Articles
- Page Path
- HOME > J Trauma Inj > Volume 34(2); 2021 > Article
-
Case Report
Celiac Artery Compression After a Spine Fracture, and Pericardium Rupture After Blunt Trauma: A Case Report from a Single Injury - Joongsuck Kim, M.D.1, Hyun Min Cho, M.D.1, Sung Hwan Kim, M.D.2, Seong Hoon Jung, M.D.3, Jeong Eun Sohn, M.D.3, Kwangmin Lee, M.D.3
-
Journal of Trauma and Injury 2021;34(2):130-135.
DOI: https://doi.org/10.20408/jti.2020.0053
Published online: June 10, 2021
- 3,047 Views
- 68 Download
1Department of Trauma Surgery, Cheju Halla General Hospital, Jeju, Korea
2Department of Neurosurgery, Cheju Halla General Hospital, Jeju, Korea
3Department of Anesthesiology and Pain Medicine, Cheju Halla General Hospital, Jeju, Korea
- Correspondence to Hyun Min Cho, M.D. Department of Trauma Surgery, Cheju Halla General Hospital, 65 Doryeong-ro, Jeju 63127, Korea Tel: +82-64-740-5000 Fax: +82-64-743-3110 E-mail: csking1@daum.net
• Received: September 16, 2020 • Revised: November 7, 2020 • Accepted: November 16, 2020
Copyright © 2021 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Celiac artery compression is a rare condition in which the celiac artery is compressed by the median arcuate ligament. Case reports of compression after trauma are hard to find. Blunt traumatic pericardium rupture is also a rare condition. We report a single patient who experienced both rare conditions from a single blunt injury. An 18-year-old woman was brought to the trauma center after a fatal motorcycle accident, in which she was a passenger. The driver was found dead. Her vital signs were stable, but she complained of mild abdominal pain, chest wall pain, and severe back pain. There were no definite neurologic deficits. Her initial computed tomography (CT) scan revealed multiple rib fractures, moderate lung contusions with hemothorax, moderate liver injury, and severe lumbar spine fracture and dislocation. She was brought to the angiography room to check for active bleeding in the liver, which was not apparent. However, the guide wire was not able to pass through the celiac trunk. A review of the initial CT revealed kinking of the celiac trunk, which was assumed to be due to altered anatomy of the median arcuate ligament caused by spine fractures. Immediate fixation of the vertebrae was performed. During recovery, her hemothorax remained loculated. Suspecting empyema, thoracotomy was performed at 3 weeks after admission, revealing organized hematoma without pus formation, as well as rupture of the pericardium, which was immediately sutured, and decortication was carried out. Five weeks after admission, she had recovered without complications and was discharged home.
- Celiac artery compression is a rare condition in which the celiac artery is compressed by the median arcuate ligament. It is a rare entity, first reported by Lipshutz in 1917, and described by Dunbar in 1965; thus, it is also known as Dunbar syndrome [1]. With its low incidence of two per 100,000 population, case reports of compression after trauma are hard to find, especially related to blunt trauma. Blunt traumatic rupture of the pericardium is also a rare condition [2], with an estimated incidence of 0.37%. Both conditions may go unnoticed or become fatal, and therefore require a thorough diagnosis and surgical repair. We report a single patient who experienced both rare conditions from a single blunt injury.
INTRODUCTION
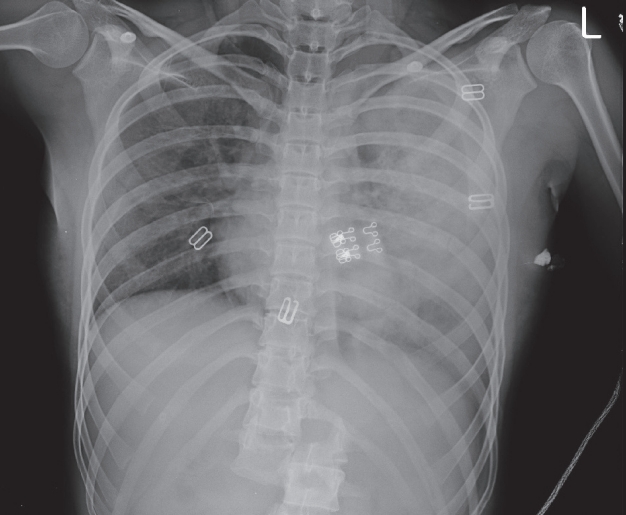
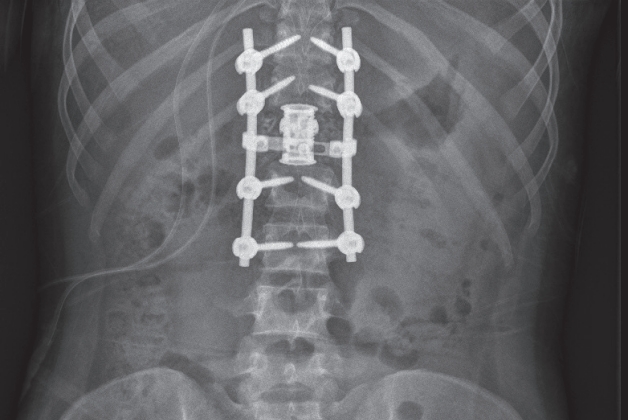
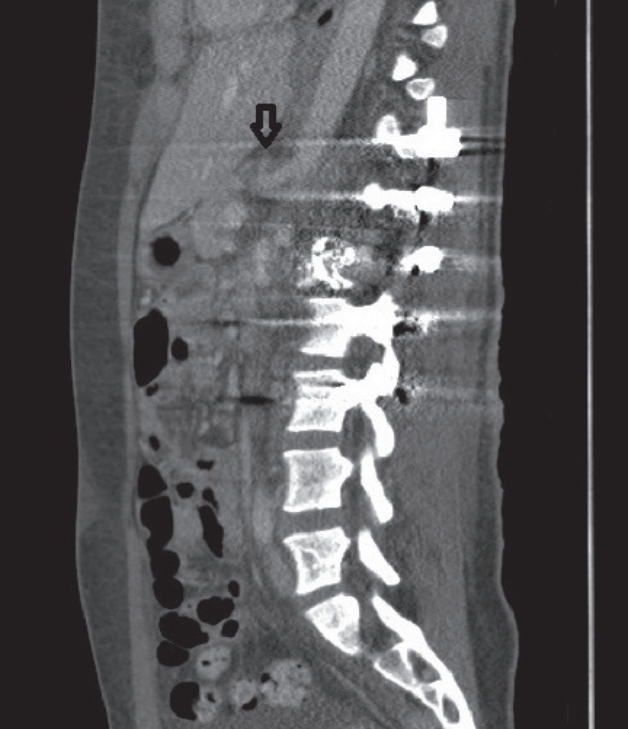
- An 18-year-old woman was brought to the trauma center after a fatal motorcycle accident. The driver was found dead. She was riding behind the driver. Her initial vital signs were stable, but she complained of mild abdominal pain, chest wall pain, and severe back pain. There were no definite neurologic deficits. Her initial X-ray examination showed multiple rib fractures, left hemothorax, a normal-shaped heart, and obvious lumbar spine dislocation (Fig. 1). A computed tomography (CT) scan was performed at the same time as the X-ray, additionally revealing moderate liver injury. She was brought to the angiography room to check for active bleeding in the liver, which was not apparent. However, the guide wire was not able to pass through the celiac trunk (Fig. 2). Angiography of the hepatic arteries was performed by selecting the superior mesenteric artery, which provided collateral circulation to the hepatic arteries and other arteries arising from the celiac artery. A review of the initial CT scan revealed kinking of the celiac artery (Fig. 3), which was assumed to have been due to altered anatomy of the median arcuate ligament caused by spine fractures. The spine surgery team conducted a careful neurologic examination and performed immediate fixation of the spine (Fig. 4). The trauma team anticipated automatic correction of the celiac artery compression after fixation, assuming that her deviated median arcuate ligament would return to the normal position, which became apparent on the follow-up CT scan of her abdomen (Fig. 5).
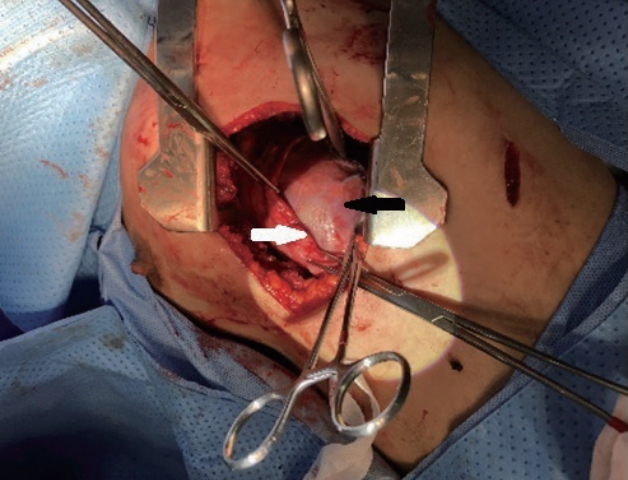
- During recovery, the patient did not complain of abdominal pain, but 3 weeks after admission, she developed a fever, and an X-ray exam revealed an abnormally enlarged heart (Fig. 6). Suspecting loculated fluid collection and possibly empyema in both lung fields and pericardiac rupture with a herniated heart, the chest surgeon team decided to perform thoracotomy, which revealed rupture of the left pericardium (Fig. 7). The laceration was about 10 centimeters long, running perpendicularly to the path of the phrenic nerve at the left side of the heart. About half of the left ventricle was herniated out of the pericardium. There was no adhesion between the pericardium and pleura, and the pericardium was quite redundant; thus, a patch was unnecessary. There was organized hematoma in the pleural cavity without evidence of pus formation, with some adhesions between the parietal pleura and lung. The surgeons decided it would be safe to repair the pericardium, which was carried out with interrupted non-absorbable sutures. Adhesiolysis and hematoma removal were then done. Five weeks after admission, the patient had recovered without complications and was discharged home.
CASE REPORT
- The median arcuate ligament is located under the diaphragm and connects the right and left crura. The crura originate from the front of the vertebral bodies and the intervertebral fibrocartilage of the lumbar spine. The median arcuate ligament forms the anterior margin of aortic hiatus, where the aorta, thoracic duct, and azygos vein pass. It is normally positioned superior to the celiac trunk, and therefore does not interfere with the flow of the celiac artery. However, the ligament may be lower in up to 25% of the population. The ligament can then compress the celiac artery, interfering with its flow and becoming pathologic [3]. This is called celiac artery compression syndrome, also known as median arcuate ligament syndrome or Dunbar syndrome. The decreased flow can diminish blood flow to the intestines, resulting in abdominal pain. Abdominal pain may be also induced by compression of the celiac ganglia. Due to its nature, it is a chronic condition which is usually diagnosed by exclusion of other gastrointestinal diseases. Thus, suspicion of this syndrome in the acute setting is even lower, especially in trauma patients.
- In this case, the patient probably had normal anatomy of the median arcuate ligament, or her ligament may have been slightly lower, without compressing the celiac artery. This would have gone unnoticed for her entire life, as long as there was no disruption of the anatomy surrounding the celiac artery, such as spine dislocation. The intense force of the motor vehicle accident dislocated her spine, which then abnormally stretched the median arcuate ligament and disoriented it from its normal position, compressing the celiac artery. This may not have been fatal since it did not completely compress the artery. Even if it had done so, the collateral circulation from the superior mesenteric artery would have adequately supplied the organs; therefore, fatal ischemia would probably not have happened. This phenomenon would have even gone unnoticed by the trauma team if her liver was not injured and angiography was not performed. Her spine obviously needed fixation, which would have unnoticeably fixed the compressed celiac artery (Fig. 8). The unusual event of an impassable guide wire through the celiac artery led the trauma team to thoroughly review the patient’s initial CT scan, finding the cause of obstruction. As mentioned above, since her spine was planned to be fixed regardless, the trauma team did not plan an additional intervention to correct the celiac artery. This was confirmed by a follow-up CT scan. If the authors had discovered the compressed artery when first looking at the CT scan, we would have still requested the angiography interventionist to check for the continuity of the celiac artery and to perform hepatic artery angiography. If the spine injury had been unfixable for any reason, and if there was evidence of organ ischemia due to the compression of the artery, we might have considered surgical correction of the artery, which would have been even more unusual.
- The pericardium encloses the pericardial cavity, which contains the heart and the roots of the great vessels. It is made up of two layers: the serous layer and the fibrous layer. The pericardium fixes the heart to the mediastinum, lubricates the heart, and protects the heart. Disruption of the pericardium results in injury to the underlying heart. In a penetrating injury, the opening of the pericardium may large enough to let the penetrating object injure the heart, but small enough to entrap the blood gushing out of the heart inside the pericardium, resulting in hemopericardium. Tamponade from this trapped blood is fatal and needs immediate decompression and consultation with a cardiac surgeon. Hemopericardium may be visible in the initial survey of trauma patients with ultrasonography. It may also be visible in cases of severe blunt trauma to the thorax if the injury is serious enough to rupture the heart. However, the injury may just strong enough to rupture only the pericardium, but not the heart, as seen in this patient.
- The patient initially complained of chest wall pain, and the initial X-ray showed hemothorax and rib fractures, as well as a normal heart contour (Fig. 1). Thus, the trauma team carefully examined her heart with ultrasonography, but did not find any hemopericardium, which was confirmed again by her initial CT scan. Injury to the heart was excluded. The team did not suspect cardiomegaly until her febrile condition called for thoracotomy, which revealed the ruptured pericardium and intact heart. The heart might have gradually herniated out of the pericardial sac without any hemodynamic dysfunction. Without a high suspicion of herniation, the gradual enlargement was overlooked due to the anterior-posterior nature of plain chest X-rays taken with the patient in the supine position. Isolated pericardium injury is usually of no consequence. However, a herniated heart may result in torsion along the inferior vena cava [4]. This may induce arrhythmia and hemodynamic instability, resulting in sudden cardiac arrest.
- The diagnosis of blunt traumatic pericardium rupture and herniated heart is difficult. It requires thorough investigations including multiple modalities such as electrocardiography, plain X-rays, echocardiography, CT, and magnetic resonance imaging [5]. The findings of pericardial rupture include focal pericardial dimpling and discontinuity and pneumopericardium, while the findings of a herniated heart include the empty pericardiac sac sign (air outlining the empty pericardium), the collar sign (compression of the cardiac contour by a pericardial band), and a dilated inferior vena cava. Above all, clinical suspicion by the medical staff is the utmost key in diagnosis. Once diagnosed, an untreated herniated heart can be fatal; thus, surgical correction is usually warranted. This can be done through thoracoscopy or thoracotomy. A small to moderate-sized pericardiac injury may be simply closed, while a larger injury may require a mesh prothesis.
- We report a case in which these two rare entities occurred simultaneously from a single blunt traumatic event. Both entities may have gone unnoticed and may not cause severe consequences in the future. Celiac artery compression was caused by spine dislocation and automatically corrected by fixation of the spine; thus, it may have been a small, temporary, and unproblematic finding. In contrast, pericardium rupture is not temporary and may cause problems. Temporary or not temporary, problematic or not problematic, rare entities may happen in any trauma patient. Trauma surgeons need to be alert and have an extremely high index of suspicion to prevent unfavorable outcomes.
DISCUSSION
Fig. 8.Schematic drawing of celiac artery compression induced by dislocation of the spine, corrected by spine fixation.


- 1. Saleem T, Katta S, Baril DT. Celiac artery compression syndrome [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 [cited 2020 Sep 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470601/.
- 2. Lindenmann J, Matzi V, Neuboeck N, Porubsky C, Ratzenhofer B, Maier A, et al. Traumatic pericardial rupture with cardiac herniation. Ann Thorac Surg 2010;89:2028–30. ArticlePubMed
- 3. Horton KM, Talamini MA, Fishman EK. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics 2005;25:1177–82. ArticlePubMed
- 4. Adams A, Fotiadis N, Chin JY, Sapsford W, Brohi K. A pictorial review of traumatic pericardial injuries. Insights Imaging 2012;3:307–11. ArticlePubMedPMCPDF
- 5. Sherren PB, Galloway R, Healy M. Blunt traumatic pericardial rupture and cardiac herniation with a penetrating twist: two case reports. Scand J Trauma Resusc Emerg Med 2009;17:64. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

 KST
KST





 PubReader
PubReader ePub Link
ePub Link Cite
Cite