Life-Threatening Necrotizing Fasciitis of the Posterior Neck
Article information
Abstract
Necrotizing fasciitis is an infection of the subcutaneous tissue that results in destruction of the fascia and is disproportionately common in patients with chronic liver disease or diabetes. Necrotizing fasciitis of the head and neck is rare, but has a high fatality rate. A 50-year-old man with a past medical history of diabetes reported a chief complaint of a wound in the posterior neck due to trauma. The wound had grown and was accompanied by pus and redness, and the patient had a fever. When the patient was referred to department of plastic & reconstructive surgery, the sternocleidomastoid muscle, semispinalis capitis muscle, splenius capitis muscle, and trapezius muscles were exposed, and the size of the defect was about 25×20 cm. Dead tissue resection was performed before negative-pressure wound therapy, followed by a split-thickness skin graft (STSG). After a 2-week course of aseptic dressing post-STSG, the patient recovered completely. No postoperative complications were observed for 1 year. Necrotizing fasciitis is a life-threatening, rapidly spreading infection, requiring early diagnosis and active surgical treatment. In addition, broad-spectrum antibiotics are required due to the variety of types of causative bacteria. Broad necrotizing fasciitis of the posterior neck is rare, but can quickly progress into a life-threatening stage.
INTRODUCTION
Necrotizing fasciitis is rarer in the cervical region than in other parts of the body, and its location makes it possible for an infection to spread rapidly to the main blood vessels of the head, neck, and chest, as well as the mediastinum. Cervical necrotizing fasciitis can therefore cause life-threatening complications faster than other types of necrotizing fasciitis [1]. For this reason, an early diagnosis, an immediate antibiotic regimen, and surgical treatment are critical in the reducing mortality rate.
We report, along with a literature review, a case of complete recovery from broad necrotizing fasciitis of the posterior neck using antibiotic treatment, dead tissue resection, negative-pressure wound therapy (NPWT), and split-thickness skin graft (STSG), consecutively.
CASE REPORT
A 50-year-old man with a past medical history of diabetes reported a wound in the posterior neck due to trauma that occurred 2 weeks prior to the medical visit. Due to symptom exacerbation and the presence of a pus-filled mass, the patient was referred by an outside physician and was presented to the emergency room (ER) for possible surgery. Upon the ER visit, redness, swelling, and a warm sensation were observed throughout the posterior neck, with some necrotic parts. The patient complained of severe pain. Neck computed tomography showed a diffuse abscess cavity and gas in the posterior neck, and the muscle was intact (Fig. 1). The laboratory risk indicator for necrotizing fasciitis (LRINEC) is a scoring system derived from six routinely performed laboratory tests that is used initially to distinguish necrotizing fasciitis from other severe soft-tissue infections [2]. The laboratory results yielded a LRINEC score of 8, supporting the diagnosis of necrotizing fasciitis (Table 1). When the inner area of the necrotic tissue was observed, the muscle layer and subcutaneous layer were easily separated, which strongly suggested necrotizing fasciitis, so emergency surgery was indicated. The Department of Head and Neck Surgery and the Department of Neurosurgery proceeded with emergency surgery accompanied by radical debridement and moved the patient to the intensive care unit. Methicillin-resistant Staphylococcus aureus was the suspected pathogen specific to this wound culture. Vancomycin, in combination with an antibiotic with anaerobic coverage, was used along with the daily aseptic dressing. Upon presentation to department of plastic & reconstructive surgery, the sternocleidomastoid muscle, semispinalis capitis muscle, and trapezius muscle were exposed, and the size of the defect was 25×20 cm (Fig. 2). An additional dead tissue resection procedure was performed, followed by NPWT 2–3 times per week over the course of 4 weeks (Fig. 3). STSG was performed for the posterior neck wound, and 2 weeks later, the patient was discharged. Although the patient had slight discomfort when moving his neck 1 year after surgery, there was no limitation of range of motion or other complications (Fig. 4). The study was performed in accordance with the principles of the Declaration of Helsinki. The patient provided written informed consent for the publication and the use of his images.
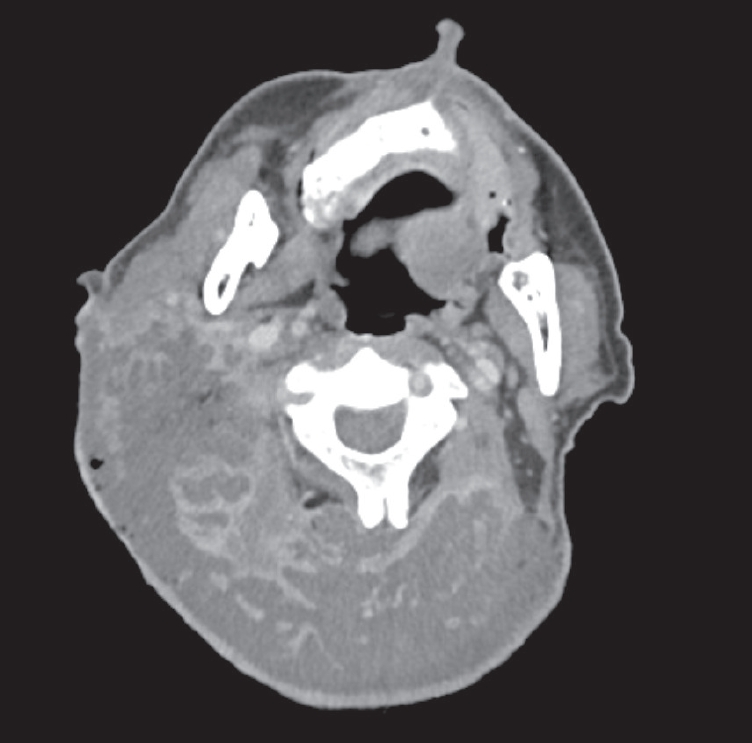
Neck computed tomography showing a diffused abscess cavity and gas in the posterior neck, with the muscle intact.
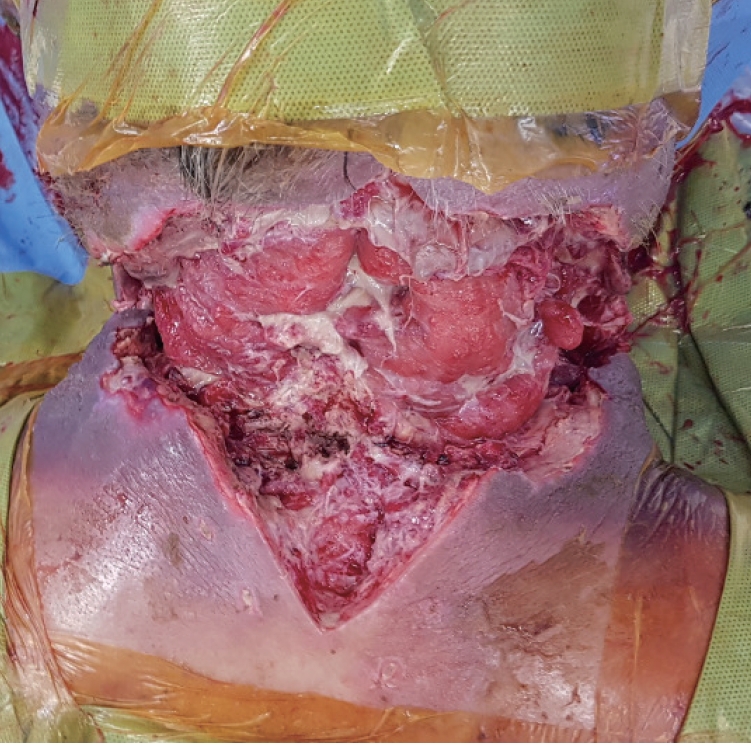
The sternocleidomastoid muscle, semispinalis capitis muscle, and trapezius muscle were exposed, and the defect measured 25×20 cm.
DISCUSSION
Necrotizing fasciitis, which is mainly caused by group A β-hemolytic Streptococcus, has a low occurrence rate. However, it causes rapid ischemia in soft tissue within fascia, leading to nonreciprocal damage and a high fatality rate if diagnosis and treatment are delayed. This disease occurs mainly in the lower extremities, as well as the perineal and abdominal regions. Its occurrence rate is relatively high in immunocompromised patients with underlying high-risk factors such as advanced age, chronic liver disease, and alcoholism [3]. External factors such as lacerations, insect bites, injections, and surgery-induced skin damage can cause necrotizing fasciitis in patients with no underlying diseases [4]. The fatality rate can be as high as 20% to 50%, and it is critical to perform immediate antibiotic treatment and surgery to reduce the risk of death [5]. Systematic toxicity can occur faster in cervical necrotizing fasciitis than in any other type of necrotizing fasciitis, possibly causing fatal complications due to direct transmission of the bacteria [1]. Necrotizing fasciitis should be carefully differentiated from skin infection caused by an abscess, which is limited to the dermis and subcutaneous space and manifests as a painful, fluctuant, erythematous nodule, with or without surrounding cellulitis [6]. Wie et al. [1] reported a case of anterior neck necrotizing fasciitis, involving rapid instability of vital signs, a broad necrotized tissue resection and subsequent drainage, and a topical flap and skin graft that enabled a complete recovery. The patient in the current study also had unstable vital signs and received a broad-spectrum antibiotic with aseptic dressing after emergency debridement. The skin and soft tissue defect of the posterior neck measured approximately 25×20 cm, and NPWT was the choice of treatment, taking into account the possibility of donor site morbidity if flap surgery is performed in a patient with diabetes mellitus. NPWT has been reported to be useful for infected wounds, including necrotizing fasciitis, in several studies [7]. Shin and Choi [8] reported using NPWT post-debridement for a case of broad necrotizing fasciitis that developed after abdominal liposuction.
The authors experienced a case of posterior neck necrotizing fasciitis that was treated sequentially with dead tissue resection, broad-spectrum antibiotic treatment, NPWT, and STSG, with satisfactory results. Necrotizing fasciitis requires early diagnosis and surgical procedures, in combination with proper antibiotic treatment, in order to lower the fatality rate. Therefore, rapid treatment is necessary upon the suspicion of the disease. It may be difficult to perform flap surgery for a broad skin and soft tissue defect if the patient has multiple underlying diseases and unstable vital signs. Although it may not be applicable in all cases, a skin graft after NPWT can be used as an alternative. Necrotizing fasciitis in the posterior neck is rare and may be more lethal than necrotizing fasciitis in other parts of the body. Thus, this case is reported along with a literature review.
Acknowledgements
This study was supported by the research funds of Dong-A University.


