Bilateral foot drop caused by T12 infectious spondylitis after vertebroplasty: a case report
Article information
Abstract
The most common cause of foot drop is lumbar degenerative disc herniation, particularly at L4/5. We present a rare case of spinal cord injury accompanied by a thoracolumbar lesion that presented with bilateral foot drop. A 69-year-old male patient presented with sudden-onset severe bilateral leg pain and bilateral foot drop. Radiologic findings revealed T12 spondylitis compressing the conus medullaris. He had undergone vertebroplasty for a T12 compression fracture after a fall 6 months before. A physical examination showed bilateral foot drop, paresthesia of both L5 dermatomes, increased deep tendon reflex, and a positive Babinski sign. An acute bilateral L5 root lesion and a conus medullaris lesion were suspected based on electromyography. A surgical procedure was done for decompression and reconstruction. After the operation, bilateral lower extremity muscle strength recovered to a good grade from the trace grade, and the patient could walk without a cane. The current case is a very rare report of bilateral foot drop associated with T12 infectious spondylitis after vertebroplasty. It is essential to keep in mind that lesions of the thoracolumbar junction can cause atypical neurological symptoms. Furthermore, understanding the conus medullaris and nerve root anatomy at the T12–L1 level will be helpful for treating patients with atypical neurological symptoms.
INTRODUCTION
Foot drop is defined as a significant weakness of ankle and toe dorsiflexion caused by weakness or paralysis of the tibialis anterior muscles. The most common cause of foot drop is an impairment of the peroneal nerve or L5 nerve root. However, bilateral foot drop is rare in peripheral lesions, and central nervous lesions should be considered in such cases [1–3].
The thoracolumbar junction is anatomically composed of the spinal cord, epiconus, conus medullaris, and cauda equina. Therefore, lesions in the thoracolumbar spine (T12–L1) can also present upper motor neuron signs and nonspecific neurological symptoms of the lower extremities [3]. In addition, middle column fracture can cause significant compression of the spinal canal, leading to substantial neurological symptoms, including foot drop.
Infectious spondylitis after vertebroplasty has been reported in rare instances [4]. Severe neurological deficits are also rare in cases of spondylitis induced by spine fractures, with a prevalence of 3% [5]. Herein, we report a very rare case of bilateral foot drop caused by a T12 vertebral compression fracture accompanied by infectious spondylitis after vertebroplasty and suggest a possible mechanism.
CASE REPORT
A 69-year-old male patient was admitted with complaints of gait disturbance, paralysis of both legs, and leg pain for 2 weeks. Six months prior to admission, he had undergone vertebroplasty for T12 compression fracture, after he fell on his buttocks. On admission, he had no signs of infection such as fever, malaise, night sweat, or weight loss. He had been diagnosed with pulmonary tuberculosis 3 months before and was on antituberculosis drugs.
Neurological examination revealed severe leg pain (visual analogue scale, 7 points) and bilateral foot drop with upper motor neuron signs, including ankle clonus and the Babinski sign. Neurogenic bladder and bowel symptoms were also reported. Although bilateral foot drop was predominantly documented (motor grade, 1/5–2/5), knee flexion and ankle plantar flexion were mildly affected (motor grade, 3/5–4/5).
Computed tomography and magnetic resonance imaging revealed infectious spondylitis with abscess formation and bony destruction at the T12 vertebral body, resulting in severe compression of the conus medullaris. There was no lesion that could cause L5 radiculopathy at the L4–5 and L5–S1 levels (Figs. 1, 2). However, a bilateral L5 root lesion and conus medullaris lesion were revealed by electromyography (EMG).

(A) T2-weighted sagittal and (B) axial magnetic resonance imaging reveal a compression fracture at T12 with spinal cord compression. The L5–S1 disc is relatively preserved on the patient’s magnetic resonance imaging. The patient provided written informed consent for the publication of the research details and clinical images.
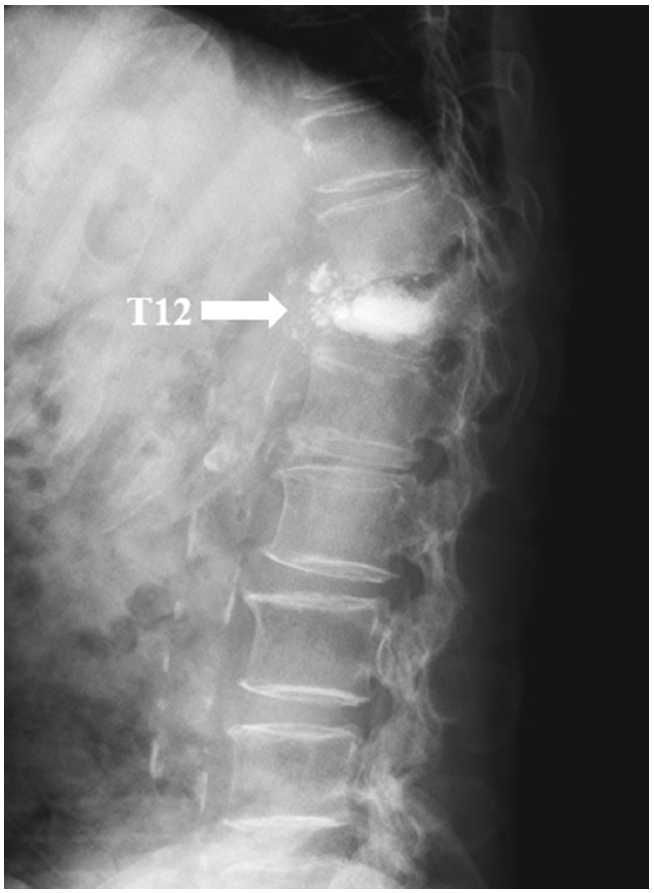
Plain radiograph reveals a compression fracture at T12 (arrow), at the level of the previous vertebroplasty. The patient provided written informed consent for the publication of the research details and clinical images.
Surgical resection of the bony fragment compressing the spinal cord was performed using a posterior approach. After pedicle screw fixation from T9 to L2, modified pedicle subtraction osteotomy was performed to decompress and correct the affected vertebrae. A mesh cage filled with autogenous bone was inserted between the lower end plate of T12 and the osteotomy surface of L1. After placement of an L2 laminar hook and rod, posterolateral bone grafting in the fixation region was performed with an autogenous bone graft (Fig. 3).
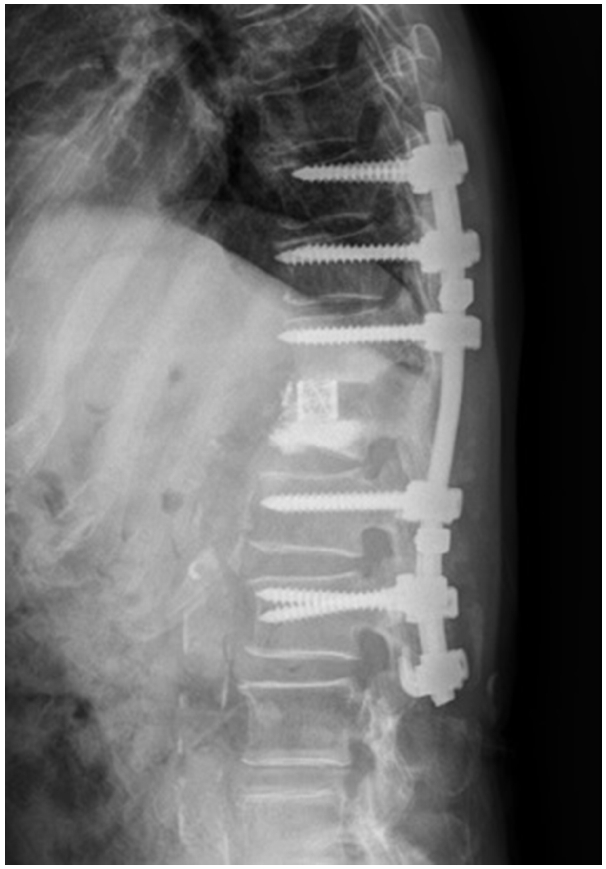
Modified pedicle subtraction osteotomy and pedicle screw insertion were performed for neural decompression and spinal stability. The patient provided written informed consent for the publication of the research details and clinical images.
Postoperatively, improvements were observed in radiating pain (visual analogue scale, 3 points) and motor weakness. Bilateral lower extremity muscle strength recovered to a good grade, and foot drop also improved immediately after surgery. The presence of a T12 fracture-induced bilateral L5 root lesion was verified.
In addition, for more quantitative measurements of preoperative and postoperative motor recovery, active range of motion (ROM) angles of ankle dorsiflexion during knee flexion and extension were measured (Fig. 4). Surface EMG was used to measure the percent reference voluntary contraction (%RVC) values of ankle dorsiflexion (Table 1). A remarkable increment in the %RVC of the bilateral tibialis anterior muscles was observed postoperatively. Consequently, we were able to objectively confirm not only manual muscle test results of ankle dorsiflexion, but also the postoperative improvement in active ROM and %RVC values.
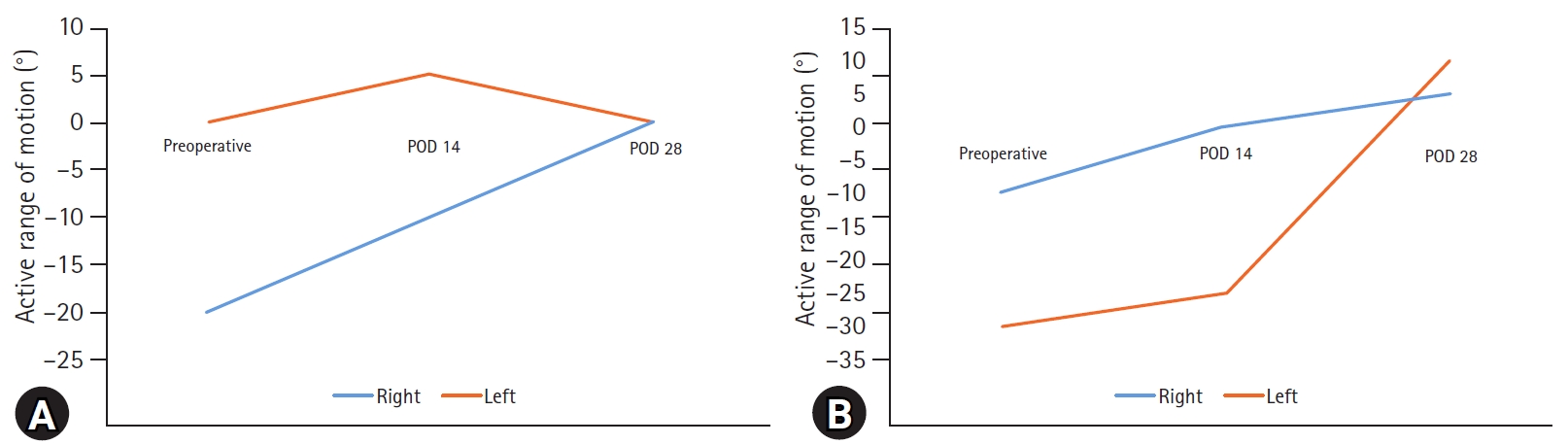
In order to obtain quantitative measurements of preoperative and postoperative motor recovery, active range of motion angles of ankle dorsiflexion during (A) knee extension and (B) flexion were measured. POD, postoperative day.

The percent reference voluntary contraction values of bilateral TA and GCM during ankle dorsiflexion
The causative pathogen was not identified in microbiological specimens, and al granuloma was not found in the biopsy sample. Empirical antibiotics and an antituberculosis regimen were administrated. On day 53, the patient was discharged with a good motor grade in both lower extremities, without bladder or bowel symptoms. The antituberculosis medication continued for 40 days.
DISCUSSION
The incidence of infectious spondylitis after percutaneous augmentation, including vertebroplasty, is low (0.46%), and the mean interval between the completion of augmentation and revision operation is 118.4 days [6]. In general, although severe back pain is a common symptom of infectious spondylitis [7,8], in our case, weakness due to cord compression first developed 164 days after vertebroplasty.
Neurological symptoms may vary according to the level of the lesion. Symptoms may manifest as paraplegia due to spinal cord compression, various sensory or motor deficits associated with cauda equina or root compression, and rectal or urinary incontinence [9]. The thoracolumbar junction (T12–L1), which is the site of cord termination, anatomically consists of the spinal cord, epiconus, conus medullaris, and cauda equina. A compressive lesion at the thoracolumbar junction causes various nonspecific neurological symptoms, including foot drop [3]. However, bilateral root paralysis is a rare pathologic condition.
Miwa et al. [3] reported that foot drop caused by a thoracolumbar spine lesion recovered much better than foot drop caused by a lumbar spine lesion. This suggests that the pathogenesis of paralysis in the 2 lesions may be different.
According to Wall et al. [10], the axial cross-section of T12–L1 shows that the spinal cord is surrounded by the L1 to L5 roots, and among these, the L5 ventral root is medially and the L1 ventral root is laterally located (Fig. 5). Based on this anatomy, we further verified how a compression fracture at the T12 level caused an L5 root lesion, subsequently leading to bilateral foot drop.
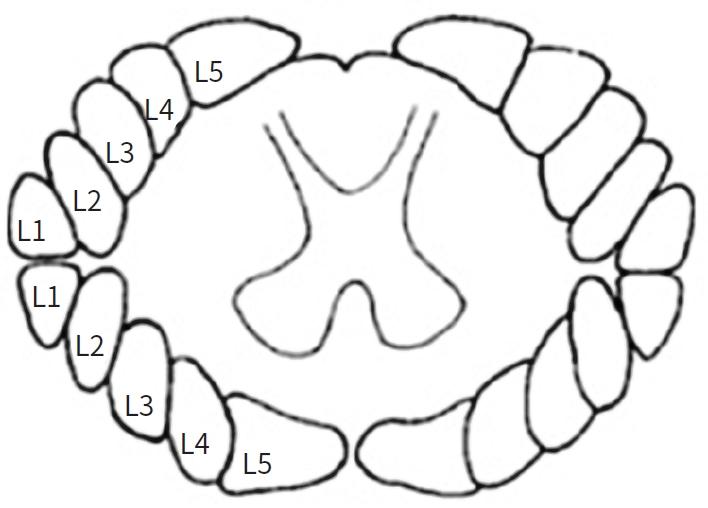
An axial cross-section of T12–L1 showing that the spinal cord is surrounded by the L5 root at L1, and among these, the L5 ventral root is medially and the L1 ventral root is laterally located. This explains how compression at the T12 level compresses both the L5 roots and leads to bilateral foot drop.
It has been reported that an L5 root lesion resulting from thoracolumbar spine fracture is anatomically possible [3,11], but this patient’s clinical presentation was very rare, as it was due to infectious spondylitis in a T12 compression fracture after vertebroplasty. To the best of our knowledge, no similar case has been reported before.
Moreover, by using a wireless EMG system (Delsys Inc., Boston, MA, USA) for motor recovery measurements, we were able to obtain more objective data. Notably, the recovery of the soleus and gastrocnemius muscles was differentiated by presenting active ROM angles of ankle dorsiflexion during knee extension and knee flexion. This aspect of the present case also bears some significance. As more cases are gathered in the future, further evaluation of motor recovery patterns is required.
In conclusion, it is essential to keep in mind that lesions of the thoracolumbar junction can present with atypical neurological symptoms, including bilateral foot drop. Understanding the conus medullaris and nerve root anatomy, as well as performing EMG, will be helpful in treating patients with atypical neurological symptoms.
Notes
Ethical statement
Informed consent was obtained from the patient.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
This work was supported by a clinical research grant from Pusan National University Hospital in 2021.
Author contributions
Conceptualization: KHN, YBS; Data curation: DHK; Formal analysis: YBS, DHK; Project administration: KHN; Visualization: DHK, YBS; Writing–original draft: DHK, KHN; Writing–review&editing: KHN, YBS, MJH, BCK, IHH.
All authors read and approved the final copy of the manuscript.
