Inhalation injury after a landmine explosion: a case report
Article information
Abstract
Blast injuries are divided into four classes, and inhalation injuries are a quaternary class of blast injuries. An inhalation injury can be critical to the patient due to the possibility of related complications, such as airway obstruction resulting from upper airway edema and pneumonia. Once diagnosed, an inhalation injury should be treated with early intubation, aerosol therapy, and antibiotics as soon as possible. We should suspect this injury in circumstances involving fire and especially bomb attacks in a military setting. Antipersonnel landmines designed to damage the soldier by amputating the leg can cause blast injuries, but their power is limited to the lower extremity. However, we found an inhalation injury in a victim whose leg had been amputated by an antipersonnel landmine. As soon as we suspected an inhalation injury, we intubated the patient to preserve his airway and started acetylcysteine/heparin aerosol therapy. The patient also was treated with proper antibiotics for right lower lung pneumonia that developed as a sequela of inhalation injury. We could extubate the patient without any complications such as airway obstruction on the third day of intensive care, after which the patient was transferred to the general ward for active rehabilitation. This report presents the first known case of inhalation injury due to a landmine explosion.
INTRODUCTION
Inhalation injuries, which can develop as a result of blast injuries, are very harmful because they cause airway obstruction, pneumonia, and acute lung injury [1]. Inhalation injuries consist of three subtypes: upper airway injuries caused by thermal heat, lower airway and lung parenchyme injuries caused by chemical irritants, and metabolic asphyxia caused by carbon monoxide and cyanide [2]. It is important for physicians to suspect inhalation injuries in cases of blast injuries; then, early management, including intubation or aerosol therapy, to prevent airway obstruction should be performed. Herein, we would like to present the case of a patient who had been injured by an antipersonnel landmine, and we want to share how we suspected and treated the inhalation injury of this patient starting in the trauma bay with early intubation and acetylcysteine/heparin aerosol therapy.
The study was approved by the Institutional Review Board of the Armed Forces Capital Hospital (No. 2022-01-003) and was in compliance with the Declaration of Helsinki. The patient provided written informed consent for publication of the research details and clinical images.
CASE REPORT
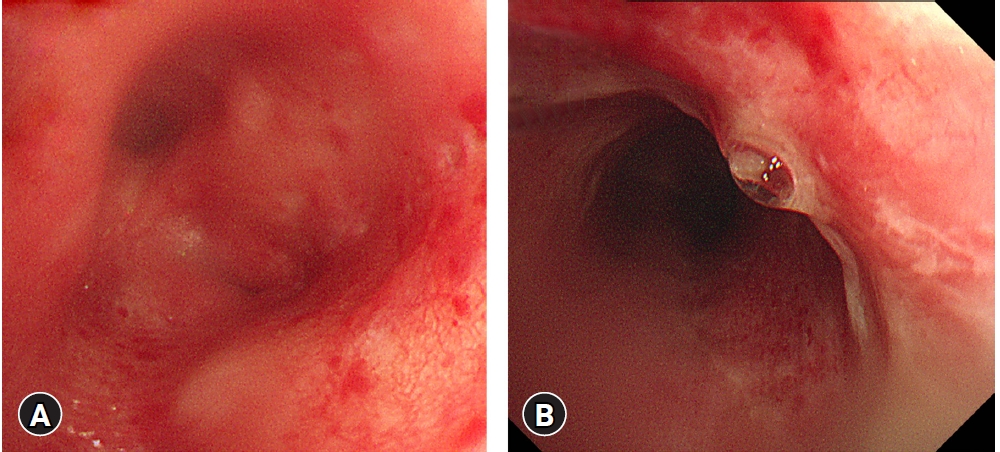
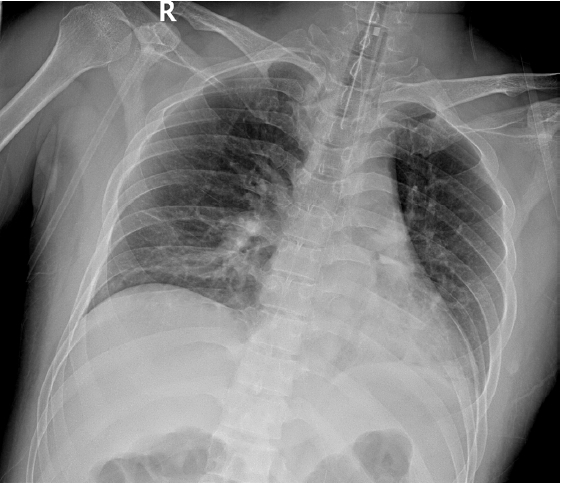
A previously healthy 39-year-old male sergeant was transferred to the trauma bay in Armed Forces Trauma Center due to a landmine injury. He was confirmed to have an amputation at the left distal tibia joint and left thumb tip due to a landmine blast injury (Fig. 1A, B). His thigh was tightened with a tourniquet by prehospital medical staff. The initial arterial blood pressure was 181/112 mmHg, the heart rate was 106 beats/min, the respiratory rate was 16 breaths/min, and the body temperature was 36℃. He had multiple burn injuries, especially on the left arm, bilateral legs, and face. Bilateral sub-conjunctival hemorrhage was confirmed (Fig. 1C). His incisor was slightly sooty. The bilateral lung sounds were clear, and the initial chest X-ray was normal. The initial arterial blood gas analysis confirmed no hypoxia or hypercapnia, with a lactate level of 1.1 mmol/L. He was intubated with video laryngoscopy for irritability and an emergent orthopedic operation was performed. Then, whole-body computed tomography was performed, and no specific injury was confirmed in the brain, chest, and abdomen. After the emergent operation was prepared, he was transferred to the operation room from the trauma bay. Because the amputated segment was not revivable and the distal tibia joint was very contaminated, the orthopedic surgeon decided to proceed with below-knee amputation and dress the amputation site and burn wound with a vacuum-assisted device. The thumb tip amputation was repaired primarily after massive irrigation and debridement. After an emergent operation, he was transferred to the intensive care unit. The day after surgery, follow-up bronchoscopy confirmed abrasions along the upper airway from the oral cavity to the upper trachea (Fig. 2), and a chest X-ray revealed increased opacity in the right lower lung field (Fig. 3). We then started heparin with acetylcysteine aerosol therapy, suspecting an inhalation burn. As Klebsiella pneumoniae and Pseudomonas aeruginosa were confirmed in tracheal culture, levofloxacin and piperacillin/tazobactam were administered. On the third hospital day, extubation was performed and follow-up laryngoscopy showed mild laryngeal edema and an oral cavity burn injury. During intensive care, as delirium and deep vein thrombosis developed, antipsychotics and low-molecular-weight heparin were administered. On the 19th hospital day, he was transferred to the general ward for active rehabilitation without any respiratory complications.
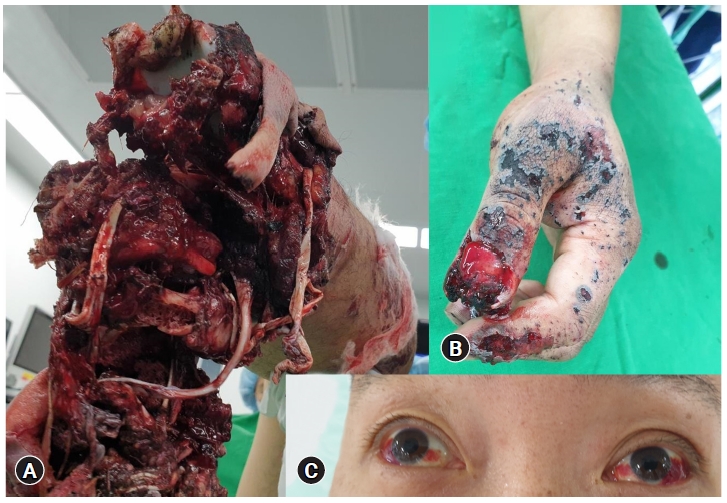
Multiple trauma wounds after landmine explosion.
(A) Amputated left leg and (B) left thumb tip. (C) Bilateral subconjunctival hemorrhage due to a landmine blast injury. The patient provided written informed consent for publication of the research details and clinical images.
DISCUSSION
Inhalation burn injuries are well-known to be quaternary blast injuries [3]. In this case, the patient’s leg was amputated as the primary injury, and he had burn injuries at multiple sites as quaternary injuries. We should suspect an inhalation injury if a patient has respiratory symptoms such as stridor, wheezing, difficulty breathing, smoke debris or burn around the face, and a sooty nose, especially, in situations related to fires. Inhalation injuries are classified into three subtypes according to the anatomic site: the upper airway, the lower airway and lung parenchyme, and metabolic asphyxiation [1]. Upper airway injuries are usually caused by thermal burns from heat transfer, lower airway and lung parenchymal injuries develop from chemical and particulate irritants, and metabolic asphyxia is due to carbon monoxide and cyanide. In this case, with confirmation of the injury in the larynx and upper airway, we suspected that the cause of the inhalation injury was a thermal burn from heat transfer. We did not consider antidotes for metabolic asphyxiation in this patient because the injury occurred in an open space where cyanide is usually not problematic [4].
Inhalation injury can lead to the development of severe airway obstruction. A steam or chemical injury from the supraglottic area to the tracheobronchial tree and lung cause constriction due to the inflammatory cascade. The most important aspect of treating inhalation injuries in trauma bay is airway management. Eckert et al. [5] reported that inhalation injury led to progressive airway symptoms within 12 hours and that the majority of symptoms occurred between 6 and 12 hours after injury. He and his colleagues argued that physicians should be ready for emergent airway management for at least 18 hours, even in blast injury patients with limited severity. To prevent progression of the obstruction, we can consider some medications such as aerosolized heparin, epinephrine, N-acetylcysteine, or beta-2 agonists [6]. In the present case, we used aerosolized heparin/N-acetylcysteine, including heparin 10,000 IU, which is known for its safety and absence of an effect on coagulation parameters [7].
In this case, as we intubated the patient immediately after he entered the trauma bay, he had no sequelae related to the airway. However, secondary airway and pulmonary injuries can occur up to 12 hours after a blast injury [5]. An inhalation injury is a predisposing factor for pneumonia, and the combination of an inhalation injury and pneumonia increases mortality [8]. Therefore, a regular culture study is important to choose the proper antibiotics, and we obtained a specimen from a bronchoscopic exam. Since the two most common bacteria in inhalation injury-related pneumonia are Klebsiella pneumoniae and Pseudomonas aeruginosa, as in this case [9], we recommend antibiotics that can cover Gram-negative strains (e.g., piperacillin/tazobactam).
Landmines are classified into antitank mines and antipersonnel mines, and injuries due to antipersonnel mines are divided into two patterns, according to whether they are caused by blast mines or fragmentation mines [10]. Blast mines usually have small explosions that only damage the lower extremity. Fragmentation mines are relatively less explosive, but cause damage at longer distances than blast mines through multiple fragmentation. We could not confirm the type of landmine in the present case; however, the injury resembled the blast mine amputation pattern. We thought the reason why secondary and tertiary injuries were not clearly observable was the amputation caused by the blast mine injury. However, there was a report that ocular injuries could occur even with a blast mine pattern [11]. This implies that an inhalation injury could also occur. In this case, we found not only a lower extremity injury, but also bilateral subconjunctival hemorrhage, which implied that the blast wave reached the level of the face. Therefore, we also must check the condition of the nose or oral cavity and suspect smoke inhalation in landmine blasts. In Korea, it is known that there are many landmines around the demilitarized zone. We may encounter victims of landmine-related injuries in the near future, and we should always be prepared for inhalation injuries caused by landmine blasts, as in this case.
Notes
Ethical statements
The study was approved by the Institutional Review Board of the Armed Forces Capital Hospital (No. 2022-01-003) and was in compliance with the Declaration of Helsinki. The patient provided written informed consent for publication of the research details and clinical images.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Author contributions
Conceptualization: HL; Data curation: WK; Formal analysis: HL; Methodology: all authors; Project administration: WK; Visualization: WK; Writing–original draft: WK; Writing–review & editing: all authors.
All authors read and approved the final manuscript.