Articles
- Page Path
- HOME > J Trauma Inj > Volume 36(4); 2023 > Article
-
Original Article
Clinical characteristics and mortality risk factors among trauma patients by age groups at a single center in Korea over 7 years: a retrospective study -
Jonghee Han, MD1
 , Su Young Yoon, MD1
, Su Young Yoon, MD1 , Junepill Seok, MD1
, Junepill Seok, MD1 , Jin Young Lee, MD2
, Jin Young Lee, MD2 , Jin Suk Lee, MD2
, Jin Suk Lee, MD2 , Jin Bong Ye, MD2
, Jin Bong Ye, MD2 , Younghoon Sul, MD2,3
, Younghoon Sul, MD2,3 , Seheon Kim, MD2
, Seheon Kim, MD2 , Hong Rye Kim, MD4
, Hong Rye Kim, MD4
-
Journal of Trauma and Injury 2023;36(4):329-336.
DOI: https://doi.org/10.20408/jti.2023.0035
Published online: November 7, 2023
- 736 Views
- 35 Download
1Department of Cardiovascular and Thoracic Surgery, Trauma Center, Chungbuk National University Hospital, Cheongju, Korea
2Deparment of Trauma Surgery, Trauma Center, Chungbuk National University Hospital, Cheongju, Korea
3Department of Trauma Surgery, Chungbuk National University College of Medicine, Cheongju, Korea
4Department of Neurosurgery, Chungbuk National University Hospital, Cheongju, Korea
- Correspondence to Su Young Yoon, MD Department of Cardiovascular and Thoracic Surgery, Trauma Center, Chungbuk National University Hospital, Cheongju, 776 1sunhwan-ro, Seowon-gu, Cheongju 28644, Korea Tel: +82-43-269-7849 Email: cbnuhtraumacs@gmail.com
Copyright © 2023 The Korean Society of Traumatology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Purpose
- In this study, we aimed to compare the characteristics of patients with trauma by age group in a single center in Korea to identify the clinical characteristics and analyze the risk factors affecting mortality.
-
Methods
- Patients aged ≥18 years who visited the Chungbuk National University Hospital Regional Trauma Center between January 2016 and December 2022 were included. The accident mechanism, severity of the injury, and outcomes were compared by classifying the patients into group A (18–64 years), group B (65–79 years), and group C (≥80 years). In addition, logistic regression analysis was performed to identify factors affecting death.
-
Results
- The most common injury mechanism was traffic accidents in group A (40.9%) and slipping in group B (37.0%) and group C (56.2%). Although group A had the highest intensive care unit admission rate (38.0%), group C had the highest mortality rate (9.5%). In the regression analysis, 3 to 8 points on the Glasgow Coma Scale had the highest odds ratio for mortality, and red blood cell transfusion within 24 hours, intensive care unit admission, age, and Injury Severity Score were the predictors of death.
-
Conclusions
- For patients with trauma, the mechanism, injured body region, and severity of injury differed among the age groups. The high mortality rate of elderly patients suggests the need for different treatment approaches for trauma patients according to age. Identifying factors affecting clinical patterns and mortality according to age groups can help improve the prognosis of trauma patients in the future.
- Background
- Trauma is the leading cause of death for people of different age groups in Korea. According to the 2021 statistics, traffic accidents are the ninth most common cause of death for men, especially for young people under the age of 40 years. In contrast, the rate of the causes of death by trauma in the elderly is low, but it is steadily increasing as the elderly population increases [1].
- The variations in the type of trauma or mechanism of injury can be attributed to the differences in the areas of activity or occupation according to age. Therefore, various clinical characteristics can be observed according to patient age. In particular, in the elderly patient group, physiological changes occur in and affect various body systems [2]. Age is a predictor of poor prognosis in patients [3–5] and increases mortality, especially among those over 65 years of age [6]. However, the prognosis of elderly patients who experience trauma is still controversial [7,8]. It is necessary to identify the characteristics of trauma patients according to age in order to provide appropriate treatment. In addition, the prognosis can be improved, and the mortality rate can be lowered through aggressive initial treatment.
- Objectives
- This study aimed to analyze the mortality rates of trauma patients who visited a single regional trauma center for 7 years. The patients were stratified by age group to identify the clinical characteristics and factors related to mortality.
INTRODUCTION
- Ethics statement
- This study was approved by the Institutional Review Board of Chungbuk National University Hospital (No. 2023-03-011-001). The requirement for informed consent was waived due to the retrospective nature of the study.
- Patients and data collection
- This retrospective study included trauma patients who visited the Chungbuk National University Hospital Regional Trauma Center and Regional Emergency Medical Center (Cheongju, Korea) from January 2016 to December 2022. Data from the medical records of the patients admitted to this hospital and registered in the Korean Trauma Database (KTDB) were collected and analyzed.
- Those who were aged below 17 years at the time of hospital visit, had already died at the time of arrival in the emergency room, or did not survive after CPR were excluded. The patients were classified into the following groups: group A (18–64 years), group B (65–79 years), and group C (≥80 years). The clinical characteristics were compared among the groups. Patients whose systolic blood pressure at the time of visiting the emergency room was <90 mmHg were considered hypotensive.
- The distribution of patients according to the Abbreviated Injury Scale (AIS) score were comparatively analyzed; areas with an AIS of 3 or more were classified as having undergone severe damage. Based on the Injury Severity Score (ISS), an indicator of the severity of damage, the patients were classified into mild and severe groups using a cutoff score of 15. Based on the Glasgow Coma Scale (GCS) score, the patients were classified into severe (3–8 points), moderate (9–12 points), and mild (13–15 points) groups. The Trauma and Injury Severity Score (TRISS), and Geriatric Trauma Outcome Score (GTOS) [9–11] were used to determine the patient's prognosis, and the GTOS was calculated using the following formula:
- GTOS = age + (2.5 × ISS) + 22 (if given packed red blood cell)
- Statistical analysis
- Statistical analyses were performed using R ver. 4.2.2 (R Foundation for Statistical Computing). Continuous variables that did not satisfy normality were expressed as median with an interquartile range (IQR). Categorical variables were expressed as percentage. Chi-square test or Fisher exact test was used for nominal variables, and one-way analysis of variance or the Kruskal-Wallis test was used for continuous variables depending on their normality. Logistic regression analysis was performed to analyze risk factors for death, and the Hosmer-Lemeshow goodness-of-fit test was performed to confirm the suitability of the test. A P-value of <0.05 was considered statistically significant.
METHODS
- Demographics
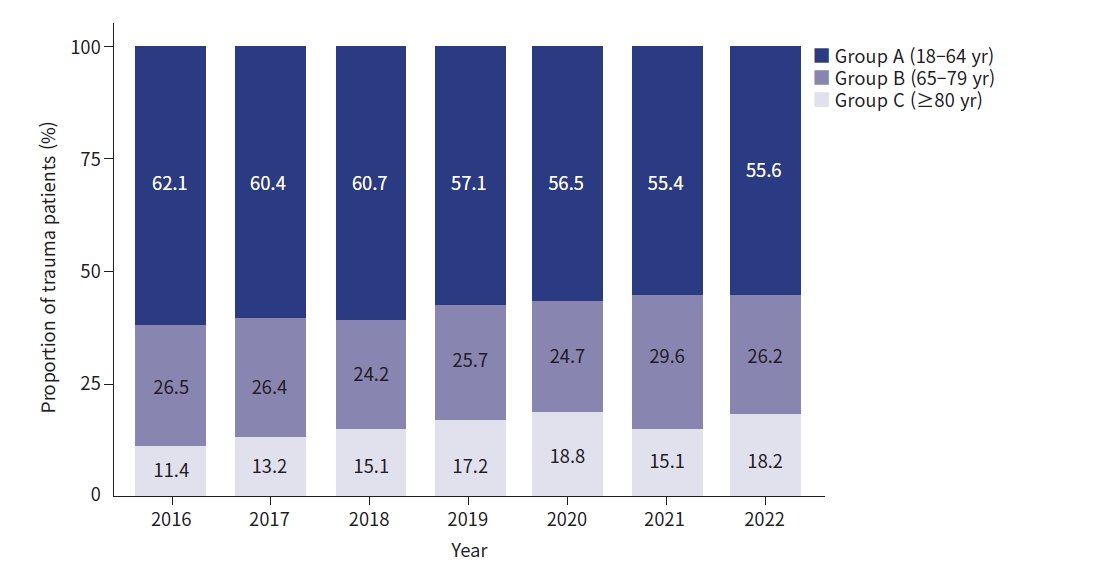
- Among the trauma patients who visited the hospital during the study period, 7,843 were analyzed. There were 4,573 patients in group A, 2,041 in group B, and 1,229 in group C. Since 2020, there has been an overall decrease in the numbers of patients with COVID-19 pandemic; however, the proportion of elderly patients has been steadily increasing (Fig. 1). Men accounted for 62.9% of the total sample, but as the age increased, the proportion of women increased. In group C, the proportion of men accounted for 37.7%. Most of the injury was blunt trauma and increased with age. Most injuries were the result of traffic accidents (36.2%), including pedestrian injuries,, falls (18.2%), and slips (27.3%), and the proportion of falls and slips tended to increase steeply with age. The lowest incidence of trauma was observed in winter in all age groups (Table 1).
- Injured body region and injury severity
- Except for the facial and external areas, pelvis and extremities (55.1%) were the most frequently injured areas in all age groups, followed by the head and neck (31.1%), chest (29.1%), and abdomen (20.4%). As age increased, injuries to the head, neck, thorax, and abdomen decreased frequently, and only injuries to the pelvic and limb areas tended to increase with age. In particular, the incidence of severe injury (AIS score, >3) in the pelvis and extremities was the highest in group C (49.1%). Multiple injuries were observed in 3,420 patients (43.6%), and the frequency decreased with age (Table 2).
- The median ISS was 9 (IQR, 4–16), and the difference in the scores among the groups was not significant. The ISS was the highest in group A (30.4%) and decreased significantly with age (group B, 26.5%; group C, 20.1%). The GCS score severity showed no significant difference among the groups; however, TRISS and GTOS showed significant differences among the groups (Table 3).
- Clinical parameters and outcomes
- At the time of visiting the emergency room, the incidence rate of low blood pressure and red blood cell transfusion within 4 hours of visiting the hospital were the highest in group A. However, the proportion of patients requiring red blood cell transfusions within 24 hours after visiting the hospital, group C was 19.6%, higher than the rates in both group A (17.8%) and group B (18.4%). The proportion of patients requiring surgery or interventions was the highest in group A (25.7%) compared to that in group B (18.2%) and group C (12.8%) (Table 4).
- The rate of intensive care unit (ICU) hospitalization was the highest in group A; the length of ICU stay was the longest in group C. The in-hospital mortality rate was 5.4% for the entire study group; group C had the highest in-hospital mortality rate of 9.5%. When calculated only for patients admitted to the ICU, the mortality rates were 9.4%, 16.7%, and 26.6% for groups A, B, and C, respectively (Table 4).
- Predictors of mortality
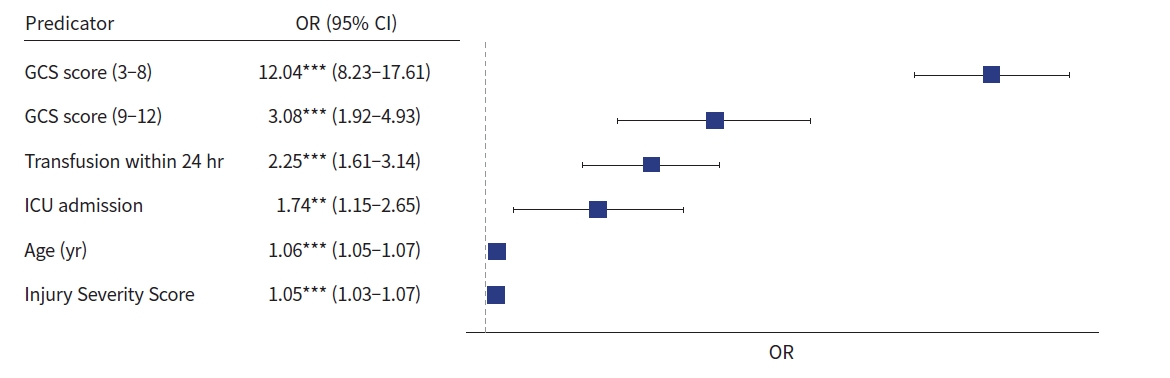
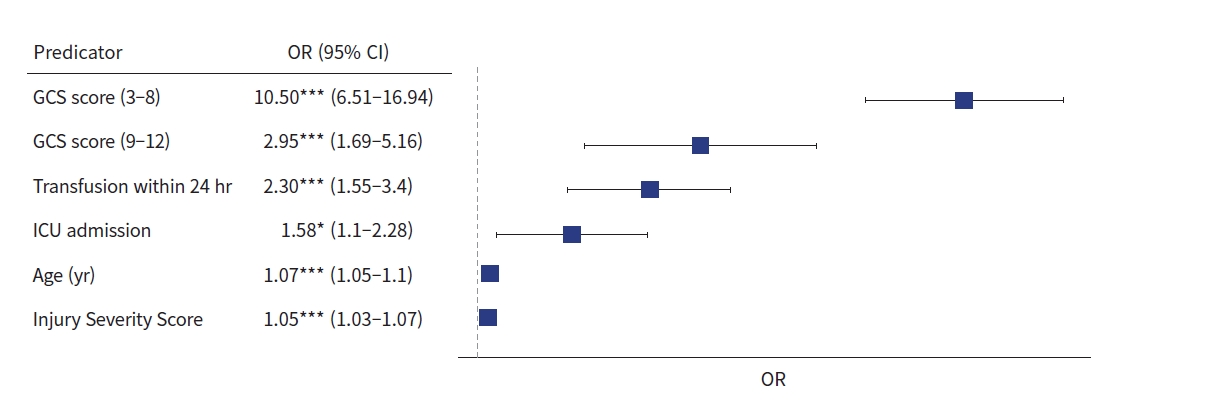
- Logistic regression analysis was performed using sex, age, ISS, red blood cell transfusion, hypotension, ICU admission, GCS score, surgery, and intervention as independent variables (Table 5). The GCS score had the highest odds ratio (12.04; 95% confidence interval, 8.23–17.61; P<0.001). Transfusion within 24 hours, admission to the ICU, age, and ISS were the other predictors (Fig. 2). When logistic regression analysis was conducted on age ≥65 years, the GCS score was the strongest predictor, and sex was a predictor compared with the entire age group. Male sex was a predictor of high mortality rates in the elderly population (odds ratio, 1.58; 95% confidence interval, 1.10–2.28; P<0.05) (Fig. 3).
RESULTS
- This study is meaningful in that the results can improve the treatment of trauma patients by identifying the characteristics, severity of injury of trauma patients by age group. It can also contribute to the appropriate distribution of equipment, manpower, and costs at regional trauma centers by identifying the causes of accidents according to age. In particular, it can be helpful in the treatment of super-aged trauma patients by separately presenting the characteristics of super-aged trauma patients.
- In this study, injuries caused by traffic accidents (36.2%) were the most common among all age groups. In groups A and B, which were socially active, the rate of accidents caused by falls and impaled objects, in addition to traffic accidents, was higher than that in group C. This is thought to be due to the high rate of movement or occupational activity in groups A and B, and the difference in the mechanism of injury appears to be due to a difference in the area or degree of injury. In contrast, in group C, which was a super-aged group, the damage caused by falls was 56.2%, significantly higher than that in the other groups. Owing to the difference in the mechanism of injury, the rate of injury to the head and neck, pelvis, and extremities was high in group C. In addition, osteoporosis is often present in the elderly, so the frequency or severity of fractures in the pelvis or extremities is higher than that in the young, even with low-energy trauma [12,13]. In this study, 73.6% of pelvic fractures in patients aged 80 years or older showed severe damage of 3 AIS. Older patients with pelvic fractures show a fourfold increase in mortality and a higher rate of prolonged hospitalization or other complications than their younger counterparts. In addition, patients aged 60 years or older are reported to have a high risk of intrapelvic bleeding; therefore, interventional procedures, such as angiography or embolization, are often needed early [14]. For elderly patients, even if the frequency of multiple injuries from low-energy trauma is low, active treatment and attention are needed in cases of pelvic injury.
- ISS is useful for predicting the morbidity and mortality of patients with trauma, estimating the length of recovery after trauma, and predicting resource demands in regional trauma centers. ISS was higher in the younger age group, probably due to differences in the mechanism of injury. Several indicators can determine the severity of trauma and predict mortality or survival rates. In this study, GCS scores showed no significant differences among the three age groups. However, TRISS and GTOS showed significant differences. GTOS is a scoring system [9] that can easily predict the possibility of death in elderly patients, and its effectiveness has been verified in several studies [15–17].
- The frequency of low blood pressure, requirement for red blood cell transfusion, and requirement for ICU admission were higher in the younger age group; however, the duration of hospitalization and mortality rate in the ICU were higher in the elderly. In addition, the number of patients who needed red blood cell transfusion within 24 hours was higher in the elderly group than in the younger age group, possibly because of the presence of underlying diseases and systemic conditions that are not explained by injury scores or hypotension immediately after injury and because the elderly have different degrees of physiological responses to acute injuries. Perdue et al. [16] reported that the mortality rate was twice as high in elderly patients, despite having the same injury mechanism and similar damage scores as the younger patients, because they more often have comorbid diseases and complications. Therefore, in the case of elderly patients who visit the hospital for trauma, a detailed treatment approach involving a detailed medical history taking and evaluation of the overall condition is needed.
- Recently, the increase in traffic accidents has led to an increase in the incidence of multiple traumas. A study by van Breugel et al. [17] reported that the overall mortality rate of trauma patients has decreased over the past decade and that the main cause of death has shifted from multiple organ failure to brain damage. In the study by Chang et al. [18], the cause of accidents in patients in severe specialized trauma centers in Korea was traffic accidents, and the main cause of death was brain damage. In this study, similar to previous studies, severe brain injury was the major cause of death. Mock et al. [19] reported that the mortality rate of patients aged 80 years and above admitted to the ICU was 22%, similar to the 26.6% reported in this study. In this study, the mortality rate increased with age and the mortality rate was higher among patients requiring ICU admission.
- Factors affecting posttraumatic mortality vary depending on the study design, but older age, high ISS, and low GCS score have been reported to be some common predictors [20,21]. In this study, low GCS score was also the strongest predictor, followed by blood transfusion, ICU admission, age, and ISS. The odds ratios of low GCS score tended to be lower in the elderly patient group than in the entire age group. Considering that there is no difference in the distribution of GCS score according to the age group, it can be estimated that underlying diseases or frailty affect death in the elderly group. In particular, in the group of elderly patients aged 65 years or older, women had a lower mortality rate than men, probably due to the mechanism of injury in elderly women, mainly slipping.
- Limitations
- This study has several limitations. First, this was a retrospective study and may have been affected by selection bias and unreliable data. Second, this study was based on data from a single center, and the results may not be generalizable to all trauma patients. Third, by excluding patients who died during transport or in the emergency room, the data may not have reflected the mechanism of a severe injury that could cause death at the time of injury.
- Conclusions
- Trauma patients experience different mechanisms, injured body regions, and severities of injury, and the prognosis differs according to age group. Despite the low ICU admission rate among older patients, the high mortality rate suggests that different strategies are required for older trauma patients. For most patients, low GCS score and transfusion within 24 hours were predictors of death. The survival rate of trauma patients can be improved by providing appropriate and aggressive treatment according to the age and characteristics of the patients visiting the emergency department for trauma.
DISCUSSION
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Author contributions
Conceptualization: JHH, SYY; Data curation: JHH, JS, JYL, JSL, JBY, YS, SK, HRK; Formal analysis: JHH; Methodology: JHH; Project administration: YS; Supervision: SYY; Writing–original draft: JHH; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Data availability
Data analyzed in this study are available from the corresponding author upon reasonable request.
ARTICLE INFORMATION

| Variable | Total (n=7,843) | Group A (n=4,573) | Group B (n=2,041) | Group C (n=1,229) | P-value |
|---|---|---|---|---|---|
| Injured body regiona) | |||||
| Head and neck | 2,443 (31.1) | 1,426 (31.2) | 680 (33.3) | 337 (27.4) | <0.001 |
| Face | 999 (12.7) | 713 (15.7) | 219 (10.7) | 67 (5.5) | <0.001 |
| Chest | 2,282 (29.1) | 1,455 (31.8) | c588 (28.8) | 239 (19.4) | <0.001 |
| Abdomen | 1,601 (20.4) | 1,168 (25.5) | 334 (16.4) | 99 (8.1) | <0.001 |
| Pelvis and extremities | 4,318 (55.1) | 2,360 (51.6) | 1,139 (55.8) | 819 (66.6) | <0.001 |
| External | 2,401 (30.6) | 1,615 (35.3) | 561 (27.5) | 225 (18.3) | <0.001 |
| Severely injured regiona),b) | |||||
| Head and neck | 1,789 (22.8) | 993 (21.7) | 524 (25.7) | 272 (22.1) | 0.002 |
| Face | 54 (0.7) | 41 (0.9) | 12 (0.6) | 1 (0.1) | <0.001 |
| Chest | 1,639 (20.9) | 990 (21.6) | 472 (23.1) | 177 (14.4) | <0.001 |
| Abdomen | 781 (10.0) | 584 (12.8) | 156 (7.6) | 41 (3.3) | <0.001 |
| Pelvis and extremities | 2,062 (26.3) | 821 (18.0) | 638 (31.3) | 603 (49.1) | <0.001 |
| External | 7 (0.1) | 7 (0.2) | 0 | 0 | - |
| No. of injured region | <0.001 | ||||
| 2 | 1,635 (20.8) | 1,054 (23.0) | 412 (20.2) | 169 (13.8) | |
| ≥3 | 1,785 (22.8) | 1,218 (26.6) | 419 (20.5) | 148 (12.0) |
Values are presented as median (interquartile range) or number (%). Patients were classified based on age: group A (18–64 years), group B (65–79 years), and group C (≥80 years).
ISS, Injury Severity Score; GCS, Glasgow Coma Scale; TRISS, Trauma and Injury Severity Score; GTOS, Geriatric Trauma Outcome Score.
- 1. Statistics Korea. Causes of death statistics in 2021. Statistics Korea; 2022.
- 2. Gillies D. Elderly trauma: they are different. Aust Crit Care 1999;12:24–30. ArticlePubMed
- 3. Grossman MD, Miller D, Scaff DW, Arcona S. When is an elder old? Effect of preexisting conditions on mortality in geriatric trauma. J Trauma 2002;52:242–6. ArticlePubMed
- 4. Gubler KD, Davis R, Koepsell T, Soderberg R, Maier RV, Rivara FP. Long-term survival of elderly trauma patients. Arch Surg 1997;132:1010–4. ArticlePubMed
- 5. Keller JM, Sciadini MF, Sinclair E, O’Toole RV. Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma 2012;26:e161–5. PubMed
- 6. Caterino JM, Valasek T, Werman HA. Identification of an age cutoff for increased mortality in patients with elderly trauma. Am J Emerg Med 2010;28:151–8. ArticlePubMed
- 7. Badenes R, Taccone FS. Are you “too old” to survive a traumatic brain injury. Minerva Anestesiol 2017;83:1121–3. ArticlePubMed
- 8. Davidson GH, Hamlat CA, Rivara FP, Koepsell TD, Jurkovich GJ, Arbabi S. Long-term survival of adult trauma patients. JAMA 2011;305:1001–7. ArticlePubMed
- 9. Zhao FZ, Wolf SE, Nakonezny PA, et al. Estimating geriatric mortality after injury using age, injury severity, and performance of a transfusion: the Geriatric Trauma Outcome Score. J Palliat Med 2015;18:677–81. ArticlePubMedPMC
- 10. Park J, Lee Y. Predicting mortality of Korean geriatric trauma patients: a comparison between Geriatric Trauma Outcome Score and Trauma and Injury Severity Score. Yonsei Med J 2022;63:88–94. ArticlePubMedPDF
- 11. Zhuang Y, Feng Q, Tang H, Wang Y, Li Z, Bai X. Predictive value of the Geriatric Trauma Outcome Score in older patients after trauma: a retrospective cohort study. Int J Gen Med 2022;15:4379–90. ArticlePubMedPMCPDF
- 12. Sadro CT, Sandstrom CK, Verma N, Gunn ML. Geriatric trauma: a radiologist’s guide to imaging trauma patients aged 65 years and older. Radiographics 2015;35:1263–85. ArticlePubMed
- 13. Henry SM, Pollak AN, Jones AL, Boswell S, Scalea TM. Pelvic fracture in geriatric patients: a distinct clinical entity. J Trauma 2002;53:15–20. ArticlePubMed
- 14. Kimbrell BJ, Velmahos GC, Chan LS, Demetriades D. Angiographic embolization for pelvic fractures in older patients. Arch Surg 2004;139:728–33. ArticlePubMed
- 15. Cook AC, Joseph B, Inaba K, et al. Multicenter external validation of the Geriatric Trauma Outcome Score: a study by the Prognostic Assessment of Life and Limitations After Trauma in the Elderly (PALLIATE) consortium. J Trauma Acute Care Surg 2016;80:204–9. PubMed
- 16. Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma 1998;45:805–10. PubMed
- 17. van Breugel JM, Niemeyer MJ, Houwert RM, Groenwold RH, Leenen LP, van Wessem KJ. Global changes in mortality rates in polytrauma patients admitted to the ICU: a systematic review. World J Emerg Surg 2020;15:55. ArticlePubMedPMCPDF
- 18. Chang I, Kim H, Shin HJ, Joen WC, Park JM, Shin DW, et al. Factors contributing to mortality for patients at a newly-designated regional trauma center. J Korean Soc Traumatol 2012;25:188–95.
- 19. Mock K, Keeley J, Moazzez A, Plurad DS, Putnam B, Kim DY. Predictors of mortality in trauma patients aged 80 years or older. Am Surg 2016;82:926–9. ArticlePubMedPDF
- 20. Lustenberger T, Inaba K, Schnuriger B, et al. Gunshot injuries in the elderly: patterns and outcomes: a National Trauma Databank analysis. World J Surg 2011;35:528–34. ArticlePubMedPDF
- 21. Bouamra O, Wrotchford A, Hollis S, Vail A, Woodford M, Lecky F. A new approach to outcome prediction in trauma: a comparison with the TRISS model. J Trauma 2006;61:701–10. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Angioembolization performed by trauma surgeons for trauma patients: is it feasible in Korea? A retrospective study
- A decade of treating traumatic sternal fractures in a single-center experience in Korea: a retrospective cohort study
- Determining the appropriate resting energy expenditure requirement for severe trauma patients using indirect calorimetry in Korea: a retrospective observational study
- Epidemiology and clinical characteristics of posttraumatic hospitalized patients with symptoms related to venous thromboembolism: a single-center retrospective study
 KST
KST


 PubReader
PubReader ePub Link
ePub Link Cite
Cite