ABSTRACT
-
Purpose
- Trauma is the top cause of death in people under 45 years of age. Deaths from severe trauma can have a negative economic impact due to the loss of people belonging to socio-economically active age groups. Therefore, efforts to reduce the mortality rate of trauma patients are essential. The purpose of this study was to investigate preventable mortality in trauma patients and to identify factors and healthcare-related challenges affecting mortality. Ultimately, these findings will help to improve the quality of trauma care.
-
Methods
- We analyzed the deaths of 411 severe trauma patients who presented to Gachon University Gil Hospital regional trauma center in South Korea from January 2015 to December 2017, using an expert panel review.
-
Results
- The preventable death rate of trauma patients treated at the Gachon University Gil Hospital regional trauma center was 8.0%. Of these, definitely preventable deaths comprised 0.5% and potentially preventable deaths 7.5%. The leading cause of death in trauma patients was traumatic brain injury. Treatment errors most commonly occurred in the intensive care unit (ICU). The most frequent management error was delayed treatment of bleeding.
-
Conclusions
- Most errors in the treatment of trauma patients occurred in early stages of the treatment process and in the ICU. By identifying the main causes of preventable death and errors during the course of treatment, our research will help to reduce the preventable death rate. Appropriate trauma care systems and ongoing education are also needed to reduce preventable deaths from trauma.
-
Keywords: Regional trauma center; Severe trauma; Preventable death rate
INTRODUCTION
- According to the Korean National Statistical Office, deaths from trauma accounted for about 10%, or 27,154, of the total of 280,000 deaths in Korea in 2016. Notably, trauma was the top cause of death in people under 45 years of age [1]. Deaths or serious injuries resulting from trauma have a negative impact on society, because of the loss of young people who are the most active in social and economic activities, restrictions on return to daily life due to post-injury disability, and consequent reduced productivity. Several studies have estimated the cost of productivity loss at about 350 million Korean won per death due to trauma. The mortality rate of trauma patients must be lowered to reduce the public burden of these costs [2-5].
- Treatment for severe trauma patients requires hospital personnel, including specialist surgeons and anesthesiologists, and facilities such as operating rooms, intensive care units (ICUs), and essential medical equipment. Therefore, in developed countries such as the United States, systems for the treatment of severe trauma patients are mostly operated by local or state governments. In the United States, verified trauma centers began to be established in the 1970s and currently a trauma surveillance program facilitates information exchange between trauma centers operated by each region or state [5]. In 2012, the Ministry of Health and Welfare began to establish regional trauma centers in Korea, with the goal of providing optimal treatment 24 hours a day, 365 days a year, such as emergency surgery for severe trauma patients upon arrival at the hospital. Trauma centers must have a resuscitation room, a radiology room, an ICU, and an operating room for the treatment of trauma patients, which function independently of existing facilities. Thirteen institutions that meet these standards are currently in operation.
- Preventable death corresponds to cases in which a patient who died from trauma would probably have lived had he or she been in the right hospital at the right time and received optimal treatment. According to a 2011 survey, the preventable mortality rate from trauma in Korea was 35.2% [6], with major causes of injury being traffic accidents and falls [7]. The leading cause of death in trauma patients was head injury, followed by bleeding and multiple organ failure [7]. Studies in the United States suggested that with appropriate trauma systems in place, preventable mortality can be reduced to 4.2%. Along with recently-reported preventable mortality rates of 5.2% and 2.4% in Scandinavia and California, respectively, this suggests that Korea has not managed trauma patients as effectively as other countries [8-11].
- The purpose of this study is to investigate the preventable mortality rate of trauma patients who died at Gachon University Gil Hospital regional trauma center from 2015 to 2017 and to identify factors that contributed to these deaths. This information would identify shortcomings in the current management of trauma patients and help improve the quality of trauma care in Korea.
METHODS
- Ethical approval was obtained from the Institutional Review Board (IRB) of Gachon University Gil Hospital (IRB No. GDIRB2020-366). Human subjects were not identified in the description, tables, and figures in this article. Hence, written informed consent was not needed.
- Research site
- Gachon University Gil Hospital is a university hospital with more than 1,500 beds in Incheon. In 2014, it was established as the first regional trauma center in Incheon. The number of trauma-related hospitalizations is more than 3,000 per year, of which about 500 to 550 patients are severe trauma patients with an Injury Severity Score (ISS) of 15 or more. The trauma center is dedicated to trauma patients only and has two resuscitation and operating rooms, 20 ICU beds, 19 trauma surgeons, four trauma coordinators, and 11 trauma nurses. Emergency medicine specialists, anesthesiologists, and neurosurgeons, although not exclusive to the trauma center, form part of the team and respond to calls as needed.
- Research subjects
- The subjects of this study were severe trauma patients who died during treatment at the Gachon University Gil Hospital regional trauma center between January 2015 and December 2017. Trauma was defined as physical injury caused by traffic accidents (cars, bicycles, motorcycles, etc.), falls, slips, blunt injury and penetrating injury. Patients who were dead on arrival and did not undergo cardiopulmonary resuscitation, or who died of disease, burns, drowning, and poisoning were excluded. The data used for analysis were extracted from the Korea Trauma Database and the electronic medical records of the Gachon University Gil Hospital regional trauma center.
- Research procedure
- Based on the medical records of trauma patients who died, preventable mortality was determined by an expert panel discussion that established for each case the probability of death and the cause of death. The panel consisted of one emergency medicine specialist, three trauma surgeons, and one neurosurgery specialist at Gachon University Gil Hospital regional trauma center. The final judgment of preventable mortality was decided through a deliberative process, in which the preventable mortality rate was not simply determined through a majority vote, but instead a judgement was made based on a discussion among the panelists in which opinions were revised.
- Panelists judged subjectively whether death could have been prevented, considering the patient’s condition, the mechanism of injury, the time interval between arrival and death, the cause of death, the occurrence of inter-hospital transfer, and the treatment received in the hospital. Preventable deaths were defined as those that would have been prevented had the trauma patient been transferred to the appropriate hospital promptly and received optimal treatment. The panel defined definitely preventable (DP) deaths as those for which the panelists rated the likelihood of survival under optimal conditions to be greater than 75%, potentially preventable (PP) deaths as those with a likelihood of survival rated between 25% and 75%, and non-preventable (NP) deaths as those for which the likelihood of survival was less than 25%. The final preventable mortality was the sum of DP and PP.
- To complement the subjective panel evaluation and facilitate a comparison with other preventable mortality studies, we also used the Trauma and Injury Severity Score (TRISS) [12] scoring system to assess the severity of trauma and compared this with the panel’s evaluation. The TRISS calculates the patient’s probability of survival (Ps) using three variables: the ISS [13], the Revised Trauma Score (RTS) [12], and the patient’s age, as follows:
- Ps=1/(1+e-b)
- For blunt trauma, b=-0.4499-(0.0835×ISS)+ (0.8085×RTS)-(1.7430×age)
- For penetrating trauma, b=-2.5355-(0.0651×ISS)+ (0.9934×RTS)-(1.1360×age)
RESULTS
- Clinical characteristics of patients included in the study
- Among the 9,988 patients who were treated at the regional trauma center during the investigation period, the total number of trauma-related deaths was 443. The clinical characteristics of these patients are shown in Table 1. Preventable mortality was analyzed in 411 of these patients, after excluding 32 patients who were dead at the time of admission. The panel review found that the total preventable mortality rate was 8%, of which two deaths were DP (0.5%) and 31 PP (7.5%) (Fig. 1).
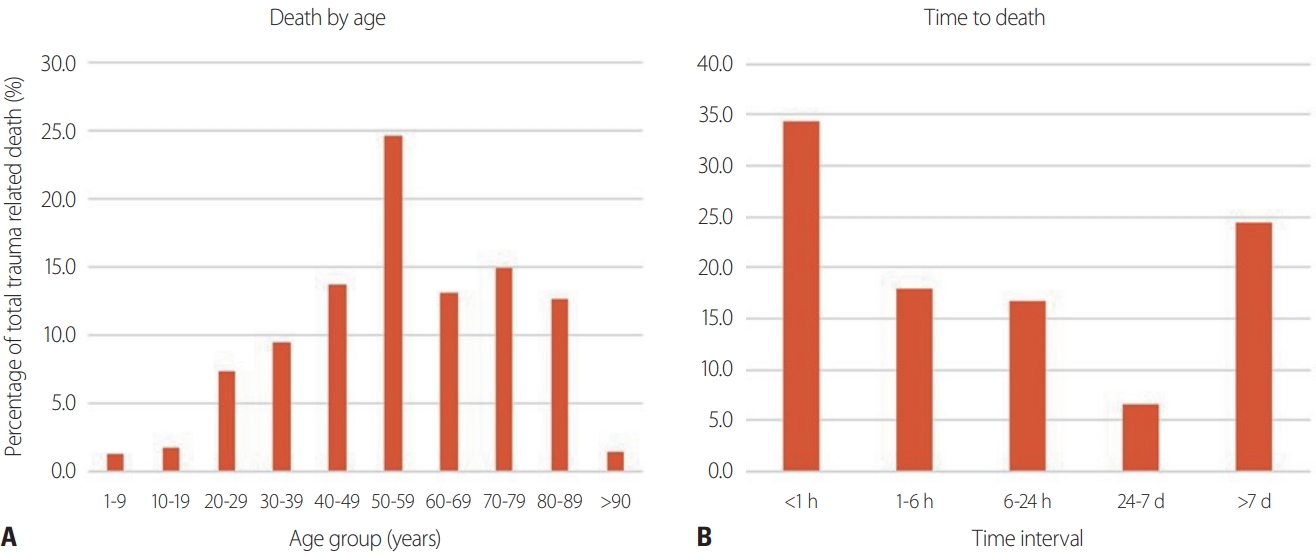
- Most patients who died of severe trauma were in their 50s, and elderly patients aged 70 or older accounted for about one-third of deaths. The average patient age was 56 years and the proportion of males (69.6%) was 2.3 times higher than females. The mechanism of most injuries was blunt trauma (96.0%). The median systolic blood pressure was 37 mmHg, median heart rate was 65 beats/minute, and median ISS was 22. The median probability of survival under optimal treatment conditions by TRISS was 16%, and 26.8% of patients were transferred from other hospitals. Most deaths occurred within 1 hour of arrival at the trauma center, and the next greatest proportion of deaths occurred 7 or more days after arrival (Fig. 2).
- Factors affecting preventable death
- Factors that potentially affect preventable mortality are presented in Table 2. Among the 233 patients with a known cause of death, traumatic brain injury was the most common cause, followed by massive bleeding and multiple organ failure. The majority of deaths from traumatic brain injury were non-preventable (95.3%). Among bleeding patients, 15.6% of deaths were preventable, and 37.5% of the deaths from multiple organ failure were preventable.
- Of the 411 deaths, 13 were excluded from the TRISS score calculation due to a lack of data, and 53% of the remaining 398 patients had a Ps of less than 25%. Although there were five preventable deaths with a Ps of less than 25%, the majority of preventable deaths had a Ps of greater than 50%.
- Treatment shortcomings
- Because some deaths were the result of more than one error, a total of 42 errors were identified in 33 preventable deaths. As presented in Table 3, the most frequent error type was delayed treatment for bleeding (30.9%). Delayed management of abdominal and pelvic bleeding and delayed management of chest bleeding each contributed 11.9% to this total. The next most frequent errors were faults in the treatment decision-making process (21.4%), followed by failure to prevent deep vein thrombosis and pulmonary embolism (9.5%), improper management in the ICU (9.5%), and failure to diagnose abdominal trauma (9.5%).
DISCUSSION
- Preventable mortality rates have been used in the United States and the United Kingdom since the 1960s to assess the outcome and level of trauma care [14]. In Korea, a total of four preventable mortality studies were conducted between 1997 and 2011. The preventable mortality rate in 1997 was 40.5%, which decreased to 39.6% in 2003 and 32.6% in 2006, and rose slightly to 35.2% in 2009 [6,7,15,16]. In the current study, the preventable mortality rate was 8%, and 6.2% of preventable deaths were DP (with a likelihood of survival higher than 75%), while 93.8% were PP (with a 25–75% likelihood of survival). Although this is substantially lower than the preventable mortality rate of 35.2% found by the Korean Ministry of Health and Welfare survey in 2011, it is still higher than the 2.4% preventable mortality rate in California in the United States in 2006 [11].
- Estimates of preventable mortality can, however, vary depending on the method of investigation and analysis. The preventable mortality rate tends to be highest when using expert consensus judgment, in which a decision is reached when at least one panelist judges that death was preventable [17]. The preventable mortality rate assessed via the deliberative process in this study may therefore have been higher if the expert consensus judgment method had been used [17]. In contrast, the use of autopsy in a given patient group reduces the estimated preventable mortality rate compared with the use of hospital records alone [18]. Since autopsies are rarely performed in Korea, the preventable mortality rate is likely to be overestimated compared to that of other countries.
- We found that traumatic brain injury was the leading cause of traumatic death, accounting for 55% of all trauma-related deaths; however, 95.3% of them were NP, with less than a 25% chance of survival. The leading causes of preventable death (DP and PP) were multiple organ failure and massive bleeding. It has been found that rapid hemostasis reduces the risk of death from hemorrhage, and thereby markedly lowers the mortality rate of trauma patients [19]. The same study found that only 15.6% of patients with massive bleeding had a 25% or lower probability of survival.
- To reduce preventable mortality, it is therefore important to have a system that enables bleeding patients to receive the appropriate treatment promptly. In fact, we found that delayed treatment for bleeding was the most common management problem contributing to preventable death. Specifically, there were cases where surgery was delayed to perform a computed tomography scan or an angiogram was delayed in a hemodynamically unstable patient. To address this type of error, in 2017 the National Central Medical Center developed standard trauma treatment guidelines and trained staff on the management and imaging of hypovolemic shock in trauma patients.
- To reduce common treatment errors, including incorrect treatment decision-making, failure to prevent of deep vein thrombosis and pulmonary embolism, and failure to diagnose abdominal trauma, regular training of trauma staff and quality of care monitoring are needed.
- During trauma patient care, 31% of errors occurred in the ICU and improper treatment in the ICU accounted for 9.5% of preventable deaths. In addition, a quarter of management errors occurred in general wards. This means that patient management systems, including appropriate protocols, education, and monitoring, are needed. Twenty-nine percent of problems occurred at the emergency department stage, which, although high, is lower than the proportion of 52.3% reported in previous studies [7]. This is because the quality of the initial treatment was improved by using the trauma resuscitation zone instead of the emergency room and assigning a dedicated trauma specialist.
- According to a study conducted in the United States, when patients with traumatic brain injury were transferred to a trauma center from another hospital, the mortality rate 2 weeks after the injury was about 50% higher than when patients presented to the trauma center directly [20]. In the current study, more than 25% of all patients arrived at the trauma center via other hospitals. Pre-hospital severity classification is not yet well performed in Korea. Notably, 14% of errors occurred at the pre-hospital stage, and inadequate care at the inter-hospital transfer stage accounted for 4.8% of preventable deaths. However, these figures are based on incomplete pre-hospital information and the pre-hospital preventable mortality rate may have been higher had more detailed data been available for analysis. Therefore, further analysis and in-depth investigation of pre-hospital mortality is needed.
- Several limitations of this study should be noted. First, this was a retrospective study using trauma data from deceased patients. The clinical characteristics of trauma patients, such as underlying disease and age, may bias the results, and the exact cause of death of each patient is unknown because no autopsy was performed. In addition, since the research was conducted at a single hospital, the findings may be biased because of differences between medical institutions. Furthermore, because it is difficult to identify problems occurring prior to hospital arrival, errors during pre-hospital treatment or patient transfer may have been underestimated. Further research is needed to address these issues. To identify issues in the management of severe trauma and improve outcomes, each trauma center should evaluate preventable mortality through standardized evaluation indicators and a nationwide study of preventable mortality should be conducted.
CONCLUSION
- The preventable mortality rate of trauma patients who visited Gachon University Gil Hospital regional trauma center was 8%. Multiple organ failure and massive bleeding in the torso accounted for the largest portion of the causes of death in cases of preventable death. Most errors in the treatment of trauma patients occurred in the early stages of the treatment process and in the ICU. Therefore by identifying the main causes of preventable death and errors during the course of treatment, our research will help to reduce the preventable death rate. Finally, appropriate trauma care systems and ongoing education are needed to reduce preventable deaths from trauma.
ARTICLE INFORMATION
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
INFORMED CONSENT
This type of study does not require informed consent.
Fig. 1.Flowchart for establishing the number of preventable deaths from trauma out of all trauma admissions in the period from 2015 to 2017. DOA: death on arrival, CPR: cardiopulmonary resuscitation, NP: non-preventable, DP: definitely preventable, PP: potentially preventable.
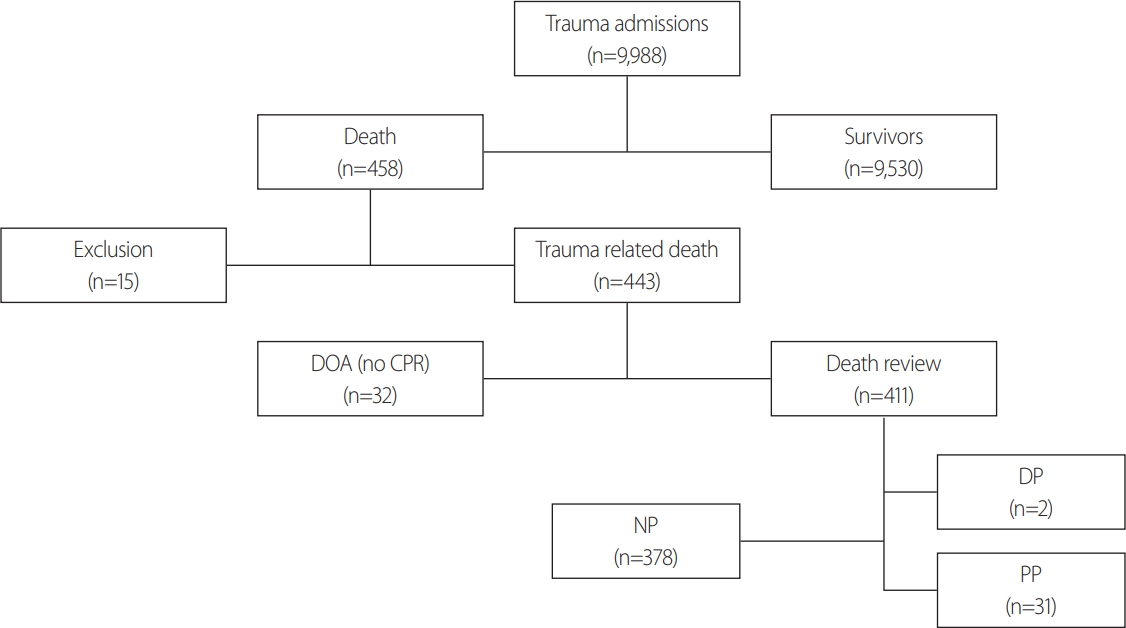
Fig. 2.(A) Breakdown of deaths by trauma according to patient age group. (B) Breakdown of deaths by time to death from hospital admission.

Table 1.Clinical characteristics of trauma patients
|
Values (n=411) |
|
Age (years) (mean±SD) |
56.4±19.5 |
|
Male (n [%]) |
286 (69.6) |
|
Blunt trauma (n [%]) |
397 (96.6) |
|
Interhospital transfer (n [%]) |
110 (26.8) |
|
Initial systolic blood pressure (mmHg) (median [IQR]) |
37 (0.0–124.0) |
|
Initial heart rate (median [IQR]) |
65 (0.0–98.0) |
|
ISS (mean±SD) |
22.0±14.3 |
|
RTS (median [IQR]) |
1.89 (0.0–5.2) |
|
TRISS (Ps %) (median [IQR]) |
16 (3.0–62.0) |
Table 2.Preventable deaths by cause of death and TRISS score
|
Cause of death (n=233) (178 deaths of unknown causes excluded) |
Number |
|
NP |
|
DP+PP |
|
Traumatic brain injury |
127 |
|
121 (95.3) |
|
6 (4.7) |
|
Massive hemorrhage |
45 |
|
38 (84.4) |
|
7 (15.6) |
|
Multiple organ failure |
48 |
|
30 (62.5) |
|
18 (37.5) |
|
Others |
13 |
|
11 (84.6) |
|
2 (15.4) |
|
Ps from TRISS (n=398) (13 missing data)
|
|
Number
|
|
DP+PP
|
|
|
Ps <25% |
|
218 |
|
5 (2.3) |
|
|
Ps 25–50% |
|
55 |
|
3 (5.5) |
|
|
Ps >50% |
|
125 |
|
25 (20.0) |
|
Table 3.Types and locations of errors that occurred during trauma management in cases of preventable death
|
Errors in DP+PP patients |
|
Error type |
|
|
Delayed control of hemorrhage |
13 (30.9) |
|
Abdominal/pelvic hemorrhage |
5 (11.9) |
|
Intra-thoracic hemorrhage |
5 (11.9) |
|
Other source of bleeding |
3 (7.1) |
|
Delayed management of traumatic brain injury |
1 (2.4) |
|
Under-resuscitation |
2 (4.8) |
|
Inadequate prophylaxis |
5 (11.9) |
|
Deep vein thrombosis/pulmonary embolism prophylaxis |
4 (9.5) |
|
Genitourinary prophylaxis |
1 (2.4) |
|
Inappropriate intensive care unit management |
4 (9.5) |
|
Inappropriate inter-hospital transfer |
2 (4.8) |
|
Missed intra-abdominal injury |
4 (9.5) |
|
Other poor management decisions |
9 (21.4) |
|
Unsuccessful intubation and delayed surgical airway |
1 (2.4) |
|
Unstable patient sent to computed tomography scan |
1 (2.4) |
|
Place |
|
|
Intensive care unit |
13 (31.0) |
|
Emergency room |
12 (29.0) |
|
Ward |
10 (24.0) |
|
Pre-hospital |
6 (14.0) |
|
Operating room |
1 (2.0) |
REFERENCES
- 1. Statistics Korea. Causes of death statistics in 2016 [Internet]. Daejeon: Statistics Korea; 2017 [cited 2020 Sep 10]. Available from: http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&bSeq=&aSeq=363695&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=s-rch&sTarget=title&sTxt=death+.
- 2. Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev 2015;21:434–40. ArticlePubMed
- 3. Brenneman FD, Redelmeier DA, Boulanger BR, McLellan BA, Culhane JP. Long-term outcomes in blunt trauma: who goes back to work? J Trauma 1997;42:778–81. PubMed
- 4. Pfeifer R, Lichte P, Zelle BA, Sittaro NA, Zilkens A, Kaneshige JR, et al. Socio-economic outcome after blunt orthopaedic trauma: implications on injury prevention. Patient Saf Surg 2011;5:9. ArticlePubMedPMC
- 5. Chiara O, Cimbanassi S, Pitidis A, Vesconi S. Preventable trauma deaths: from panel review to population based-studies. World J Emerg Surg 2006;1:12. ArticlePubMedPMC
- 6. Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci 2019;34:e65. ArticlePubMedPMC
- 7. Jung KY, Kim SP, Kin SH, Kim H, Noh H, Chang HY, et al. Analysis and development plan of South Korea's trauma medical system [Internet]. Sejong: Ministry of Health and Welfare; 2011 [cited 2020 Sep 10]. Available from: https://webcache.googleusercontent.com/search?q=cache:RTuwoTRf5OEJ:https://media.nemc.or.kr/file/download_file_encrypt.do%3Ffileitemno%3D6c1efcf9f8fb4033b1cb51a8367612b4+&cd=2&hl=ko&ct=-clnk&gl=kr.
- 8. Ghorbani P, Strommer L. Analysis of preventable deaths and errors in trauma care in a Scandinavian trauma level-I centre. Acta Anaesthesiol Scand 2018;62:1146–53. Article
- 9. Esposito TJ, Sanddal TL, Reynolds SA, Sanddal ND. Effect of a voluntary trauma system on preventable death and inappropriate care in a rural state. J Trauma 2003;54:663–70. ArticlePubMed
- 10. Zafarghandi MR, Modaghegh MH, Roudsari BS. Preventable trauma death in Tehran: an estimate of trauma care quality in teaching hospitals. J Trauma 2003;55:459–65. ArticlePubMed
- 11. Teixeira PG, Inaba K, Hadjizacharia P, Brown C, Salim A, Rhee P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma 2007;63:1338–47. ArticlePubMed
- 12. Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma 1987;27:370–8. PubMed
- 13. Baker SP, O'Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187–96. PubMed
- 14. Cayten CG, Stahl WM, Agarwal N, Murphy JG. Analyses of preventable deaths by mechanism of injury among 13,500 trauma admissions. Ann Surg 1991;214:510–21. ArticlePubMedPMC
- 15. Kim Y, Jung KY, Cho KH, Kim H, Ahn HC, Oh SH, et al. Preventable trauma deaths rates and management errors in emergency medical system in Korea. J Korean Med Sci 2006;17:385–94.
- 16. Jung KY, Kim SP, Kin SH, Kim H, Noh H, Chang HY, et al. A study on emergency medical system performance indicators in Korea [Internet]. Sejong: Ministry of Health and Welfare; 2008 [cited 2020 Sep 10]. Available from: https://webcache.googleusercontent.com/search?q=cache:4cqokX7gwdsJ:https://media.nemc.or.kr/file/download_file_encrypt.do%3Ffileitemno%3Dcb7aa0cf2fdcc380dde65cbe65334cab+&cd=1&hl=ko&ct=-clnk&gl=kr.
- 17. MacKenzie EJ. Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma 1999;47(Suppl 3):S34–41. ArticlePubMed
- 18. West JG. Validation of autopsy method for evaluating trauma care. Arch Surg 1982;117:1033–5. ArticlePubMed
- 19. Oyeniyi BT, Fox EE, Scerbo M, Tomasek JS, Wade CE, Holcomb JB. Trends in 1029 trauma deaths at a level 1 trauma center: impact of a bleeding control bundle of care. Injury 2017;48:5–12. ArticlePubMed
- 20. Härtl R, Gerber LM, Iacono L, Ni Q, Lyons K, Ghajar J. Direct transport within an organized state trauma system reduces mortality in patients with severe traumatic brain injury. J Trauma 2006;60:1250–6. ArticlePubMed
Citations
Citations to this article as recorded by

- Effects of Transport to Trauma Centers on Survival Outcomes Among Severe Trauma Patients in Korea: Nationwide Age-Stratified Analysis
Hakrim Kim, Kyoung Jun Song, Ki Jeong Hong, Jeong Ho Park, Tae Han Kim, Stephen Gyung Won Lee
Journal of Korean Medical Science.2024;[Epub] CrossRef - TiME OUT: Time-specific machine-learning evaluation to optimize ultramassive transfusion
Courtney H. Meyer, Jonathan Nguyen, Andrew ElHabr, Nethra Venkatayogi, Tyler Steed, Judy Gichoya, Jason D. Sciarretta, James Sikora, Christopher Dente, John Lyons, Craig M. Coopersmith, Crystal Nguyen, Randi N. Smith
Journal of Trauma and Acute Care Surgery.2024; 96(3): 443. CrossRef - Progressive Reduction in Preventable Mortality in a State Trauma System Using Continuous Preventable Mortality Review to Drive Provider Education: Results of Analyzing 1,979 Trauma Deaths from 2015 to 2022
Charles D Mabry, Benjamin Davis, Michael Sutherland, Ronald Robertson, Jennifer Carger, Deidre Wyrick, Terry Collins, Austin Porter, Kyle Kalkwarf
Journal of the American College of Surgeons.2024; 238(4): 426. CrossRef - Emergency department laparotomy for patients with severe abdominal trauma: a retrospective study at a single regional trauma center in Korea
Yu Jin Lee, Soon Tak Jeong, Joongsuck Kim, Kwanghee Yeo, Ohsang Kwon, Kyounghwan Kim, Sung Jin Park, Jihun Gwak, Wu Seong Kang
Journal of Trauma and Injury.2024; 37(1): 20. CrossRef - Angioembolization performed by trauma surgeons for trauma patients: is it feasible in Korea? A retrospective study
Soonseong Kwon, Kyounghwan Kim, Soon Tak Jeong, Joongsuck Kim, Kwanghee Yeo, Ohsang Kwon, Sung Jin Park, Jihun Gwak, Wu Seong Kang
Journal of Trauma and Injury.2024; 37(1): 28. CrossRef - Nomogram for predicting in-hospital mortality in trauma patients undergoing resuscitative endovascular balloon occlusion of the aorta: a retrospective multicenter study
Byungchul Yu, Jayun Cho, Byung Hee Kang, Kyounghwan Kim, Dong Hun Kim, Sung Wook Chang, Pil Young Jung, Yoonjung Heo, Wu Seong Kang
Scientific Reports.2024;[Epub] CrossRef - Analysis of mortality over 7 years in a mature trauma center: evolution of preventable mortality in severe trauma patients
Sarah Guigues, Jean Cotte, Jean-Baptiste Morvan, Henry de Lesquen, Bertrand Prunet, Mathieu Boutonnet, Nicolas Libert, Pierre Pasquier, Eric Meaudre, Julien Bordes, Michael Cardinale
European Journal of Trauma and Emergency Surgery.2023; 49(3): 1425. CrossRef - Incidence and predictors of mortality among adult trauma patients admitted to the intensive care units of comprehensive specialized hospitals in Northwest Ethiopia
Mengistu Abebe Messelu, Ambaye Dejen Tilahun, Zerko Wako Beko, Hussien Endris, Asnake Gashaw Belayneh, Getayeneh Antehunegn Tesema
European Journal of Medical Research.2023;[Epub] CrossRef - Characteristics and Clinical Outcomes of Elderly Patients with Trauma Treated in a Local Trauma Center
Kwanhoon Park, Geonjae Cho, Sungho Lee, Kang Yoon Lee, Ji Young Jang
Journal of Acute Care Surgery.2023; 13(1): 13. CrossRef - An Artificial Intelligence Model for Predicting Trauma Mortality Among Emergency Department Patients in South Korea: Retrospective Cohort Study
Seungseok Lee, Wu Seong Kang, Do Wan Kim, Sang Hyun Seo, Joongsuck Kim, Soon Tak Jeong, Dong Keon Yon, Jinseok Lee
Journal of Medical Internet Research.2023; 25: e49283. CrossRef - Preventable Death Rate of Trauma Patients in a Non-Regional Trauma Center
Kwanhoon Park, Wooram Choi, Sungho Lee, Kang Yoon Lee, Dongbeen Choi, Han-Gil Yoon, Ji Young Jang
Journal of Acute Care Surgery.2023; 13(3): 118. CrossRef - Nine year in-hospital mortality trends in a high-flow level one trauma center in Italy
Elisa Reitano, Roberto Bini, Margherita Difino, Osvaldo Chiara, Stefania Cimbanassi
Updates in Surgery.2022; 74(4): 1445. CrossRef - Decision support by machine learning systems for acute management of severely injured patients: A systematic review
David Baur, Tobias Gehlen, Julian Scherer, David Alexander Back, Serafeim Tsitsilonis, Koroush Kabir, Georg Osterhoff
Frontiers in Surgery.2022;[Epub] CrossRef - Flat Inferior Vena Cava on Computed Tomography for Predicting Shock and Mortality in Trauma: A Meta-Analysis
Do Wan Kim, Hee Seon Yoo, Wu Seong Kang
Diagnostics.2022; 12(12): 2972. CrossRef - Model for Predicting In-Hospital Mortality of Physical Trauma Patients Using Artificial Intelligence Techniques: Nationwide Population-Based Study in Korea
Seungseok Lee, Wu Seong Kang, Sanghyun Seo, Do Wan Kim, Hoon Ko, Joongsuck Kim, Seonghwa Lee, Jinseok Lee
Journal of Medical Internet Research.2022; 24(12): e43757. CrossRef - Thoracic injuries in trauma patients: epidemiology and its influence on mortality
Andrea Lundin, Shahzad K. Akram, Lena Berg, Katarina E. Göransson, Anders Enocson
Scandinavian Journal of Trauma, Resuscitation and .2022;[Epub] CrossRef



 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite