Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Case Report
Successful nonoperative management of a simultaneous high-grade splenic injury and devascularized kidney in Australia: a case report -
Peter Thanh Tam Nguyen, MD1
 , Jeremy M. Hsu, MBBS1,2
, Jeremy M. Hsu, MBBS1,2
-
Journal of Trauma and Injury 2023;36(4):431-434.
DOI: https://doi.org/10.20408/jti.2023.0017
Published online: September 7, 2023
- 541 Views
- 11 Download
1Trauma Service, Westmead Hospital, Sydney, Australia
2Westmead Clinical School, University of Sydney, Sydney, Australia
- Correspondence to Peter Thanh Tam Nguyen, MD Trauma Service, Westmead Hospital, Cnr Hawkesbury Road and Darcy Rd Westmead, Sydney 2145, Australia Tel: +61-2-8890-5555 Email: Peter.Nguyen2@health.nsw.gov.au
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Severe blunt injuries to isolated solid abdominal viscera have been previously managed nonoperatively; however, management algorithms for simultaneous visceral injuries are less well defined. We report a polytrauma case of a 33-year-old man involved in a motorbike collision who presented with left-sided chest and abdominal pain. Initial imaging demonstrated multiple solid organ injuries with American Association for the Surgery of Trauma (AAST) grade V splenic injury and complete devascularization of the left kidney. The patient underwent urgent angioembolic coiling of the distal splenic artery with successful nonoperative management of simultaneous grade V solid organ injuries.
- In hospitalized patients, abdominal solid organ injuries are associated with a mortality rate of approximately 5% [1]. Nonoperative management is the preferred approach for stable patients with isolated splenic injuries resulting from blunt trauma [2]. However, simultaneous multiple solid organ injuries are associated with the failure of nonoperative therapy and an increased risk of complications, including pneumonia, sepsis, and prolonged hospitalization [3,4]. Risk factors associated with the failure of nonoperative management include older age, the presence of vascular blush on computed tomography, and a large volume of hemoperitoneum [4]. Additionally, signs of hemodynamic instability including hypotension on presentation, higher Injury Severity Scores (ISSs), and high transfusion requirements are factors associated with a higher mortality rate [3]. We describe below the successful nonoperative management of simultaneous high-grade splenic and kidney injuries following blunt trauma.
INTRODUCTION
- A man in his 30s presented to our level I trauma center (Westmead Hospital, Sydney, Australia) after being ejected from a motorbike at high speed whilst under the influence of methamphetamines. He was hemodynamically stable, but exhibited confusion and agitation, with a Glasgow Coma Scale of 14. The patient had no relevant past medical history.
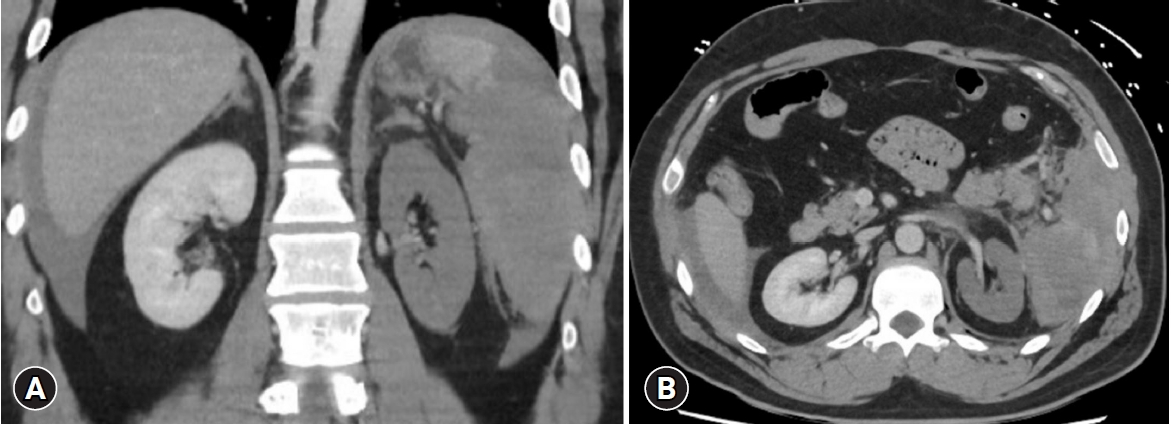
- An extended focused assessment with sonography for trauma examination was positive for free fluid in the left subphrenic, hepatorenal, and pelvic spaces. Trauma pan computed tomography (CT) demonstrated a large volume of hemoperitoneum, grade V splenic injury, left adrenal hematoma, and a grade V left renal vascular pedicle injury with devascularized left kidney, but no perirenal hematoma (Fig. 1). Other injuries included anterior mediastinal hematoma, bony injuries including right scaphoid and lunate fractures, a left scapula supraclavicular fossa fracture, and an isolated posterior 11th rib fracture. The biochemical markers on presentation were notable for marked acidosis with a venous pH of 7.26 and lactate level of 3.7 mmol/L but a base excess of –1.6 mmol/L. Hemoglobin on presentation was normal (134 g/L), and the patient was identified to be heterozygous for factor V Leiden mutation Arg506Gln (associated with an increased risk of venous thromboembolism [5]).
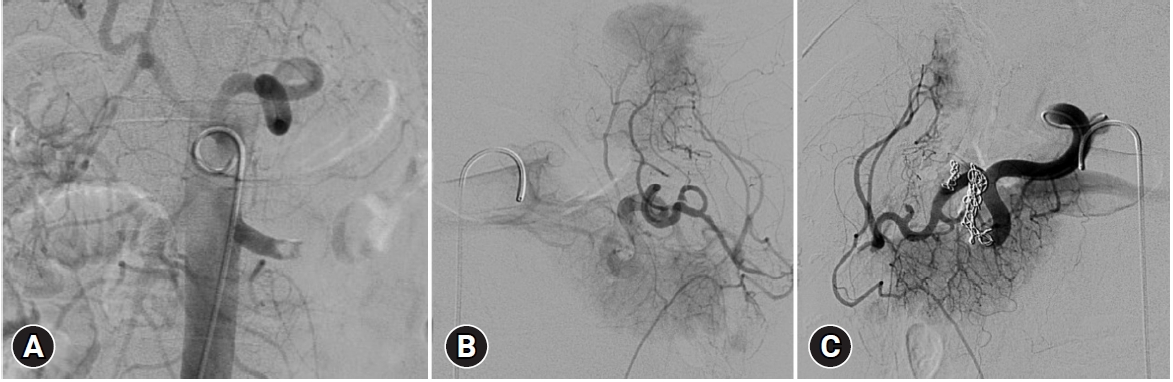
- The patient was managed with urgent interventional radiology 6 hours after presentation, with a diagnostic aortogram and splenic angiogram demonstrating traumatic dissection and abrupt occlusion of the left main renal artery approximately 2 cm from the renal ostium. No evidence of arteriovenous fistulae or active bleeding was noted. Despite the high-grade renal injury, the renal parenchyma remained intact, and percutaneous stenting was considered as a feasible management strategy. The interventional radiologist was unable to traverse the injury with a wire, and therefore the plan for stenting was abandoned. Significant fragmentation and devascularization of the spleen were identified. Thirteen coils were deployed with additional gelfoam embolization to distal splenic and associated branches beyond the pancreatica magna artery, as shown in Fig. 2. The patient’s scaphoid and lunate fractures were managed with open reduction and internal fixation, while the other bony injuries were nonoperatively managed. The patient was monitored with 6-hourly hemoglobin levels with a trough hemoglobin level of 83 g/L and serial examinations. Chemical venous thromboembolism prophylaxis was commenced 24 hours following angioembolization.
- The patient remained hemodynamically stable throughout his admission; however, cyclical high fevers up to 39°C were observed with unremarkable septic screens. Intravenous empirical antibiotics were administered for 7 days after fever commencement. Interval abdominopelvic CT performed 4 and 8 days after presentation demonstrated splenic and left renal infarcts consistent with prior imaging, with no new hematoma formation, pseudoaneurysm, or associated intraabdominal abscesses. Atelectasis was identified on chest imaging. The patient was commenced on patient-controlled analgesia (PCA) and ketamine infusion initially. PCA was discontinued on day 6 posttrauma and de-escalated to only oral analgesia on day 7. He was discharged on day 13, with outpatient follow-up.
- Ethics statement
- Consent for publication of the research details and clinical images was obtained from the patient.
CASE REPORT
- The management of solid injuries is predominantly nonoperative in hemodynamically stable patients, and angioembolization is a useful adjunct to solid organ preservation [6]. The success rates of nonoperative management have been reported to be approximately 86% in splenic trauma [4], 97% in hepatic trauma [7], and 92% in renal trauma [8]. The grading of splenic injuries according to the American Association for the Surgery of Trauma (AAST) Injury Scoring Scale ranges from grade I to V, with grade V referring to splenic and kidney injuries with vascular involvement and bleeding extension into the peritoneum or shattered or devitalized parenchyma. Although some evidence demonstrating a correlation between the failure of nonoperative management and the grade of injury [9], multiple other studies have indicated that nonoperative management is ideal independent of the lesion grade, more strongly for splenic injuries [10] than for renal injuries [9]. Some contemporary recommendations suggest operative management of grade V kidney injuries [6,11,12] depending on hemodynamic stability. In broad terms, however, the risk factors for failure of nonoperative management of solid viscus injuries, including refractory haemodynamic instability and worsening biochemical markers of perfusion (for example, lactate and base excess), reflect the physiologic status of the patient. In this case of a hemodynamically stable patient with no comorbidities, further attempts at renal revascularisation were not pursued. Prolonged ischaemic time is associated with exponential losses in kidney function [11]. An operative intervention was not pursued, as expectant management of sequelae (such as progression to chronic kidney disease or hypertension) during follow-up was considered to have a more favorable risk profile.
- Patterns of concomitant solid organ injuries are less well studied and have fewer recommendations for nonoperative management. Important concepts include early recognition with CT imaging [2,13] and serial clinical examinations, with diffuse peritonitis, hemodynamic instability, or persistent biochemical signs of shock despite resuscitation being the only reliable markers of the failure of operative management. Older age, higher ISSs, head injury, the presence of femur fractures, and ongoing blood transfusion requirements are similarly factors that favor operative management and are predictors of failure of nonoperative management [3,4].
- This case highlights the successful nonoperative management of concomitant splenic and renal injuries. Solid organ injury management should be dependent on clinical status, with radiology findings determining the role of angioembolization, even in the setting of multiple solid organ injuries.
DISCUSSION
-
Author contributions
Conceptualization: PTTN; Data curation: PTTN; Investigation: PTNN; Methodology: PTTN; Project administration: PTTN; Supervision: HJ; Visualization: PTNN; Writing–original draft: PTTN; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
Jeremy M. Hsu is an Editorial Board member of the Journal of Trauma and Injury, but was not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Data availability
Data sharing is not applicable as no new data were created or analyzed in this study.
ARTICLE INFORMATION
- 1. Abo-Elhoda MF, Attia SM, Ahmed ME, Abdeldaiem KA. Solid organs injuries in blunt abdominal trauma patients. Egypt J Hosp Med 2021;83:1477–83. Article
- 2. Stassen NA, Bhullar I, Cheng JD, et al. Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012;73(5 Suppl 4):S294–300. PubMed
- 3. El-Menyar A, Abdelrahman H, Al-Hassani A, et al. Single versus multiple solid organ injuries following blunt abdominal trauma. World J Surg 2017;41:2689–96. ArticlePubMedPDF
- 4. Teuben MP, Spijkerman R, Blokhuis TJ, et al. Safety of selective nonoperative management for blunt splenic trauma: the impact of concomitant injuries. Patient Saf Surg 2018;12:32. ArticlePubMedPMCPDF
- 5. Simioni P, Prandoni P, Lensing AW, et al. The risk of recurrent venous thromboembolism in patients with an Arg506->Gln mutation in the gene for factor V (factor V Leiden). N Engl J Med 1997;336:399–403. ArticlePubMed
- 6. Kanlerd A, Auksornchart K, Boonyasatid P. Non-operative management for abdominal solidorgan injuries: a literature review. Chin J Traumatol 2022;25:249–56. ArticlePubMedPMC
- 7. Brillantino A, Iacobellis F, Festa P, et al. Non-operative management of blunt liver trauma: safety, efficacy and complications of a standardized treatment protocol. Bull Emerg Trauma 2019;7:49–54. ArticlePubMedPMCPDF
- 8. van der Wilden GM, Velmahos GC, Joseph DK, et al. Successful nonoperative management of the most severe blunt renal injuries: a multicenter study of the research consortium of New England Centers for Trauma. JAMA Surg 2013;148:924–31. ArticlePubMed
- 9. Keihani S, Xu Y, Presson AP, et al. Contemporary management of high-grade renal trauma: results from the American Association for the Surgery of Trauma Genitourinary Trauma study. J Trauma Acute Care Surg 2018;84:418–25. ArticlePubMed
- 10. Ruscelli P, Gemini A, Rimini M, et al. The role of grade of injury in non-operative management of blunt hepatic and splenic trauma: case series from a multicenter experience. Medicine (Baltimore) 2019;98:e16746. PubMedPMC
- 11. Coccolini F, Moore EE, Kluger Y, et al. Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg 2019;14:54. ArticlePubMedPMCPDF
- 12. Brown CV, Alam HB, Brasel K, et al. Western trauma association critical decisions in trauma: management of renal trauma. J Trauma Acute Care Surg 2018;85:1021–5. ArticlePubMed
- 13. The EAST Practice Management Guidelines Work Group; Holevar M, DiGiacomo JC, et al. Practice management guidelines for the evaluation of genitourinary trauma. Eastern Association for the Surgery of Trauma (EAST); 2003.
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Blunt abdominal trauma resulting in pancreatic injury in a pediatric patient in Australia: a case report
- Nonoperative management of colon and mesocolon injuries caused by blunt trauma: three case reports
- Successful management of a common carotid artery injury using a Pruitt-F3 Carotid Shunt: a case report
- Very large haematoma following the nonoperative management of a blunt splenic injury in a patient with preexisting liver cirrhosis: a case report
 KST
KST

 PubReader
PubReader ePub Link
ePub Link Cite
Cite



