Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(3); 2023 > Article
-
Original Article
Clinical characteristics of patients with the hardware failure after surgical stabilization of rib fractures in Korea: a case series -
Na Hyeon Lee, MD1
 , Sun Hyun Kim, MD1
, Sun Hyun Kim, MD1 , Seon Hee Kim, MD1
, Seon Hee Kim, MD1 , Dong Yeon Ryu, MD1
, Dong Yeon Ryu, MD1 , Sang Bong Lee, MD1
, Sang Bong Lee, MD1 , Chan Ik Park, MD1
, Chan Ik Park, MD1 , Hohyun Kim, MD1
, Hohyun Kim, MD1 , Gil Hwan Kim, MD1
, Gil Hwan Kim, MD1 , Youngwoong Kim, MD2
, Youngwoong Kim, MD2 , Hyun Min Cho, MD3
, Hyun Min Cho, MD3
-
Journal of Trauma and Injury 2023;36(3):196-205.
DOI: https://doi.org/10.20408/jti.2023.0026
Published online: September 5, 2023
- 1,208 Views
- 49 Download
- 1 Crossref
1Department of Trauma and Surgical Critical Care, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
2Department of Thoracic and Cardiovascular Surgery, National Medical Center, Seoul, Korea
3Department of Trauma Surgery, Cheju Halla General Hospital, Jeju, Korea
- Correspondence to Seon Hee Kim, MD Department of Trauma and Surgical Critical Care, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, 179 Gudeok-ro, Seo-gu, Busan 49241, Korea Tel: +82-51-240-7369 Email: ksh810427@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- Surgical stabilization of rib fractures (SSRF) is widely used in patients with flail chests, and several studies have reported the efficacy of SSRF even in multiple rib fractures. However, few reports have discussed the hardware failure (HF) of implanted plates. We aimed to evaluate the clinical characteristics of patients with HF after SSRF and further investigate the related factors.
-
Methods
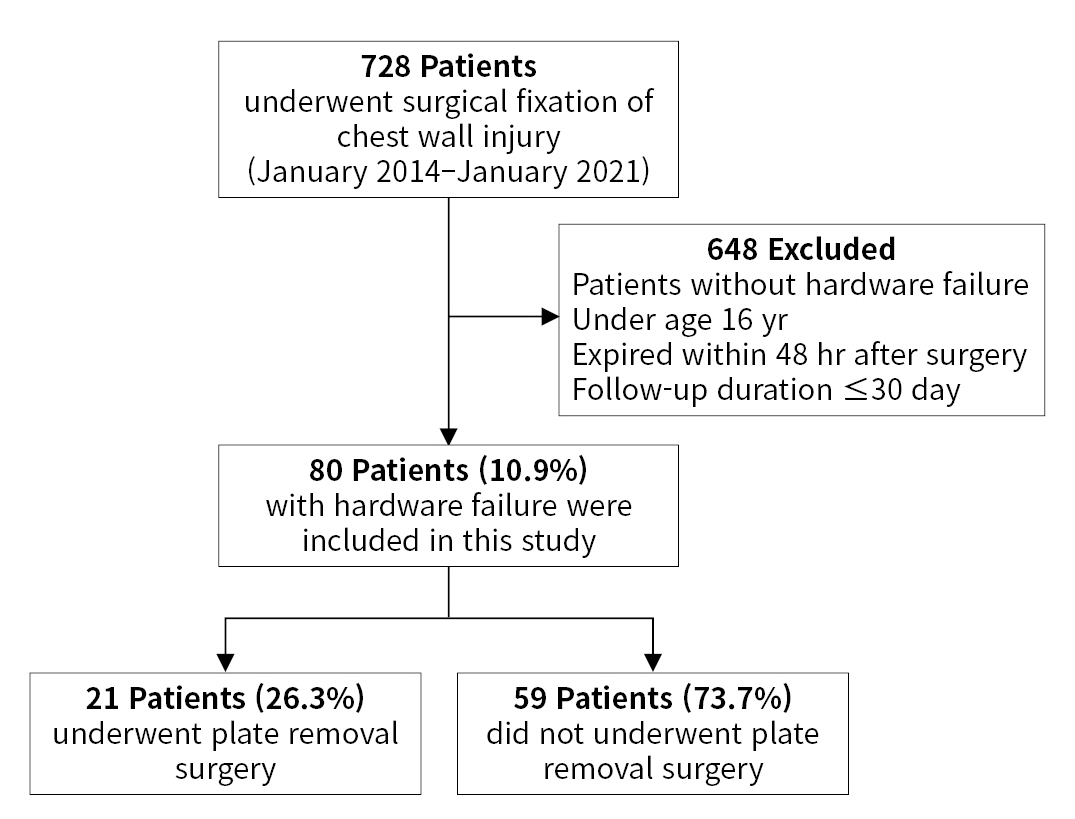
- We retrospectively reviewed the electronic medical records of patients who underwent SSRF for multiple rib fractures at a level I trauma center in Korea between January 2014 and January 2021. We defined HF as the unintentional loosening of screws, dislocation, or breakage of the implanted plates. The baseline characteristics, surgical outcomes, and types of HF were assessed.
-
Results
- During the study period, 728 patients underwent SSRF, of whom 80 (10.9%) were diagnosed with HF. The mean age of HF patients was 56.5±13.6 years, and 66 (82.5%) were men. There were 59 cases (73.8%) of screw loosening, 21 (26.3%) of plate breakage, 17 (21.3%) of screw migration, and seven (8.8%) of plate dislocation. Nine patients (11.3%) experienced wound infection, and 35 patients (43.8%) experienced chronic pain. A total of 21 patients (26.3%) underwent reoperation for plate removal. The patients in the reoperation group were significantly younger, had fewer fractures and plates, underwent costal fixation, and had a longer follow-up. There were no significant differences in subjective chest symptoms or lung capacity.
-
Conclusions
- HF after SSRF occurred in 10.9% of the cases, and screw loosening was the most common. Further longitudinal studies are needed to identify risk factors for SSRF failure.
- Background
- Multiple rib fractures are the most common injuries observed after blunt chest trauma and account for approximately 10% of all trauma cases [1]. As rib fractures are frequently accompanied by major intrathoracic and extrathoracic injuries, they are inevitably associated with severe damage, pain, and long-term sequelae [2–4]. Furthermore, more fractured ribs and older age were associated with poorer outcomes [5,6]. Insufficient ventilation and impaired pulmonary hygiene due to pain can lead to critical respiratory complications in these patients. Pain control, respiratory support, and pulmonary rehabilitation are the standard therapies for rib fractures, conventionally [1]. However, over the past few decades, there has been emerging interest in the surgical stabilization of rib fractures (SSRF) with technological advancements in surgical instruments. Previous randomized studies have demonstrated that SSRF reduces the duration of hospital stay, ventilator days, the occurrence of pneumonia, and mortality in patients with flail chest [7–9]. Recent trials on chest wall injuries have shown favorable outcomes in terms of pain and disability-related quality of life among patients with a nonflail chest [10]. Throughout the literature supporting the advantages of SSRF, the indications for SSRF have expanded, and SSRF is now becoming an established technique at regional trauma centers [11–13].
- As the use of SSRF increases, concerns regarding surgical complications have inevitably been raised. To stabilize a fractured rib, SSRF usually involves nonabsorbable metallic implants. Unlike other bones, the ribs continue to move while breathing after orthopedic surgery, which can contribute to long-term complications. Recent studies have reported an incidence of up to 10% for complications, including bleeding, infection, inadequate bone healing, implant-related irritation, and implant failure [14]. Despite the assumption of relative safety, little is known about the long-term complications of SSRF, particularly those associated with hardware failure (HF) of the implanted plates. HF is defined as the unintentional loosening of screws, dislocation, or breakage of implanted plates and can occur for various reasons, such as improper placement, insufficient screw fixation, or a lack of plate length [15]. Previous studies have investigated the efficacy of SSRF and its associated risks; however, few have explored the clinical characteristics and factors related to HF after SSRF [14–18]. Understanding the clinical characteristics and risk factors of HF can help improve patient selection, surgical techniques, and postoperative care, which may reduce the incidence of complications and improve patient outcomes.
- Objectives
- In this study, we aimed to retrospectively analyze the electronic medical records of patients who underwent SSRF for multiple rib fractures at a level I trauma center in Korea to assess the clinical characteristics of patients with HF and further investigate the factors related to reoperation. We hypothesized that HF after SSRF is not prevalent and typically has insignificant clinical consequences.
INTRODUCTION
- Ethics statement
- This study was approved by the Ethics Committee of Pusan National University Hospital (No. H-2205-007-114). The requirement for informed consent was waived due to the retrospective nature of the study. The study was conducted in accordance with the Declaration of Helsinki for experiments involving humans.
- Study setting and populations
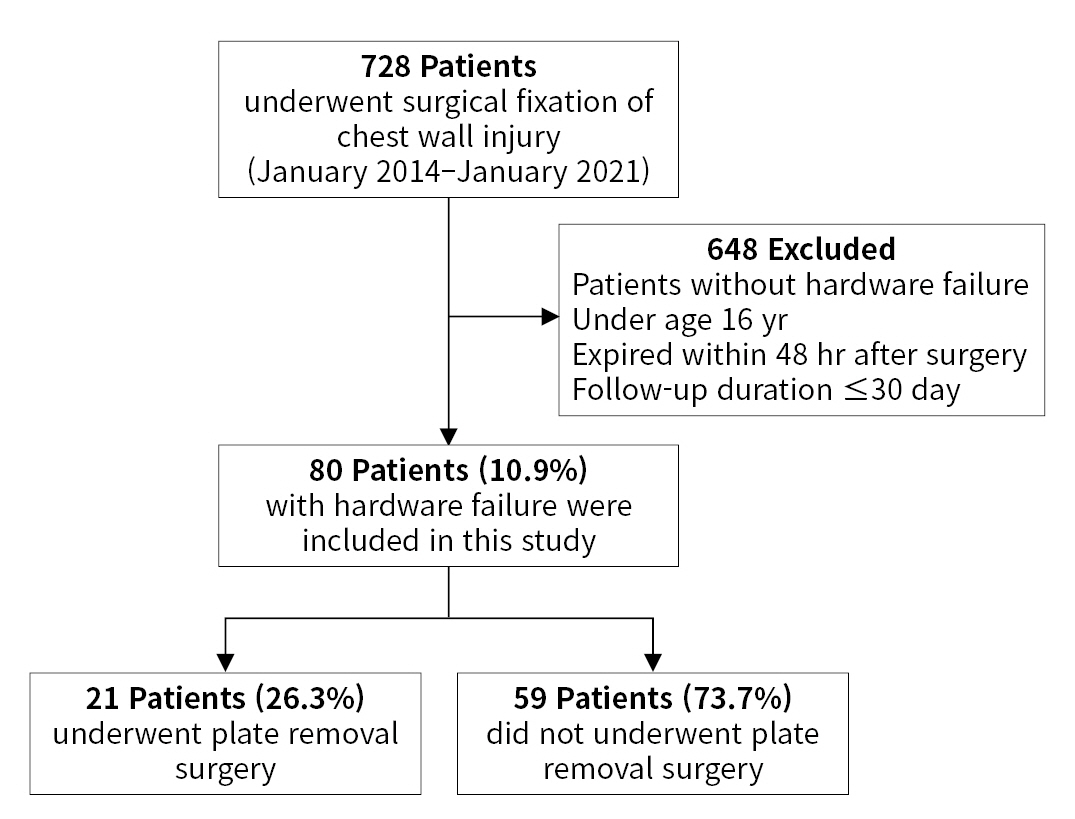
- This retrospective cohort study was performed at a regional trauma center between January 1, 2014 and January 1, 2021. Using the hospital inpatient inquiry system, 5,792 patients with chest injuries admitted to the level I trauma center were identified. We selected patients who had undergone surgical fixation of the chest wall. A total of 728 patients who underwent SSRF were included in the study. The exclusion criteria were as follows: no HF, age <16 years, death within 48 hours after surgery, and follow-up duration <30 days. The final study population comprised 80 patients with HF after SSRF (Fig. 1).
- Data collection
- Patient demographics, mechanisms of injury, and SSRF and HF characteristics were recorded. The available data included age, sex, mechanism of injury, Injury Severity Score (ISS), anatomical features of the chest wall injuries (flail chest, bilateral fracture, sternal fracture, number of rib fractures, costal fractures), HF, location, failed plating system, failure mode, time to detection of HF, surgical details (such as fixation site, number of plates implanted, fixed rib number, and time to SSRF), any postoperative complication, reoperation, hospital stay, laboratory values of pulmonary function, follow-up duration, and survival status. In addition, a subgroup analysis was performed by dividing the patients into two groups according to whether metal removal was performed.
- The consensus of the Chest Wall Injury Society (CWIS) was used to describe the location of rib fractures [19]. The chest wall was defined as having three sectors: the anterior, lateral, or posterior sector. These were divided by the anterior and posterior axillary lines, where the anterior axillary line defined the border between the anterior and lateral fractures and the posterior axillary line defined the border between the lateral and posterior fractures. In addition to these three sectors, the costal cartilage sector was recorded. A flail segment was defined as three or more consecutive ribs that fractured in more than one location, producing a free-floating segment of the chest wall.
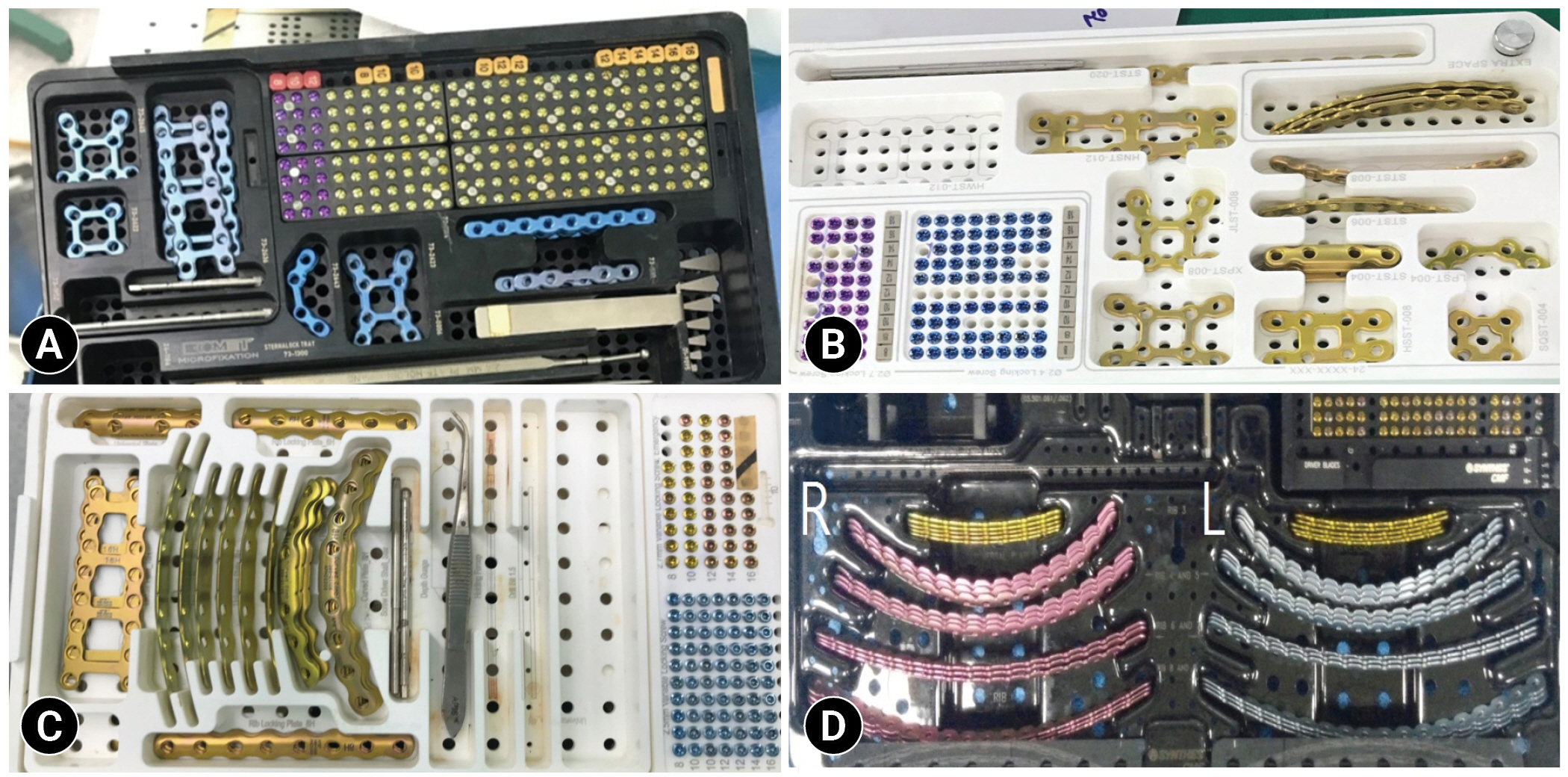
- During the study period, four thoracic surgeons performed SSRF using at least one of four commercially available plating systems, all of which were anterior bicortical screw locking systems: SternaLock Blu Plate (Zimmer Biomet Inc), ARIX Sternal & Rib System (Jeil Medical Corp), APIS Rib Locking Plate System (TDM Corp), and MatrixRIB Fixation System (Depuy Synthes) (Fig. 2). All the systems included straight or precontoured titanium plates and self-drilling and self-tapping screws, except for the MatrixRIB Plate. The choice of plating system was at the discretion of the surgeon.
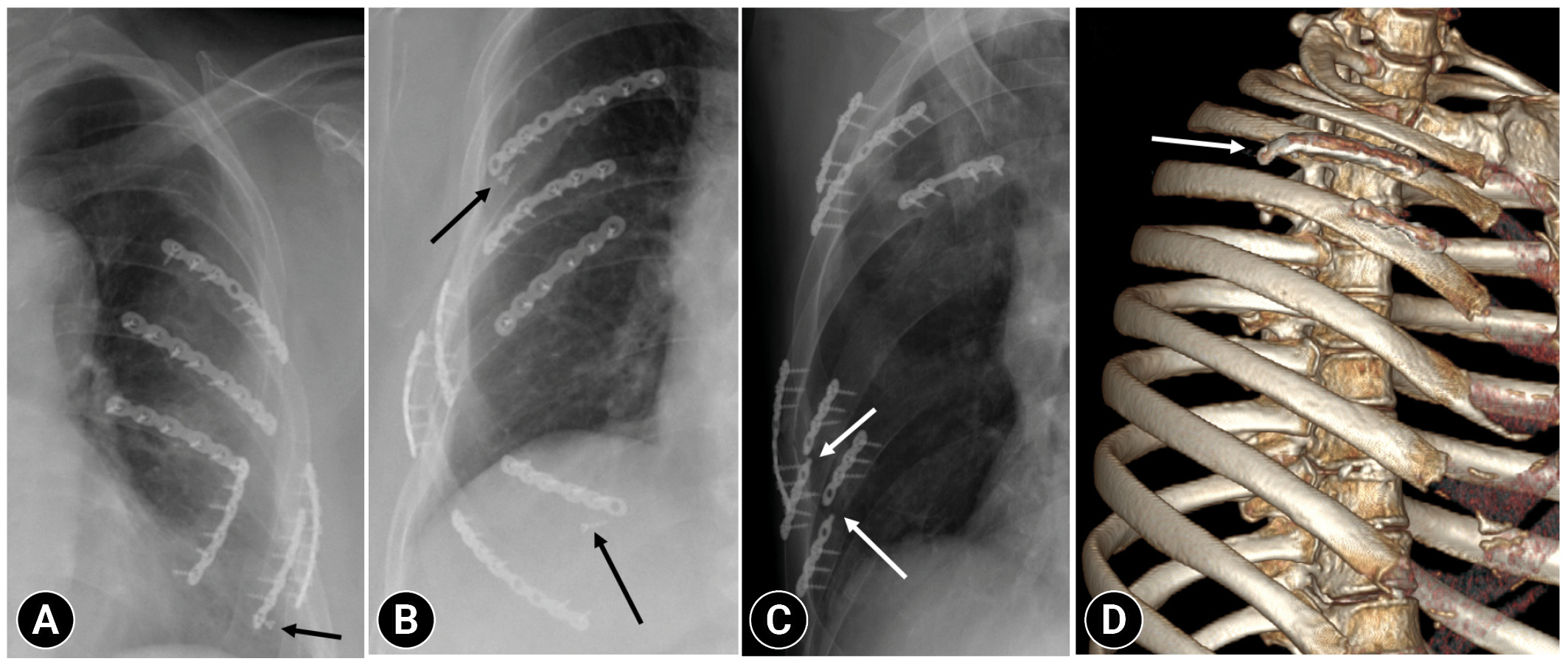
- HF was defined as follows: (1) screw loosening, defined as a screw that protrudes from the screw hole but does not pull out completely; (2) screw migration, defined as a screw being pulled out of a screw hole and moved to a completely different position; (3) plate fracture, defined as breakage of implanted plates; and (4) plate dislocation, defined as the displacement of a plate superiorly or inferiorly (Fig. 3).
- All patients visited the hospital regularly at 3, 6, and 12 months after surgery. Three-dimensional chest computed tomography (CT), pulmonary function tests, and chest radiography were routinely performed. HF was confirmed using routine imaging after surgery.
- Outcome measure
- The primary objective of this study was to report the incidence, characteristics, and clinical impact of HFs. The secondary objective was to determine the differences between patients who underwent reoperation (the plate removal surgery group) and those who did not.
- Statistical analysis
- Summary statistics are reported as median and interquartile range (IQR) or mean±standard deviation, where appropriate. Categorical variables are expressed as numbers and percentages. Chi-square and Fisher exact tests were used to compare the frequencies of categorical variables between the groups. The Mann-Whitney U-test and Wilcoxon rank-sum test were used to compare the mean values of continuous variables. We used the receiver operating characteristic (ROC) curve and area under the curve (AUC) to evaluate predictive factors for plate removal. A P-value of <0.05 was considered statistically significant. Statistical analysis was performed using IBM SPSS ver. 22 (IBM Corp).
METHODS
Definition of anatomic location chest wall injury
Type of chest wall plating system
Definition of HF mode
HF detection
- Characteristics of the patients with HF
- The demographic characteristics of patients with HF are summarized in Table 1. The overall incidence of HF after SSRF was 10.9% (80 of 728). The mean age of HF patients was 56.5±13.6 years, with the most common mechanism being motor vehicle accidents (57.5%). The median number of fractured ribs per patient was 9 (IQR, 4–24) and 73.8% of the patients had a flail segment. The median ISS was 22 (IQR, 4–45), indicating a severe injury. In terms of comorbidities, the majority of patients (68.6%) had no underlying disease, whereas those with diabetes mellitus (2.5%) had ischemic heart disease.
- SSRF was performed within 7.5 days by four thoracic surgeons with SSRF experience ranging from 1 to more than 10 years. At least one of the four commercially available plating systems was chosen for the SSRF, with the most commonly used system being ARIX (62.5%), followed by the SternaLock (41.3%), APIS (22.5%), and MatrixRIB (3.8%). An average of four ribs (IQR, 1–13) were fixed, and six plates (IQR, 1–29) were implanted. SSRF was mainly performed anterolaterally (anterior, 52.5%; lateral, 72.5%; and posterior, 43.8%). This is consistent with the most common location of HF.
- Although no deaths were reported during hospitalization, perioperative complications such as pneumonia (51.2%), acute kidney injury (16.3%), and wound infection (11.3%) occurred. Thirty-five patients (43.8%) experienced chronic pain during follow-up. Thirty-two patients (40.0%) presented with normal lung capacity at the last follow-up. A total of 21 patients (26.3%) underwent reoperation for plate removal.
- Clinical features of HF in total cohort
- The clinical features of patients with HF are shown in Table 2. The mean time from implantation to HF was approximately 3 months. HF was detected in the anterolateral region of the chest (78.8%), and screw loosening (73.8%) was the most common mode of failure. The ARIX plating system was used more frequently, resulting in HF. By location, 42.4% lateral screw loosening, 52.9% anterior screw migration, 47.6% posterolateral plate fractures, and 57.1% anterior plate dislocations were recorded. In addition, the ARIX system in the anterolateral sector and the SternaLock system in the posterior sector failed. Screw loosening, screw migration, and plate fractures were more common in the ARIX system (Table 3). However, there was no statistically significant correlation between the failure location, failed plate, and failure mode. Although up to 80% of the HF cases occurred in the ARIX and SternaLock systems, the correlation was not statistically significant (P=0.12 and P=0.29, respectively). There was no definitive relationship between anterolateral location and HF (P=0.70 and P=0.80, respectively) (Table 4). Furthermore, screw failure occurred in 12 of the 14 patients (85.7%) who underwent costal fixation; however, the difference was not statistically significant (P=0.33).
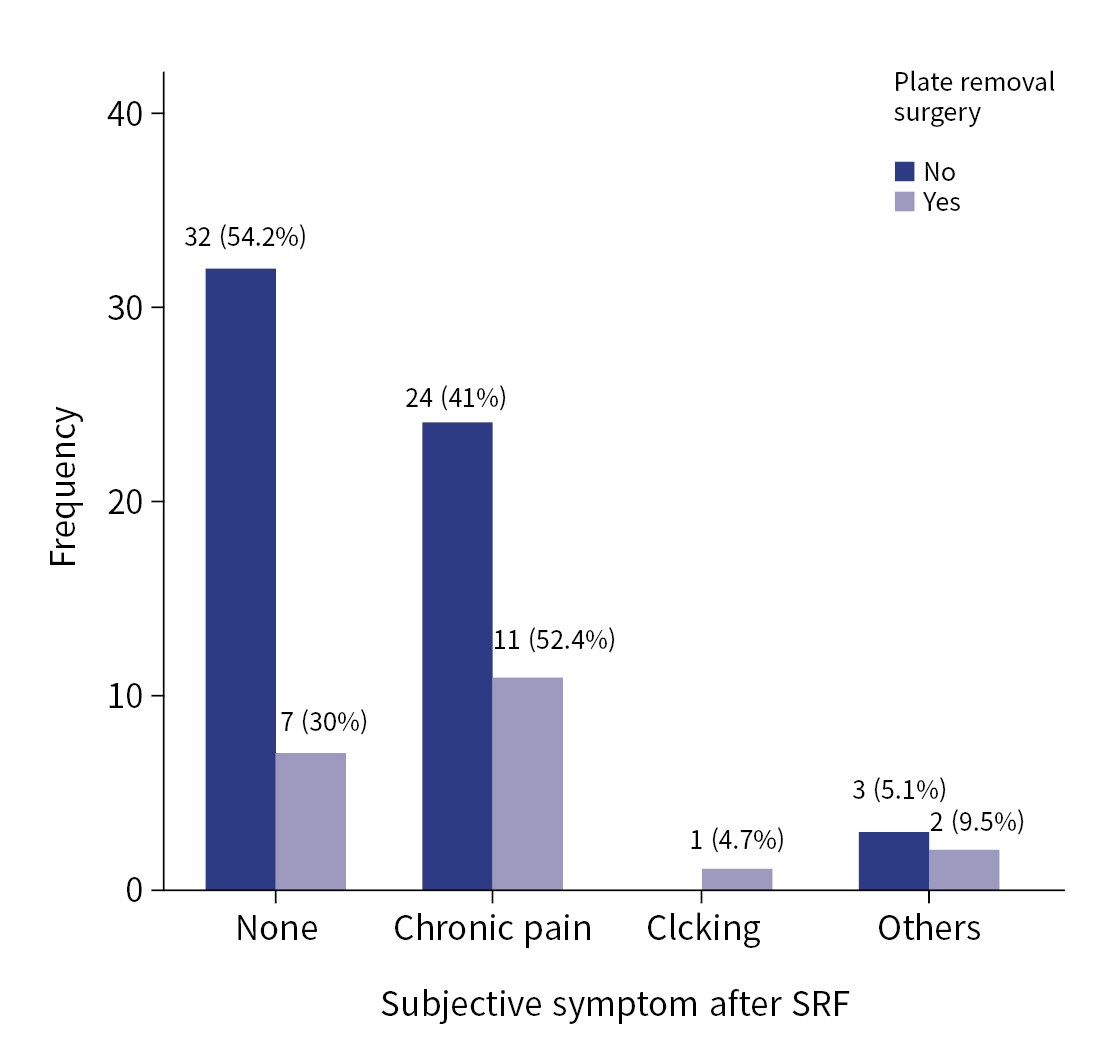
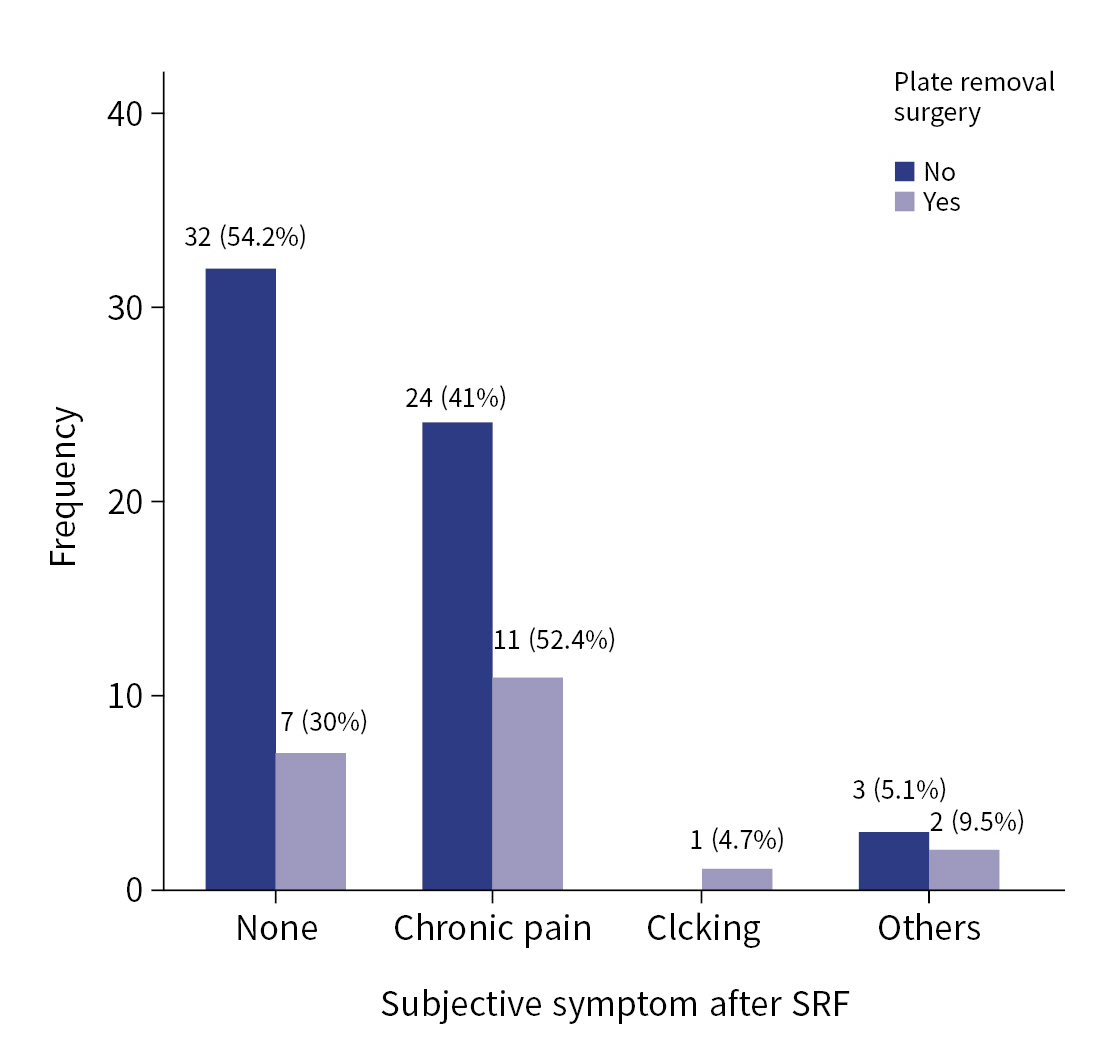
- Comparison of patients’ characteristics according to plate removal surgery
- Table 5 demonstrates the differences between patients with HF who underwent reoperation (the plate removal surgery group) and those who did not undergo reoperation. The reoperation group was statistically significantly younger (59.1±12.8 years vs. 49.1±13.3 years, P=0.03), had fewer fractures (10.0±4.6 vs. 7.2±5.0, P=0.01), and had more costal fixation (11.8% vs. 80.9%, P=0.04). SSRF performed at another location on the chest wall was more common in patients who did not undergo reoperation (67.8% vs. 47.6%, P=0.03). Although there was no difference in the failure mode or plating system between the two groups, the failure location, especially in the anterior sternum, was frequent in the reoperation group (P=0.007). The time to detect HF was not different, but the follow-up duration was longer in reoperation group (312.8±244.7 vs. 487.3±371.4, P=0.01). There were no significant differences in wound infection, subjective chest symptoms, or lung capacity at the last follow-up. A total of 52.4% of patients with plate removal surgery experienced chronic chest pain; however, no statistically significant difference was noted between the groups (P=0.13) (Fig. 4).
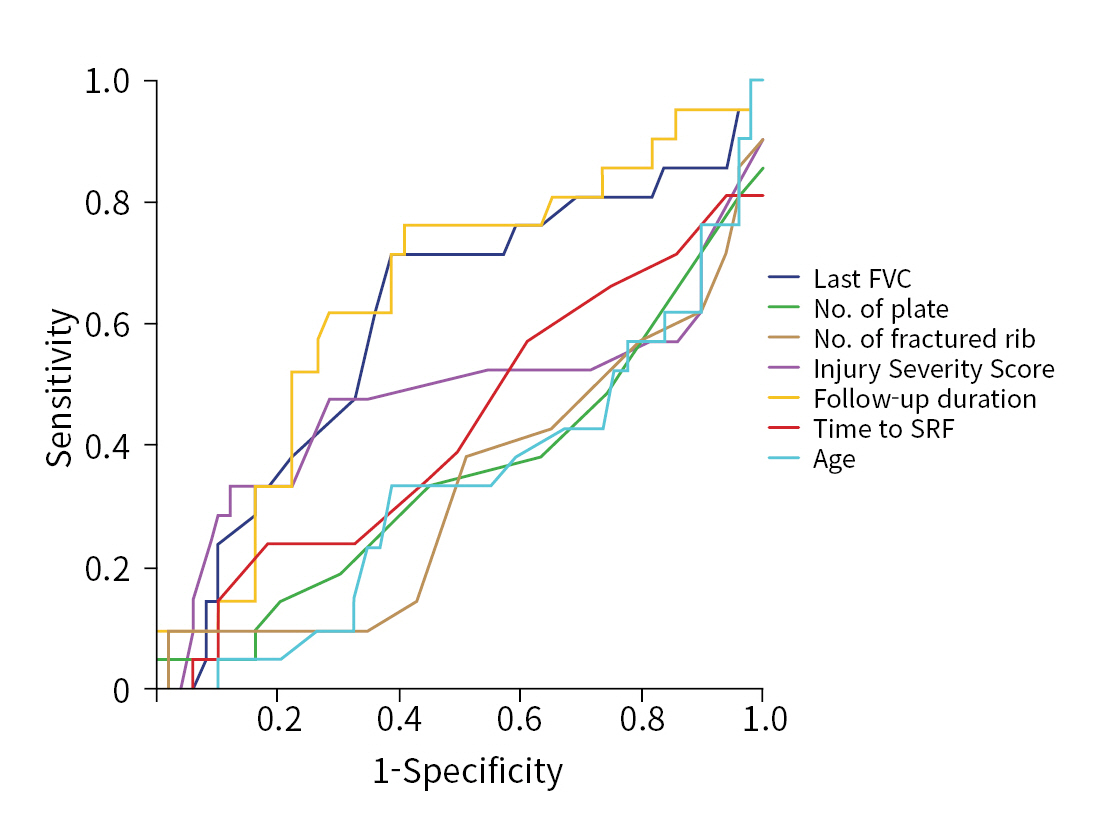
- ROC analysis
- ROC curve analyses were performed on the variables that identified differences according to the plate removal surgery. Using a single-factor evaluation, AUC was low: follow-up duration, last functional vital capacity (FVC), time to SSRF, ISS, number of fractured ribs, number of implanted plates, and age showed AUCs of 0.647, 0.609, 0.431, 0.477, 0.331, 0.354, and 0.337, respectively (Fig. 5).
RESULTS
- This is the first study to describe the incidence and clinical features of HF after SSRF in a contemporary cohort of level I regional trauma centers in Korea. We found that the overall incidence of HF after SSRF was 10.9% (80 of 728) over the 7 years. Screw failure was the most common type of HF, followed by plate fractures and plate dislocations. HF frequently occurs in the anterolateral region, including the costal cartilage. Half of these patients experienced subjective symptoms, and only 26.3% underwent plate removal surgery. Plate removal was associated with a younger age, fewer fixed ribs, failure location in the anterior region, especially in the costal cartilage portion, and a long follow-up duration. There was no relationship among the failure mode, failure location, and plating system.
- SSRF has become increasingly popular in recent years as multiple studies have demonstrated its benefits, even in nonfrail rib fractures [7–10,20]. As the indications for SSRF have expanded, it has become essential to identify and analyze the long-term surgical complications associated with this procedure. Since its inception in the early 21st century, there have been only a few case reports or single-center studies of implant-related complications [21–27]. In 2019, the CWIS published a multicenter retrospective study reporting a 3% (38 of 1,224) HF rate after SSRF, mainly due to screw migration (n=17, 44.7%) and plate fracture (n=18, 47.4%) in the posterolateral region. Forty percent of these patients were asymptomatic, and 55% required explantation of the hardware [15]. The authors concluded that HF after SSRF rarely occurs and is clinically insignificant. A systematic review published in 2020 also reported a low HF risk [14]. Through a review of 1952 SSRF patients, the study reported 173 surgery- and implant-related complications (10.3%). Implant irritation was the most common (n=65, 6.9%) implant-related complication, and only one patient (0.1%) presented with a plate fracture. The most recent meta-analysis showed similar results, with 4% (range, 3%–7%) of HF cases reported, including mechanical failure, infection, pain or discomfort, and nonunion [28]. Broken plates were the most common cause of HF, and insufficient patient data precluded the characterization of the failure location and reasons for failure.
- The incidence of HF in our study was slightly higher (10.3%) than that reported previously. This difference can be attributed to two factors. First, the detection rate may have increased due to regular follow-up after surgery. Previous multicenter study lacked follow-up imaging protocols, which may have led to underreporting [15]. However, in our center, we followed a specific imaging protocol, including an x-ray check-up 2 weeks after postdischarge and three-dimensional CT imaging at 3, 6, and 12 months after surgery, which could have contributed to the higher detection rate. Second, the surgeon might have played a role, as the four surgeons involved may have differed in ability, experience, and technical selection, such as the number of screws and plate length, based on the fracture pattern. Although the plate locking screw system theoretically leads to more plate fractures or dislocations, the higher screw failure rate in our study could be attributed to technical errors. To minimize technical errors, it is essential to be meticulous during surgery, focusing on details such as bicortical screwing, proper plate fitting on the rib surface, adequate plate length, and reduction in bone defects.
- Compared to other orthopedic surgeries, SSRF poses unique technical challenges because immobilization after surgery is not possible. The posterolateral region is known to experience the most stress during respiration, and plate fatigue in this area can result in the fracture or dislocation of the plate [15,29]. We found that plate fracture or dislocation occurred more frequently in the posterolateral region of the chest. However, to better understand the correlation between the location and mode of metal failure, further research on the biomechanics of metal respiration is necessary. In terms of plating systems, we used four distinct locking screw plate systems that varied in terms of metal thickness, shape, and minor deviations. Despite these variations, no correlation between the plating system and the failure modes was observed in this study. Although ARIX occurred more frequently in HF cases, it was deemed insignificant because it was the most commonly used metal.
- Among the patients who experienced HF, only 23% underwent metal removal surgery. Of these patients, only two underwent removal due to infection, while the rest underwent surgery due to irritation symptoms, such as pain, tightness, or sensitivity to touch, or during surgery to remove metal from other areas, particularly in cases of orthopedic surgery. Metal removal surgery was more common in younger patients, those with fewer rib plates, and in the anterior region, particularly the costal cartilage, than in the nonsurgical group. Elderly patients with multiple areas requiring metal removal surgery may be hesitant to undergo this procedure because of the potential increased surgical risks and associated complications. Given the relatively infrequent occurrence of HF and the low likelihood of subsequent reoperations, the clinical implications of HF are not particularly substantial. However, this is a technical shortcoming; it is essential to follow proper surgical techniques and carefully monitor patients after surgery to minimize the risk of mechanical complications.
- Limitations
- First, as this was a single-center study, it cannot be considered representative of other trauma centers in Korea. Second, the sample size was insufficient to yield statistically significant results. Although we observed a high frequency of screw failure in the anterior region, no significant correlation was found between the associated variables. Therefore, it is imperative to conduct further multicenter studies with a larger patient cohort to elucidate the underlying characteristics of HF in patients undergoing SSRF. Third, this study had several confounding factors. Differences in technical skills, such as the type of plates selected, the length of the plates used, and the number of screws used, may vary among surgeons. Because HF is a technical error, these factors may have influenced the results. Moreover, the frequency of the surgical sites or plating systems cannot be applied uniformly, leading to a selection bias that affects the results. Given the constrained sample size of the four plating systems, it was impractical to establish any discernible variance in HF outcomes attributed to the particular plating system employed. To conduct an investigation in this regard, it would be necessary to perform an analysis incorporating each plating system with a substantial sample size, carried out by a single surgeon.
- Conclusions
- HF occurred in 10.9% of cases following SSRF, with no observed correlation between the mode, location, or type of plate used. Patients with coastal fractures require special attention. Although not all patients require plate removal surgery, HF is a technical shortcoming requiring increased surgical vigilance. Furthermore, a deeper understanding of respiratory dynamics through additional research is needed to better understand the etiology of HF.
DISCUSSION
-
Author contributions
Conceptualization: Seon Hee K, YK, HMC; Data curation: DYR, CIP, YK; Formal analysis: DYR, SBL, HK, GHK; Funding acquisition: Seon Hee K; Investigation: Sun Hyun K, NHL; Methodology: SBL, CIP, HK; Project administration: Seon Hee K; Writing–original draft: Sun Hyun K, NHL; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
Seon Hee Kim and Hohyun Kim are Editorial Board members of the Journal of Trauma and Injury but were not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
-
Funding
This study was supported by a National Research Foundation of Korea (NRF) grant (No.2020R1F1A1052713), funded by the Ministry of Science and ICT of Korea; and Pusan National University Research Grant in 2020.
-
Data availability
Data of this study are available from the corresponding author upon reasonable request.
-
Additional information
This study was presented at the 9th Pan-Pacific Trauma Congress (PPTC) in July 2022 in Gyeongju, Korea.
ARTICLE INFORMATION
| Clinical feature | Value (n=80) |
|---|---|
| Time to detection of hardware failure (day) | 84.0±131.2 |
| Failure location | |
| Anterior | 28 (35.0) |
| Lateral | 35 (43.8) |
| Posterior | 18 (22.5) |
| Sternum | 7 (8.8) |
| Failed plating systema) | |
| SternaLock | 27 (33.8) |
| ARIX | 45 (56.3) |
| APIS | 10 (12.5) |
| MatrixRIB | 1 (1.3) |
| Failure mode | |
| Screw loosening | 59 (73.8) |
| Screw migration | 17 (21.3) |
| Plate fracture | 21 (26.3) |
| Plate dislocation | 7 (8.8) |
| Variable | Failure location | Failed plating systema) | ||||||
|---|---|---|---|---|---|---|---|---|
| Anterior | Lateral | Posterior | Sternum | SternaLock | ARIX | APIS | MatrixRIB | |
| Failure mode | ||||||||
| Screw loosening | 22 (37.3) | 25 (42.4) | 11 (18.6) | 7 (11.9) | 17 (28.8) | 37 (62.7) | 7 (11.8) | 0 |
| Screw migration | 9 (52.9) | 6 (35.3) | 4 (23.5) | 1 (5.9) | 5 (29.4) | 10 (58.8) | 3 (17.6) | 0 |
| Plate fracture | 5 (23.8) | 10 (47.6) | 10 (47.6) | 0 | 8 (38.1) | 10 (47.6) | 4 (19.0) | 1 (4.8) |
| Plate dislocation | 4 (57.1) | 2 (28.6) | 2 (28.6) | 0 | 4 (57.1) | 3 (42.9) | 1 (14.3) | 0 |
| Failure location | ||||||||
| Anterior | - | - | - | - | 11 (39.3) | 17 (60.7) | 3 (10.7) | 0 |
| Lateral | - | - | - | - | 8 (22.9) | 21 (60.0) | 6 (17.1) | 0 |
| Posterior | - | - | - | - | 9 (50.0) | 7 (38.9) | 3 (16.7) | 1 (5.6) |
| Sternum | - | - | - | - | 3 (42.9) | 4 (57.1) | 0 | 0 |
| Variable | No (n=59) | Yes (n=21) | P-value |
|---|---|---|---|
| Age (yr) | 59.1±12.8 | 49.1±13.3 | 0.030 |
| Male sex | 49 (83.1) | 17 (80.9) | - |
| Motor vehicle accident | 34 (57.6) | 12 (57.1) | - |
| Injury severity | |||
| Injury Severity Score | 23.5±9.0 | 21.5±12.7 | - |
| Flail segment | 50 (84.7) | 9 (42.8) | 0.010 |
| Bilateral rib fracture | 25 (42.4) | 6 (28.6) | - |
| Sternal fracture | 9 (15.3) | 5 (23.8) | - |
| No. of rib fractures | 10.0±4.6 | 7.2±5.0 | 0.010 |
| Surgical procedure | |||
| Time from admission to SRF (day) | 8.0±7.0 | 6.1±4.4 | - |
| No. of fixed ribs | 4.5±1.7 | 4.1±2.8 | - |
| No. of implanted plates | 6.8±3.4 | 5.9±5.9 | 0.050 |
| Fixation of costal cartilage | 7 (11.8) | 17 (80.9) | 0.040 |
| Fixation sector of chest wall | 0.030 | ||
| Anterior | 6 (10.2) | 4 (19.0) | |
| Lateral | 7 (11.8) | 2 (9.5) | |
| Posterior | 6 (10.2) | 2 (9.5) | |
| Combined | 40 (67.8) | 10 (47.6) | |
| Sternum (isolated) | 0 | 3 (14.3) | |
| HF | |||
| Failure mode | - | ||
| Screw loosening | 42 (71.2) | 17 (80.9) | |
| Screw migration | 7 (11.8) | 0 | |
| Plate fracture | 13 (22.0) | 8 (38.1) | |
| Plate dislocation | 12 (20.3) | 5 (23.8) | |
| Failed plating systema) | 0.060 | ||
| SternaLock | 19 (32.2) | 8 (38.1) | |
| ARIX | 33 (55.9) | 12 (57.1) | |
| APIS | 8 (13.6) | 2 (9.5) | |
| MatrixRIB | 0 | 1 (4.8) | |
| Failure location | 0.007 | ||
| Anterior | 18 (30.5) | 10 (47.6) | |
| Lateral | 31 (52.5) | 4 (19.0) | |
| Posterior | 11 (18.6) | 7 (33.3) | |
| Sternum | 2 (3.4) | 5 (23.8) | |
| Complication | |||
| Wound infection | 6 (10.2) | 14 (66.7) | - |
| Pneumonia | 34 (57.6) | 7 (33.3) | - |
| Acute kidney injury | 11 (18. 6) | 2 (9.5) | - |
| Tracheostomy | 26 (44.1) | 3 (14.3) | 0.018 |
| Hospital stay (day) | 53.2±61.3 | 49.2±79.6 | - |
| Patients’ follow-up | |||
| Time to detection HF | 62.8±96.8 | 143.9±189.0 | - |
| Follow-up duration (day) | 312.8±244.7 | 487.3±371.4 | 0.010 |
| Subjective chest symptoms | 27 (45.8) | 14 (66.7) | - |
| FVC ≥80% predicted | 19 (32.2) | 15 (71.4) | - |
Values are presented as mean±standard deviation or number (%).
SRF, surgical rib fixation; HF, hardware failure; FVC, functional vital capacity
a) SternaLock Blu Plate (Zimmer Biomet Inc), ARIX Sternal & Rib System (Jeil Medical Corp), APIS Rib Locking Plate System (TDM Corp), and MatrixRIB Plate (Depuy Synthes).
- 1. Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014;76:462–8. PubMed
- 2. Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients: still a relevant problem? Scand J Trauma Resusc Emerg Med 2017;25:42. ArticlePubMedPMCPDF
- 3. Marasco S, Lee G, Summerhayes R, Fitzgerald M, Bailey M. Quality of life after major trauma with multiple rib fractures. Injury 2015;46:61–5. ArticlePubMed
- 4. Fabricant L, Ham B, Mullins R, Mayberry J. Prolonged pain and disability are common after rib fractures. Am J Surg 2013;205:511–6. ArticlePubMed
- 5. Bulger EM, Arneson MA, Mock CN, Jurkovich GJ. Rib fractures in the elderly. J Trauma 2000;48:1040–7. ArticlePubMed
- 6. Coary R, Skerritt C, Carey A, Rudd S, Shipway D. New horizons in rib fracture management in the older adult. Age Ageing 2020;49:161–7. ArticlePubMedPDF
- 7. Liu T, Liu P, Chen J, Xie J, Yang F, Liao Y. A randomized controlled trial of surgical rib fixation in polytrauma patients with flail chest. J Surg Res 2019;242:223–30. ArticlePubMed
- 8. Marasco SF, Davies AR, Cooper J, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J Am Coll Surg 2013;216:924–32. ArticlePubMed
- 9. Tanaka H, Yukioka T, Yamaguti Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727–32. ArticlePubMed
- 10. Pieracci FM, Leasia K, Bauman Z, et al. A multicenter, prospective, controlled clinical trial of surgical stabilization of rib fractures in patients with severe, nonflail fracture patterns (Chest Wall Injury Society NONFLAIL). J Trauma Acute Care Surg 2020;88:249–57. ArticlePubMed
- 11. Kasotakis G, Hasenboehler EA, Streib EW, et al. Operative fixation of rib fractures after blunt trauma: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2017;82:618–26. PubMed
- 12. Kane ED, Jeremitsky E, Pieracci FM, Majercik S, Doben AR. Quantifying and exploring the recent national increase in surgical stabilization of rib fractures. J Trauma Acute Care Surg 2017;83:1047–52. ArticlePubMed
- 13. Brasel KJ, Moore EE, Albrecht RA, et al. Western Trauma Association critical decisions in trauma: management of rib fractures. J Trauma Acute Care Surg 2017;82:200–3. PubMed
- 14. Peek J, Beks RB, Hietbrink F, et al. Complications and outcome after rib fracture fixation: a systematic review. J Trauma Acute Care Surg 2020;89:411–8. ArticlePubMed
- 15. Sarani B, Allen R, Pieracci FM, et al. Characteristics of hardware failure in patients undergoing surgical stabilization of rib fractures: a Chest Wall Injury Society multicenter study. J Trauma Acute Care Surg 2019;87:1277–81. ArticlePubMed
- 16. Peek J, Kremo V, Beks R, et al. Long-term quality of life and functional outcome after rib fracture fixation. Eur J Trauma Emerg Surg 2022;48:255–64. ArticlePubMedPDF
- 17. Uchida K, Miyashita M, Kaga S, et al. Long-term outcomes of surgical rib fixation in patients with flail chest and multiple rib fractures. Trauma Surg Acute Care Open 2020;5:e000546ArticlePubMedPMC
- 18. Marasco SF, Martin K, Niggemeyer L, Summerhayes R, Fitzgerald M, Bailey M. Impact of rib fixation on quality of life after major trauma with multiple rib fractures. Injury 2019;50:119–24. ArticlePubMed
- 19. Edwards JG, Clarke P, Pieracci FM, et al. Taxonomy of multiple rib fractures: results of the chest wall injury society international consensus survey. J Trauma Acute Care Surg 2020;88:e40–5. ArticlePubMed
- 20. Buyukkarabacak YB, Sengul AT, Celik B, et al. The usefulness of early surgical rib stabilization in flail chest. Acta Chir Belg 2015;115:408–13. ArticlePubMed
- 21. Sawan TG, Nickerson TP, Thiels CA, et al. Load sharing, not load bearing plates: lessons learned from failure of rib fracture stabilization. Am Surg 2016;82:E15–7. ArticlePubMedPDF
- 22. de Jong MB, Houwert RM, van Heerde S, de Steenwinkel M, Hietbrink F, Leenen LP. Surgical treatment of rib fracture nonunion: a single center experience. Injury 2018;49:599–603. ArticlePubMed
- 23. Kim KT, Chang SW. An unexpected fracture of a titanium rib plate in a patient with traumatic brain injury. Trauma Case Rep 2019;24:100254. ArticlePubMedPMC
- 24. Kazakova T, Tafen M, Wang W, Petrov R. Rescue re-do inline osteosynthesis with wire cerclage for failed rib plating of multilevel rib nonunion. J Cardiothorac Trauma 2019;4:59–62. ArticlePubMedPMC
- 25. Metsemakers WJ, Kuehl R, Moriarty TF, et al. Infection after fracture fixation: current surgical and microbiological concepts. Injury 2018;49:511–22. ArticlePubMed
- 26. Hernandez MC, Reisenauer JS, Aho JM, et al. Bone autograft coupled with locking plates repairs symptomatic rib fracture nonunions. Am Surg 2018;84:844–50. ArticlePubMedPDF
- 27. Drahos A, Nowack T, Fitzgerald M, Christie DB. Longterm postoperative hardware complications after open rib fixation. Am Surg 2018;Aug;84:e317–9. ArticlePubMedPDF
- 28. Choi J, Kaghazchi A, Sun B, Woodward A, Forrester JD. Systematic review and meta-analysis of hardware failure in surgical stabilization of rib fractures: who, what, when, where, and why. J Surg Res 2021;268:190–8. ArticlePubMed
- 29. Marasco SF, Sutalo ID, Bui AV. Mode of failure of rib fixation with absorbable plates: a clinical and numerical modeling study. J Trauma 2010;68:1225–33. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Komplikationen nach operativer vs. konservativer Versorgung des schweren Thoraxtraumas
Lars Becker, Marcel Dudda, Christof Schreyer
Die Unfallchirurgie.2024; 127(3): 204. CrossRef
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite