Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Original Article
One year of treating patients with open fractures of the lower extremity in a new military trauma center in Korea: a case series -
Ji Wool Ko, MD1
 , Giho Moon, MD2
, Giho Moon, MD2 , Jin Geun Kwon, MD3
, Jin Geun Kwon, MD3 , Kyoung Eun Kim, MD4
, Kyoung Eun Kim, MD4 , Hankaram Jeon, MD5
, Hankaram Jeon, MD5 , Kyungwon Lee, MD1
, Kyungwon Lee, MD1
-
Journal of Trauma and Injury 2023;36(4):376-384.
DOI: https://doi.org/10.20408/jti.2023.0041
Published online: December 19, 2023
- 418 Views
- 17 Download
1Department of Surgery, Korea University Guro Hospital, Seoul, Korea
2Department of Orthopedic Surgery, Armed Forces Capital Hospital, Seongnam, Korea
3Department of Plastic Surgery, Armed Forces Capital Hospital, Seongnam, Korea
4Department of Rehabilitation, Armed Forces Capital Hospital, Seongnam, Korea
5Department of Psychiatry, Armed Forces Capital Hospital, Seongnam, Korea
- Correspondence to Kyungwon Lee, MD Department of Surgery, Korea University Guro Hospital, 148 Gurodong-ro, Guro-gu, Seoul 08308, Korea Tel: +82-31-789-2814 Email: enmma23@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- The Armed Forces Trauma Center of Korea was established in April 2022. This study was conducted to report our 1-year experience of treating soldiers with open fractures of the lower extremity.
-
Methods
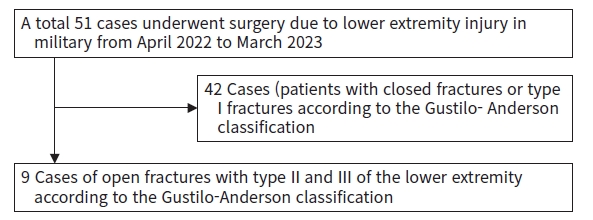
- In this case series, we reviewed the medical records of 51 Korean soldiers with open fractures of the lower extremity between April 2022 and March 2023 at a trauma center. We analyzed patients with Gustilo-Anderson type II and III fractures and reported the duration of transportation, injury mechanisms, injured sites, and associated injuries. We also presented laboratory findings, surgery types, intensive care unit stays, hospital stays, rehabilitation results, and reasons for psychiatric consultation. Additionally, we described patients’ mode of transport.
-
Results
- This study enrolled nine male patients who were between 21 and 26 years old. Six patients had type II and three had type III fractures. Transport from the accident scene to the emergency room ranged from 75 to 455 minutes, and from the emergency room to the operating room ranged from 35 to 200 minutes. Injury mechanisms included gunshot wounds, landmine explosions, grenade explosions, and entrapment by ship mooring ropes. One case had serious associated injuries (inhalation burn, open facial bone fractures, and hemopneumothorax). No cases with serious blood loss or coagulopathies were found, but most cases had a significant elevation of creatinine kinase. Two patients underwent vascular reconstruction, whereas four patients received flap surgery. After rehabilitation, six patients could walk, one patient could move their joints actively, and two patients performed active assistive movement. Eight patients were referred to the psychiatry department due to suicidal attempts and posttraumatic stress disorder.
-
Conclusions
- This study provides insights into how to improve treatment for patients with military trauma, as well as medical services such as the transport system, by revising treatment protocols and systematizing treatment.
- Background
- Korea has been in a state of ceasefire for 70 years since the end of the Korean War in 1953. The Korean military maintains 500,000 soldiers, accounting for about 1% of the Korean population in the present day [1]. Accidents such as landmine explosions, gunshots, and falls during training can occur in the military. Lower extremity injuries are especially common in the military due to soldiers’ training and exercise to maintain their physical condition. Patients with lower extremity injuries are usually hospitalized for a long time because their activity level is limited [2]. In addition, severe lower extremity injuries occasionally occur. Those with multiple severe injuries often show unstable vital signs and undergo repeated operations with considerable complications and psychological problems [3].
- Objectives
- The Armed Forces Trauma Center (AFTC; Seongnam, Korea) was established in April 2022. This study was conducted to report our 1-year experience of treating patients (soldiers) with open fractures of the lower extremity. In addition, the clinical processes of treating these patients were described in detail.
INTRODUCTION
- Ethics statement
- This study was approved by the Institutional Review Board of Armed Forces Capital Hospital (No. AFCH 2023-04-001). The requirement for informed consent was waived due to the retrospective nature of the study.
- Study design
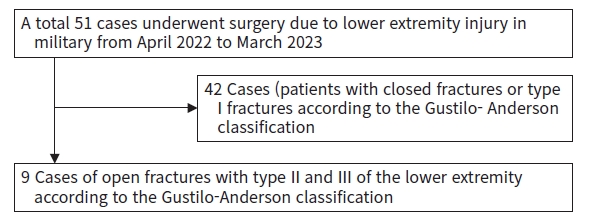
- In this observational study (case series), we reviewed the medical records of 51 Korean soldiers with open fractures of the lower extremity between April 2022 and March 2023 at a single trauma center.
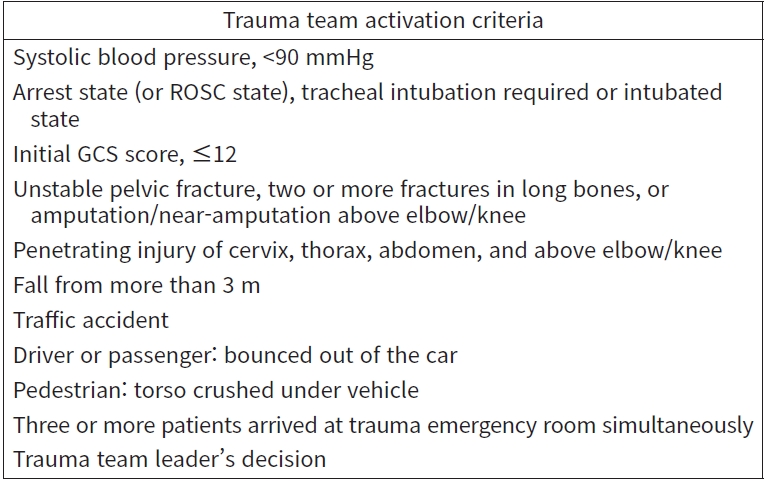
- After categorizing the severity using the Gustilo-Anderson classification, we analyzed patients with type II and III fractures (Fig. 1) [4]. The process of transporting patients was described as time elapsed from the accident scene to the emergency room (ER) and from the ER to the operating room (OR). We analyzed the patients’ injury mechanisms, injured sites, types of surgery performed, associated injuries, and clinical processes. The injury mechanisms included gunshot wounds, landmine explosions, grenade explosions, being crushed under a vehicle wheel, being trapped by mooring ropes, and falls. We classified the injured sites as pelvis, thigh (femur), knee, calf (tibiofibular), ankle, and foot. The surgeries performed were bony fixation, vascular reconstruction, and performing flap. We also reported the associated injuries of these patients and calculated the Injury Severity Score (ISS), Revised Trauma Score (RTS), and Trauma and Injury Severity Score (TRISS) for each case. We presented the initial laboratory findings upon arrival at the ER and clinical processes such as intensive care unit (ICU) stays, hospital stays, rehabilitation results, and reasons for referral to the psychiatry department for consultation.
- Processes for responding to military trauma patients
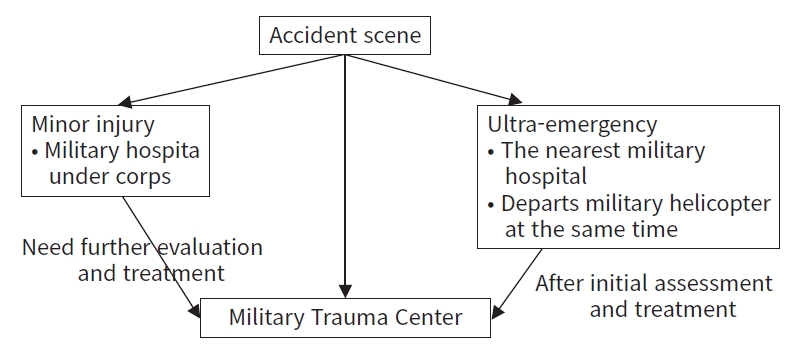
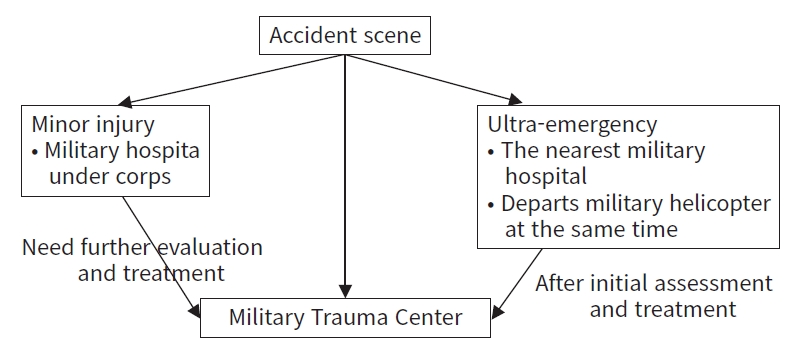
- Almost all military servicepersons who require transportation to a hospital are immediately reported to the Medical Emergency Operation Center (MEOC) under the Korean Armed Forces Medical Command (Fig. 2). The MEOC offers on-site counseling and treatment, determines the appropriate hospital (military or civilian) for patients, and prepares a transport strategy using military or civilian vehicles or helicopters. Among them, patients with traumatic injuries requiring surgical or intensive management are usually transported to the AFTC after discussion with the MEOC.
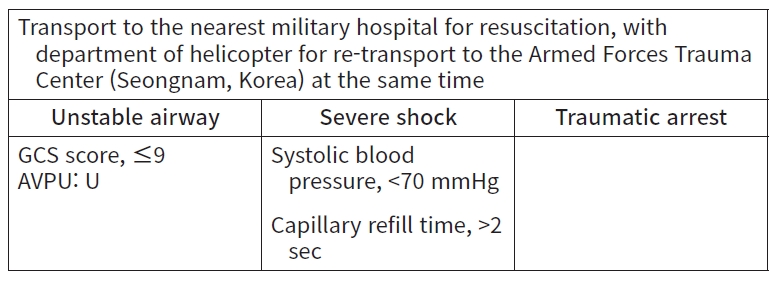
- Fig. 3. shows the field triage protocol for trauma patients. Patients with minor injuries are transported to military hospitals under corps. Ultra-emergency patients who have an unstable airway, severe shock, and traumatic arrest (Fig. 4) are transported to the nearest military hospital for initial resuscitation. The helicopters depart at the same time, and then patients are re-transported to the AFTC after resuscitation. Exceptionally, by the MEOC decision, patients are sometimes transported to the nearest civilian trauma center. Patients with major injuries (Fig. 5) are also transported to the AFTC.
- A total of 11 trauma surgeons work in the AFTC. Four are military officers, six are civilians who were dispatched from a cooperative hospital, and one is a civilian surgeon employed by the military. This center is part of the biggest military hospital in Korea, with 666 beds and 130 doctors (excluding residents). Physicians affiliated with this military hospital support the AFTC, including surgeons (thoracic, orthopedic, plastic, vascular, hepatobiliary, and neurosurgeons), interventionists, anesthesiologists, cardiologists, pulmonologists, neurologists, physiatrists, psychiatrists, and so on.
- The AFTC is a three-story building with a helipad on the roof, which is designated as the shortest distance by foot (Fig. 6A). The ground floor includes a trauma ER with two resuscitation rooms (Fig. 6B), a computed tomography (CT) room, a magnetic resonance room, and an intervention room. The first floor includes offices and educational rooms. The second floor includes a trauma OR (Fig. 6C), a general ward for trauma patients with 60 beds, and a trauma ICU (TICU) with 20 beds (Fig. 6D).
- One or more trauma surgeons are on duty all the times in the AFTC. Trauma surgeons respond to patients’ arrival at the trauma ER, apply critical care in the TICU, participate in surgery, and operate the trauma general ward. When the MEOC contacts the AFTC trauma team leader (a trauma surgeon) for patient transportation, the team leader decides whether to accept the patient, and then whether to activate the trauma team following standard criteria (Fig. 7). The trauma team consists of trauma surgeons (including the trauma team leader), trauma ER nurses, emergency medical technicians, radiology technicians, and security guards. The trauma team leader can also call for additional staff affiliated with the supporting military hospital, such as surgeons from other departments, anesthesiologists, and interventionists. When trauma patients arrive at the AFTC, trauma surgeons assess and resuscitate them if needed, together with trained nurses assigned to the trauma ER. They then discuss the treatment plan with supporting staff members. In the trauma ER, protocols are in place for CT scans, transfusion, laboratory studies, and performing necessary procedures.
METHODS
Data collection
Criteria and variables
Transportation system for trauma patients in the Korean military
AFTC workforce and building structure
AFTC treatment protocols
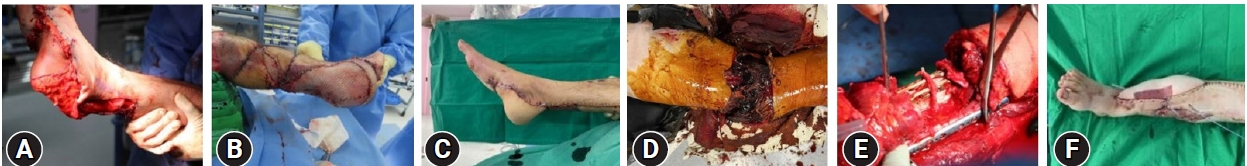
- Table 1 shows the transportation processes of patients from the accident site to the AFTC ER, along with their demographics. This study included nine male patients aged between 21 and 26 years old. Five patients were transported directly to the AFTC (cases 1, 2, 4, 5, 7), and four patients (cases 3, 6, 8, 9) were transferred to the center through another hospital. Military trauma patients can be transported in four ways: military helicopter, military ambulance, public helicopter, public ambulance. In this study, four patients were transported by military helicopter, four patients by military ambulance, and one patient by public helicopter. The time it took to transport patients from the accident scene to the AFTC ER ranged from 75 minutes (case 4) to 455 minutes (case 9), and from the ER to the OR ranged from 35 minutes (case 4) to 200 minutes (case 6). Cases that went through another hospital (cases 4, 6, 8, 9) took more time to transport. Among them, military-specific injuries included gunshot wounds (cases 1, 3), landmine explosions (cases 2, 5) (Fig. 8A–C), a grenade explosion (case 4), and entrapment by a warship’s mooring ropes (case 7) (Fig. 8D–F). The foot was the most common site of injury, and only one patient (case 4) had serious associated injuries (namely, an inhalation burn, open facial bone fractures, and hemopneumothorax with multiple rib fractures). Systolic blood pressure, ISS, Revised Trauma Score, and TRISS were not unusually low except in one case (case 4).
- Table 2 displays the initial laboratory findings upon arrival at the ER. No cases with serious blood loss (hemoglobin, <7.0 g/dL) or coagulopathies were found. Most cases showed a significant elevation of creatinine kinase (316–2,876 IU/L), except for cases 3 and 5, which were within normal range.
- Table 3 shows the operative methods used. The patients in cases 4 and 7 underwent vascular reconstruction, and the patients in cases 2, 4, 5, and 7 received external fixation during their initial surgery. The patients in cases 4, 5, 7, and 8 underwent flap surgery.
- Table 4 shows hospitalization-related variables. Case 4, a patient with multiple injuries, remained in the ICU for 169 days due to requiring long-term ventilator care and management of serious infections. Patients who required rehabilitation for an extended period were hospitalized for more than 16 weeks (cases 1, 2, 4, 5, 7, 8, 9). The results of rehabilitation were as follows: the patients in cases 1, 2, 3, 6, 8, and 9 were able to walk; the patient in case 5 was able to perform active joint movements; and the patients in cases 4 and 7 were able to perform active assistive joint movements. Eight patients in this study required referral to the psychiatry department. Four of these patients had suicidal ideation; those patients had injuriess caused by suicide attempts (cases 3, 4, 8, and 9). Their suicidal ideation were addressed following the accidents. All eight patients had posttraumatic stress disorder (PTSD).
RESULTS
- Transportation processes
- When a patient with traumatic injuries (or other serious illness) occurs, the military tries to choose the fastest transportation method. Helicopters are very useful for the military because military camps are scattered throughout the country. However, helicopter operations are limited by inclement weather, including rainy, snowy, severely windy, and foggy conditions. Additionally, military helicopters are not able to operate near the ceasefire line, since it could cause military tension. When it is difficult for the MEOC to operate a helicopter and when they suspect that a patient’s injury is serious, they arrange transportation to a nearby military or civilian hospital. After evaluation and (if needed) resuscitation, MEOC discusses the situation with AFTC medical staff and decides whether to transfer the patient to the AFTC.
- Characteristics of military trauma
- Several cases in this study included military-specific injuries unusual in civilian society, such as gunshot wounds, landmine explosions, grenade explosions, and entrapment by a warship’s mooring ropes. Additionally, there were cases of military-specific injuries caused by pinching a foot between a cannon and a cannonball, crashing a parachute, and falling from a military helicopter. These cases occurred during the study period but were excluded since they involved closed fractures of the lower extremity. Crashing injuries caused by heavy military equipment, such as moving tanks, cannons, helicopters, and warships, should be taken seriously. In addition, the medical staff of a military trauma center should understand the characteristics of various weapons. For example, even blank cartridge shot can cause severe injury due to the gunpowder blast and projectile gas [5,6]. Grenade explosions can cause whole-body injury by countless fragments with burns, including to the airway [7].
- No case of serious blood loss (hemoglobin, <7.0 g/dL) and coagulopathy was observed in this study because military medical officers were able to control bleeding well at the accident scenes. Additionally, the AFTC ICU, which is separated into single-occupancy rooms, could help patients maintain a comfortable state and enable monitoring of possible self-injury and abnormal behaviors. Patients with suicidal attempts or a concerning level of PTSD who require repeated surgery are admitted to the ICU until ready for a closed psychiatric ward or until their psychiatric problems become less concerning.
- Treatment strategies for open fractures in lower extremities
- Trauma patients should be considered in two aspects: (1) the severity of the injured site; and (2) possible life-threatening associated injuries. Aspects of the military context contribute to fractures in many patients. This is natural because soldiers undergo high-intensity training, exercise regularly, and often participate in hazardous tasks such as landmine removal. Most patients experience minor injuries, but some cases are very serious, such as limb injuries with degloving, severe associated injuries, or both [8,9]. Many cases involve injuries from which patients find it difficult to achieve a full recovery. The treatment of these patients requires a strategy consisting of several steps.
- The first step is to decide whether to salvage or sacrifice the injured leg. Trying to salvage the injured limb may require repeated operations, cause serious complications (such as infection, thrombosis, and chronic pain), impose a huge financial burden, and delay rehabilitation. For many patients with severe leg injuries, amputation might be a better option [10,11]. Patients admitted to the AFTC have their medical expenses covered by the military, and most soldiers, such as military officers and sergeants who suffered disabilities from accidents on duty, can keep their jobs postinjury and are paid during the treatment period. Therefore, we tried our best to salvage the leg in each case, since we could focus on saving the leg without worrying about time or cost [12]. In this study, no cases involved amputation of a lower limb.
- The second step is to manage concurrent injuries that could have adverse effects. Life-threatening injuries such as those affecting the brain, heart, lungs, liver, and large vessels are treated with priority.
- The third step is to perform surgery. OR decisions were made according to the injury mechanism, injured site, general condition, and the surgeon’s experience, including their skill level [13,14]. During operations, surgeons must solve problems such as vascular reconstruction, muscle repairing, and overlapping skin defects. The most crucial point for surgeons is planning. Surgeons should plan what may be feasible, up to a certain limit of reconstruction, if the injury is too serious to permit a full recovery. In particular, landmine explosions can cause serious intimal injuries that make it difficult to reconstruct vascular structures and create flaps for covering defective tissue. We tried to salvage limbs as much as possible, since most patients in this study were young, otherwise healthy soldiers.
- The fourth step is to perform rehabilitation, which may take a long time [15,16]. The timing for initiating rehabilitation depends on many factors such as how the fracture heals, the fixation method, and how related ligaments heal. The rehabilitation process typically begins with restrictive weight bearing, followed by a range of motion evaluation, continuous passive motion, and finally muscle strengthening exercises [17]. Appropriate pain control is needed across the rehabilitation period. Moreover, addressing psychological problems is the most difficult part of recovery [18–20]. Many patients have PTSD, and a psychiatrist’s active involvement is required if the cause of injury is self-harm or a suicidal attempt. In conclusion, management of lower extremity injuries requires complex processes. This study has shown our experiences and management policy for lower extremity injuries in a new military trauma center, which could be useful for other trauma centers that manage lower extremity injuries.
- Strengths and limitations
- The strengths of this study include its analysis of data based on a specialized transporting system and treatment strategies for military trauma patients. We were able to observe the entire period of treatment from initial ER management to rehabilitation. However, this study has several limitations. First, the volume of the data was small because the AFTC was established only 1 year ago. Second, it is difficult to evaluate the relevance of intensive care, since there was only one case (case 4) with life-threatening associated injuries.
- Conclusions
- This study showed the experiences of treatment in patients with lower extremity injuries in the military. We hope that the study may help improve treatment in patients with military trauma, as well as improve military medical services such as the transport system, in order to revise treatment protocols and systematize treatment during hospitalization.
DISCUSSION
-
Author contributions
Conceptualization: KL; Data curation: all authours; Formal analysis: JWK, KL; Investigation: all authours; Methodology: KL; Project administration: KL; Visualization: JWK, KL; Writing–original draft: JWK, KL; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION



| Case no. | Age (yr) | Sex | Transferred from another hospital | Mode of transport |
Elapsed time (min) |
Injury mechanism | Injured site | Severitya) | Associated injury | SBP (mmHg) | ISS | RTS | TRISS (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| From accident site to AFTC ER | From ER to OR | |||||||||||||
| 1 | 22 | Male | No | Military ambulance | 305 | 85 | Gunshot | Foot | II | None | 124 | 4 | 7.550 | 98.40 |
| 2 | 22 | Male | No | Military helicopter | 115 | 80 | Landmine explosion | Ankle, foot | II | Multiple lacerations | 144 | 5 | 7.841 | 99.58 |
| 3 | 26 | Male | Military hospital | Military helicopter | 120 | 75 | Gunshot | Foot | II | None | 162 | 4 | 7.841 | 99.28 |
| 4 | 24 | Male | No | Military helicopter | 75 | 35 | Grenade explosion | Foot, bilateral | IIIc | Inhalation burn, open facial bone fractures, hemopneumothorax with multiple rib fractures | 96 | 50 | 7.841 | 84.74 |
| 5 | 23 | Male | No | Military helicopter | 85 | 40 | Landmine explosion | Ankle, foot | IIIb | None | 114 | 4 | 7.841 | 99.61 |
| 6 | 21 | Male | Civilian hospital | Military ambulance | 405 | 200 | Crushed under vehicle wheel | Foot | II | None | 143 | 4 | 7.841 | 99.61 |
| 7 | 25 | Male | No | Public helicopter | 135 | 70 | Trapped by mooring ropes | Calf (tibiofibular) | IIIc | Rib fracture, multiple lacerations | 83 | 11 | 7.108 | 98.76 |
| 8 | 23 | Male | Civilian hospital | Military ambulance | 390 | 70 | Fall | Thigh (femur), ankle, foot | II | Multiple lacerations | 115 | 10 | 7.841 | 99.12 |
| 9 | 21 | Male | Civilian hospital | Military ambulance | 455 | 90 | Fall | Foot | II | Lumbar spine compression fracture | 120 | 13 | 7.841 | 99.19 |
| Case no. |
Length of stay (day) |
Results of rehabilitation | Reason for psychiatric consultation | |
|---|---|---|---|---|
| Intensive care unit | Hospitala) | |||
| 1 | 13 | 216 | Able to walk | PTSD |
| 2 | 4 | 243 | Able to walk | PTSD |
| 3 | 4 | 46 | Able to walk | Suicide attempt, PTSD |
| 4 | 169 | 335 | Active assistive joint movement | Suicide attempt, PTSD |
| 5 | 29 | >271b) | Active joint movement | PTSD |
| 6 | 0 | 70 | Able to walk | None |
| 7 | 13 | >181b) | Active assistive joint movement | PTSD |
| 8 | 13 | >132b) | Able to walk | Suicide attempts, PTSD |
| 9 | 11 | 130 | Able to walk | Suicide attempts, PTSD |
- 1. Korean Ministry of National Defense. 2022 Defense white paper. Korean Ministry of National Defense; 2023.
- 2. Higgins TF, Klatt JB, Beals TC. Lower Extremity Assessment Project (LEAP): the best available evidence on limb-threatening lower extremity trauma. Orthop Clin North Am 2010;41:233–9. ArticlePubMed
- 3. Balandiz H, Bolu A. Forensic mental health evaluations of military personnel with traumatic life event, in a university hospital in Ankara, Turkey. J Forensic Leg Med 2017;51:51–6. ArticlePubMed
- 4. Hu R, Ren YJ, Yan L, et al. Analysis of staged treatment for Gustilo Anderson IIIB/C open tibial fractures. Indian J Orthop 2018;52:411–7. ArticlePubMedPMCPDF
- 5. Lee H, Hwang K, Lee Y, Jeong SY. Survival of a blank cartridge gunshot injury to the soft palate in a soldier. J Craniofac Surg 2022;33:e573–6. ArticlePubMed
- 6. Kim HJ, Lee D, Lee K. Submandibular injury caused by the close-range firing of a military blank cartridge shot. J Acute Care Surg 2023;13:35–38. ArticlePDF
- 7. Robson DC. Death from an anti-personnel grenade explosion. J R Army Med Corps 1983;129:115–6. ArticlePubMed
- 8. Dehouche N. The injury severity score: an operations perspective. BMC Med Res Methodol 2022;22:48. ArticlePubMedPMCPDF
- 9. Bothig R. TRISS: a method of assessment of the prognosis in multiple trauma patients. Zentralbl Chir 1991;116:831–44. PubMed
- 10. Okereke I, Abdelfatah E. Limb salvage versus amputation for the mangled extremity: factors affecting decision-making and outcomes. Cureus 2022;14:e28153ArticlePubMedPMC
- 11. McGowan SP, Fallahi AK. Degloving injuries. StatPearls Publishing; 2023.
- 12. Korean Ministry of National Defense; Korea Law Translation Center. Military Accident Compensation Act [Internet]. Korea Legislation Research Institute; 2023 [cited 2023 Jun 1]. Available from: https://elaw.klri.re.kr/eng_service/lawView.do?hseq=60445&lang=ENG.
- 13. Xu Q, Zhu L, Wang G, et al. Application of cryopreserved autologous skin replantation in the treatment of degloving injury of limbs. J Plast Reconstr Aesthet Surg 2022;75:2387–440. Article
- 14. Yan H, Gao W, Li Z, et al. The management of degloving injury of lower extremities: technical refinement and classification. J Trauma Acute Care Surg 2013;74:604–10. PubMed
- 15. Kaya D, Guney-Deniz H, Sayaca C, Calik M, Doral MN. Effects on lower extremity neuromuscular control exercises on knee proprioception, muscle strength, and functional level in patients with ACL reconstruction. Biomed Res Int 2019;2019:1694695. ArticlePubMedPMCPDF
- 16. McKeon PO, Fourchet F. Freeing the foot: integrating the foot core system into rehabilitation for lower extremity injuries. Clin Sports Med 2015;34:347–61. PubMed
- 17. Hoyt BW, Pavey GJ, Pasquina PF, Potter BK. Rehabilitation of lower extremity trauma: a review of principles and military perspective on future directions. Curr Trauma Rep 2015;1:50–60. ArticlePDF
- 18. Al Salman A, Khatiri MZ, Cremers T, Ring D, Thomas JE, Fatehi A. Difficult life events affect lower extremity illness. Arch Orthop Trauma Surg 2022;142:599–605. ArticlePubMedPDF
- 19. Archer KR, Davidson CA, Alkhoury D, et al. Cognitive-behavioral-based physical therapy for improving recovery after traumatic orthopaedic lower extremity injury (CBPT-Trauma). J Orthop Trauma 2022;36:S1–7. Article
- 20. McCarthy ML, MacKenzie EJ, Edwin D, et al. Psychological distress associated with severe lower-limb injury. J Bone Joint Surg Am 2003;85:1689–97. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite