCLUSION
In conclusion, we found that an increase in IAP measured in the trauma ICU and the occurrence of IAH affected prognosis. Our results suggest that IAP can be used to predict the prognosis of critically ill trauma patients, although further studies in larger populations are needed.
ACKNOWLEDGEMENTS
This work was supported by clinical research grant from Pusan National University Hospital in 2019.